Abstract
A 28-year-old policeman presented with left lower limb deep vein thrombus, pulmonary embolism and a highly mobile right atrial clot. Thrombolytic therapy with IV Tenecteplase was administered. Within a few minutes after the Tenecteplase bolus, the patient's condition worsened dramatically with severe hypotension and hypoxemia. Immediate bedside transthoracic echocardiogram revealed that the mobile right atrium clot had disappeared completely presumably having migrated to the pulmonary circulation thus worsening the clinical condition. With intensive supportive measures the patient's condition was stabilized and he made a complete recovery. Prior to discharge, the echocardiogram revealed normal right ventricular function and a CT pulmonary angiogram performed after 2 months revealed near complete resolution of pulmonary thrombi. Thrombolytic therapy for right heart thrombus with pulmonary embolism can be a reasonable first line therapy but may be associated with hemodynamic worsening due to clot migration.
Keywords: Embolism, Thrombolysis, Right atrial thrombus
A 28-year-old, physically fit policeman presented with a 3 day history of dyspnea (NYHA IV) and left lower limb swelling of 15 days' duration. Patient had a past history of left lower limb deep vein thrombosis (DVT) 2 years ago for which he was prescribed oral anticoagulant therapy for 6 months. DVT in this patient was idiopathic and unprovoked since a hematologic work-up for hypercoagulable states was negative and also due to the fact that the patient was a physically active young male person. Clinical examination revealed tachycardia (HR-128/min), tachypnea (rate-28/min), blood pressure of 100/70 mmHg, saturation of 92% on room air, an RVS3 with clear lung fields. ECG revealed sinus tachycardia with deep T wave inversion in leads V1–4. Transthoracic Echocardiography (TTE) revealed a dilated right atrium (RA) and right ventricle (RV), severe RV dysfunction and a highly mobile spherical right atrial clot (size 4.84 × 2.21 cm) without any attachments to RA wall that prolapsed through the tricuspid valve with each cycle (Fig. 1A and B and Video 1). CT Pulmonary angiogram (CTPA) revealed massive pulmonary embolism (PE) with clots in both right and left pulmonary arteries as well as within the segmental branches (Fig. 2A and B). Patient was considered to be at high-risk by the cardiothoracic surgeon and hence thrombolysis was considered and an intravenous bolus of 30 mg Tenecteplase was given. Within a few minutes of the Tenecteplase bolus, the patient's condition worsened dramatically. He developed severe hypotension (SBP 60 mmHg) and respiratory distress, profuse sweating and marked desaturation (SaO2 80%). Immediate bedside TTE was performed, which revealed that the mobile RA clot had disappeared completely presumably having migrated to the pulmonary circulation thus worsening the clinical condition (Fig. 1C, Video 2). Intensive supportive measures, including noradrenaline and non-invasive mechanical ventilation were initiated and the heparin infusion was continued. Over the next 24 h, the patient's oxygenation and hemodynamic status improved significantly. Venous Doppler, performed the next day, showed extensive DVT of the left lower limb involving external iliac, superficial femoral and popliteal veins. Due to the large thrombus burden in the lower limb, massive pulmonary embolism and recurrent DVT, an IVC filter (TrapEase Filter, Cordis) was implanted on day 4 (Fig. 1D). Subsequently, oral anticoagulant therapy was initiated overlapped with heparin. Graded compression stocking was advised for the left lower limb. A TTE performed prior to discharge (day 15) revealed normal RV function without TR. Two months later, a repeat CTPA revealed complete resolution of clot in the left pulmonary artery and left segmental arteries, 50% reduction in right pulmonary artery clot and near complete resolution in right segmental arteries with normal RV function and dimensions (Fig. 2C and D). The patient is presently asymptomatic and is being followed up on warfarin.
Fig. 1.
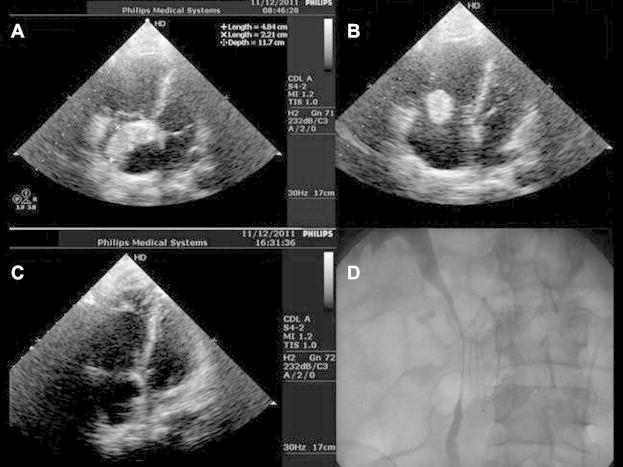
A: Apical Four chamber view demonstrating right atrial thrombus. Right ventricle is dilated. B: The freely mobile right atrial thrombus is seen prolapsing through the tricuspid valve. C: Apical Four chamber view after thrombolytic therapy showing disappearance of right atrial thrombus. D: Inferior vena cava filter.
Fig. 2.
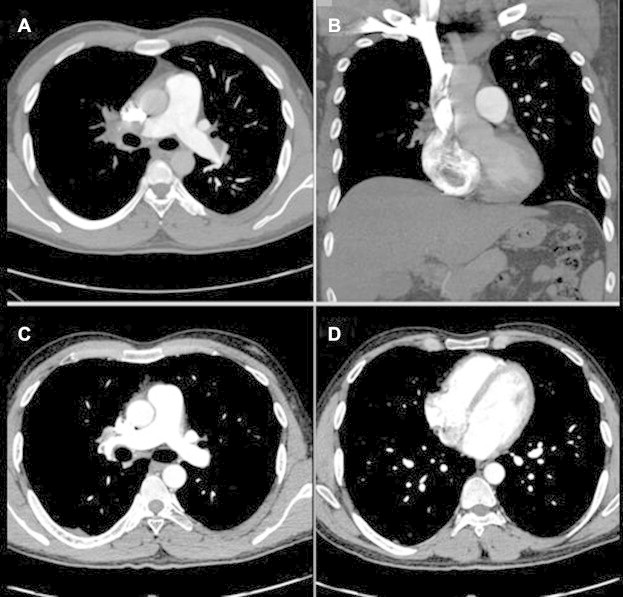
A: CT pulmonary angiogram demonstrating thrombi in right and left pulmonary artery. B: CT Pulmonary angiogram demonstrating thrombus in the right atrium. C: CT Pulmonary angiogram two months after pulmonary embolism demonstrating marked reduction in clot burden. D: CT Pulmonary angiogram two months after pulmonary embolism demonstrating a normal sized right ventricle.
The following are the Supplementary data related to this article:
Video 1Apical Four chamber view demonstrating mobile right atrial thrombus that prolapsed through the tricuspid valve with each cycle. The right ventricle is dilated and shows severe systolic dysfunction.
Video 2Apical Four chamber view after thrombolytic therapy showing disappearance of right atrial thrombus.
Supplementary data related to this article can be found online at http://dx.doi.org/10.1016/j.ihj.2013.06.015.
Mobile right heart thrombus (RHT) with PE constitutes a therapeutic emergency with a mortality of almost 100% in untreated patients and approximately 27.1% among treated patients.1 However, consensus is lacking as to whether surgery or thrombolytic therapy should be the preferred treatment. While right heart exploration with pulmonary embolectomy is the classic treatment, the drawbacks of this approach include lack of availability of surgical expertise, an inherent delay while preparing for surgery, depressant effects of anesthetic drugs and cardioplegia, and the inability to remove co-existing peripheral pulmonary thrombi. On the other hand, thrombolytic therapy is a simple, quick, readily available therapy, which can dissolve the thrombus at different locations (cardiac, pulmonary and peripheral). Two prospective studies have shown mortality rates of 14.2–20.8%.2–4 A meta-analysis of 177 patients with RHT and PE suggested that thrombolytic therapy may be better than surgery (mortality rate 11.3% versus 23.8%).1 Apart from the risk of major bleeding, thrombolytic therapy may be associated with a hypothesized risk of clot fragmentation and migration, complete pulmonary embolization or recurrent PE following partial dissolution of the venous thrombus. The occurrence of such an event in a hemodynamically unstable patient can lead to a catastrophic clinical course with severe hemodynamic compromise. Neither, the two prospective studies of thrombolytic therapy2,3 nor another study with continuous echocardiographic monitoring4 demonstrated hemodynamic worsening during thrombolytic therapy. However, a retrospective study of 38 patients,5 reported worsening of clinical status and cardiac arrest in 9 patients during treatment. Catheter based therapies including aspiration thrombectomy with local delivery of thrombolytic has a restricted role in the management of PE. A recent scientific statement from the American Heart Association (AHA)6 on the management of massive and submassive PE recommends such therapy when systemic fibrinolysis or surgery is contraindicated, not available or has failed to improve the hemodynamics in a given patient. Such a therapy was not warranted in our patient who had a good hemodynamic and anatomic improvement. Such therapies are not without complications, which include life-threatening complications like RA and RV perforation with tamponade. Inferior vena cava (IVC) filters are not routinely indicated in acute PE or in DVT, although their use is justified in recurrent DVT despite therapeutic oral anticoagulation. IVC filters by themselves can contribute to recurrence of DVT (21%), IVC thrombosis (2–10%) and device migration and hence the current recommendation is not use them routinely in PE or DVT.6 The present case demonstrates that TT can be a reasonable first line therapy for RHT with PE but may be associated with hemodynamic worsening due to clot migration.
Funding sources
None
Disclosures
None
Conflicts of interest
All authors have none to declare.
Acknowledgments
None.
References
- 1.Rose P.S., Punjabi N.M., Pearse D.B. Treatment of right heart thromboemboli. Chest. 2002;121:806–814. doi: 10.1378/chest.121.3.806. [DOI] [PubMed] [Google Scholar]
- 2.Torbicki Adam, Galié Nazzareno, Covezzoli Anna. Right heart thrombi in pulmonary embolism: results from the International Cooperative Pulmonary Embolism Registry. J Am Coll Cardiol. 2003;41:2245–2251. doi: 10.1016/s0735-1097(03)00479-0. [DOI] [PubMed] [Google Scholar]
- 3.Pierre-Justin Gilbert, Pierard Luc A. Management of mobile right heart thrombi: a prospective series. Int J Cardiol. 2005;99:381–388. doi: 10.1016/j.ijcard.2003.10.071. [DOI] [PubMed] [Google Scholar]
- 4.Greco F., Bisignani G., Serafini O. Successful treatment of right heart thromboemboli with IV recombinant tissue-type plasminogen activator during continuous echocardiographic monitoring: a case series report. Chest. 1999;116:78–82. doi: 10.1378/chest.116.1.78. [DOI] [PubMed] [Google Scholar]
- 5.Chartier Ludovic, Béra Jerome, Delomez Maxence. Free-floating thrombi in the right heart: diagnosis, management, and prognostic indexes in 38 consecutive patients. Circulation. 1999;99:2779–2783. doi: 10.1161/01.cir.99.21.2779. [DOI] [PubMed] [Google Scholar]
- 6.Jaff Michael R., Sean McMurtry M., Archer Stephen L. Management of massive and submassive pulmonary embolism, Iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension. A scientific statement from the American Heart Association. Circulation. 2011;123:1788–1830. doi: 10.1161/CIR.0b013e318214914f. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video 1Apical Four chamber view demonstrating mobile right atrial thrombus that prolapsed through the tricuspid valve with each cycle. The right ventricle is dilated and shows severe systolic dysfunction.
Video 2Apical Four chamber view after thrombolytic therapy showing disappearance of right atrial thrombus.


