Abstract
Background
Reoperation secondary to surgical site infections can be a devastating complication in orthopaedic surgery. Infection rates in the ambulatory setting have been reported to be lower than those cited in a hospital setting. However, a direct comparative analysis of infection rates of orthopaedic procedures performed in a single specialty ambulatory surgical center (ASC) versus a multi-specialty ASC has, to our knowledge, not been performed.
Methods
Four surgeons performed more than 10,000 orthopaedic surgeries in a multispecialty and single specialty ambulatory setting over 8 years. These procedures were reviewed for postoperative deep infection within one year of initial operation.
Results
The post-surgical deep infection rate in a multi-specialty ASC was 0.81% in 2867 operations compared with a rate of 0.38% in 7311 operations performed in a single specialty ASC (p = 0.007).
Conclusions
This study demonstrated that the rate of infection leading to reoperation was significantly lower in a single specialty ambulatory surgery setting as opposed to one accommodating multiple specialties.
Keywords: Infection, Postoperative, Ambulatory surgical center
1. Introduction
Ambulatory surgical centers (ASCs) in orthopaedics continue to be increasingly utilized. Efficiency, cost, and postoperative outcomes are some of the benefits that have been widely cited. One such postoperative outcome that has been studied with interest is surgical site infection. Prior studies have reported the infection rates in ASCs to be superior to those previously reported in hospital settings.1–4 Comparisons between ASCs servicing multiple specialties as opposed to a single specialty are more elusive. With teams dedicated to the care of patients undergoing a defined set of procedures and facilities designed with these procedures in mind, the benefits of an ASC are maximized in this setting. Whether these dedicated facilities and teams yield better outcomes, specifically a lower infection rate, is unclear.
Prior to April 1, 2004, all outpatient orthopaedic operations performed at Emory were performed in a facility that was utilized for outpatient procedures in Plastic Surgery, Otolaryngology, Ophthalmology, and Orthopaedic Surgery. In 2004, an ASC devoted to Orthopaedic Surgery, Emory Orthopaedic and Spine Center at Executive Park, became the chief facility at which these outpatient operations were performed. After that date, the four orthopaedic surgeons included in this study utilized this center exclusively for their operations previously performed at the multispecialty outpatient facility.
We sought to directly compare the reoperation rate secondary to infection in outpatient orthopaedic procedures performed by the same group of surgeons over 8 years at a single specialty and multispecialty outpatient facility to further explore the relationship between rate of infection and setting in which the operation is performed.
2. Patients and methods
We performed a retrospective chart review of 9012 consecutive patients who underwent total of 10,178 outpatient surgical procedures by one of four orthopaedic surgeons during one of two time periods in this study. The surgeons in this study included one upper extremity surgeon, a foot and ankle surgeon, and two sports medicine surgeons. Each surgeon had greater than 3 years operative experience and is fellowship trained in their respective subspecialties. We first identified all patients undergoing more than one orthopaedic operation at any institutional facility between January 1, 2001 and April 1, 2004. Similarly, we then identified those undergoing re-operation between April 17, 2007 and February 28, 2011. These dates were chosen based on the method of procedure reporting during these time courses. We also investigated the infection rates and case distribution during these dates based on their respective subspecialty (Hand, Foot/Ankle, and Sports).
Those patients who returned to any institutional facility with an infection and subsequent reoperation were included in this study. The determination of surgical site infection was in accordance with the CDC definition and included those who tested positive on lab cultures, had purulent drainage, or were deemed to have an infection by an attending surgeon. In addition, the infection was determined to be a surgical site infection if it occurred within 30 days after the operation if no implant was left in place and within one year if an implant was left in place. Patients were excluded if there was evidence of infection prior to the initial operation or if their initial operation was not performed in one of the two studied facilities.
There have been many variables associated with perioperative infections. This study is unique in controlling for many of these variables, such as patient preparation, patient comorbidities, and surgeon technique. The preparation was routinely an alcohol scrub followed by a Betadine prep. This was true for the entirety of the dates listed; only after the completed study dates did our institution begin using a chlorhexidine prep. Perioperative antibiotic and postoperative dressing protocols were consistent among individual surgeons across the time frames. The two facilities, although not adjacent to each other, both had laminar flow rooms with similar designs.
To assess and compare comorbidities between the two cohorts, we reviewed the comorbid conditions of 50 randomly selected patients from each cohort. We assigned each patient a number based on the number of comorbid conditions from zero to three, with three including those patients with three or more comorbid conditions. Comorbidities included in this analysis and their frequencies are listed in Table 1.
Table 1.
Microbiology of postoperative infections.
| Organism | Multispecialty | Single specialty |
|---|---|---|
| MSSA | 10 | 8 |
| MRSA | 3 | 5 |
| Staphylococcus epidermidis | 4 | 3 |
| Propionibacterium acnes | 1 | 2 |
| Staphylococcus lugdunensis | 0 | 2 |
| Streptococcus spp. | 1 | 2 |
| Enterococcus fecalis | 0 | 1 |
| Anaerobics | 0 | 1 |
| Serratia marcescens | 0 | 1 |
| Corynebacterium spp. | 0 | 1 |
Data analysis was made using chi-squared test with a level of significance set at a p-value of less than 0.05. Analysis was made using JMP software (SAS Institute Inc., North Carolina).
3. Results
Over the period 2001–2004, 2867 operations were performed at the multispecialty ASC and we identified 23 deep infections, yielding a rate of 0.81%. Over the period 2007–2011, 7311 operations were performed at Executive Park with 28 total cases of deep infection, giving a rate of 0.38% (Fig. 1). A chi-squared test demonstrated a level of statistical significance with a p-value of 0.007. The infection rates of each subspecialty during both time periods are in Fig. 2.
Fig. 1.
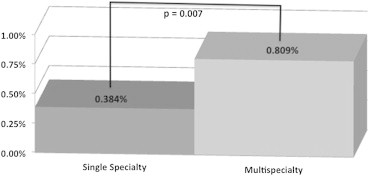
Infection rates of facilities.
Fig. 2.
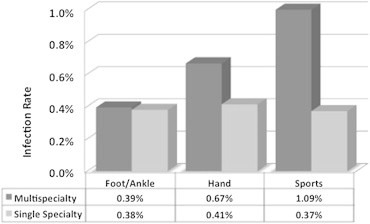
Infection rates distribution.
The distribution of cases over this time was similar. Foot and Ankle cases comprised 17.8% of the orthopaedic procedures performed from 2001 to 2004 and 21.7% of the procedures from 2007 to 2011. Hand cases comprised 36.9% vs. 26.5% and sports cases comprised 45.3.0% vs. 51.8%, respectively (Fig. 3).
Fig. 3.
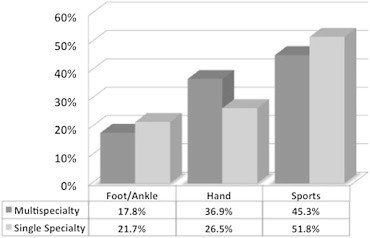
Case distribution.
The patient characteristics of the groups selected from each time period were not significantly different. Between the multispecialty and single specialty facility patients, there was not a statistically significant difference in the number of comorbidities per patient (Table 1).
The microbiology of the infections is listed in Table 2. There was no statistically significant difference in the distribution of microorganisms between the two time periods.
Table 2.
Distribution of comorbidities.
| # Of comorbidities | Multispecialty | Single specialty |
|---|---|---|
| 0 | 30(0.6) | 29(0.58) |
| 1 | 14(0.28) | 13(0.26) |
| 2 | 5(0.1) | 7(0.14) |
| 3 | 1(0.02) | 1(0.02) |
| Comorbidities identified | Hypertension (18), Thyroid abnormalities (9), Coronary Artery Disease (6), Diabetes Mellitus (5), Asthma (4), History of Cancer (3), Heart Arrhythmia (3), Congestive Heart Failure (2), Rheumatoid Arthritis (2), Anemia (2), Seizure disorder (1), Chronic steroid use (1) | |
4. Discussion
Surgical site infections in orthopaedic procedures have been shown to increase cost, prolong hospitalization, and decrease health-related quality of life.5,6 In addition, SSI rates are frequently used as a method for comparison among institutions and serve as a measure to promote quality improvement. Factors influencing the rate of SSI have been extensively studied and reported with both modifiable patient risk factors (smoking, diabetes, obesity, immunosuppression, etc.) and institutional factors (antimicrobial prophylaxis, UV light, hand scrubbing, hair shaving, surgical duration, etc.).7,8 Surgical site infection rates are frequently cited as a benefit to ASCs, but a comparison between single specialty and multi-specialty settings has not been performed.1–4 Indirect comparison of ASC rates is problematic as a number of confounding variables can prevent reliable comparisons. Differences between institutions in infection prevention and recording, different surgeons with different case distributions, and variable specialty distribution prevent reliable contrasts. We attempted to eliminate these variables by using a standard method of identifying infections in a cohort undergoing procedures in one group of orthopaedic surgeons over an 8-year period.
A limitation of this study includes its retrospective nature. While the records from all institutional hospitals were reviewed in search of eligible subjects, it is possible a small subset of patients did not follow up at a university-associated facility. By using a large sample size, we attempted to equivocate this subset between the two groups and yield a matched and accurate comparison.
The incidence of infection in clean orthopaedic surgery has been reported to be 0.5%–6.5%.9 A study of a similar cohort in an orthopaedic ASC was shown to be as low as 0.33%.1 Our study is consistent with these results, demonstrating a rate of 0.38% in the 7311 cases performed at Executive Park. This rate shows a reduction of infection leading to reoperation by more than half when compared with the results of outpatient procedures performed by the same group of surgeons at a multispecialty facility.
We also classified cases based on type of operation to evaluate the distribution between foot and ankle, hand, and sports operations. It has been previously established that procedures involving the foot and ankle are associated with high rates of infection and increased difficulty in eliminating bacteria of the forefoot prior to surgery.10–13 In our sample, we found a small difference (17.8% vs. 21.7%) in the proportion of foot and ankle cases performed between the two samples with a great proportion of foot and ankle cases being performed in the time period 2007–2011. While the cases between the two time periods did not show an identical distribution, it is important to note that of the set of procedures shown to have a higher infection rate are more highly represented during the time period spent operating at the single specialty facility.
This study is unique in that it provides direct comparison of infection rates in two different settings with the same group of surgeons and procedures. Indirect comparisons of infection rates are problematic due to varied reporting methods for infection, unequal procedure distributions among facilities, and institutional differences in the prevention of infection in the pre-, intra-, and post-operative settings. We controlled for these factors by using a consistent method of retrieving cases of infection in a cohort of patients undergoing operation by the same group of surgeons over an 8-year period. This study is distinctive in the fact that it maintains the same four surgeons, the same preoperative and postoperative protocols, and similar patient cohorts undergoing a similar distribution of outpatient procedures over an extended time period.
This study suggests that among the many factors which impact surgical site infection, the setting in which the operation takes place is another consideration which can be controlled by the surgeon to give the most optimal post-operative course and result.
Conflicts of interest
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article with the exception of Dr. John Xerogeanes. Dr. Xerogeanes is a paid speaker for Linvatech but did not receive any associated financial payments related to this article. This author's department receives money from Linvatech, Arthrex, DJO, and Smith and Nephew for Fellowship Research and Teaching.
Footnotes
The Emory IRB approved this study for retrospective review.
References
- 1.Edmonston D.L., Foulkes G.D. Infection rate and risk factor analysis in an orthopaedic ambulatory surgical center. J Surg Orthop Adv. 2010 Fall;19:174–176. [PubMed] [Google Scholar]
- 2.Gastmeier P., Sohr D., Brandt C. Reduction of orthopedic wound infections in 21 hospitals. Arch Orthop Trauma Surg. 2005;125:526–530. doi: 10.1007/s00402-005-0036-y. [DOI] [PubMed] [Google Scholar]
- 3.Majholm B., Engbaek J., Bartholdy J. Is day surgery safe? A Danish multicenter study of morbidity after 57,709 day surgery procedures. Acta Anaesthesiol Scand. 2012 Mar;56:323–331. doi: 10.1111/j.1399-6576.2011.02631.x. [DOI] [PubMed] [Google Scholar]
- 4.Maksimovic J., Markovic-Denic L., Bumbasirevic M. Surgical site infections in orthopedic patients: prospective cohort study. Croat Med J. 2008;49:58–65. doi: 10.3325/cmj.2008.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Lissovoy G., Fraeman K., Hutchins V. Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control. 2009 Jun;37:387–397. doi: 10.1016/j.ajic.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 6.Whitehouse J.D., Friedman N.D., Kirkland K.B. The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol. 2002;23:183–189. doi: 10.1086/502033. [DOI] [PubMed] [Google Scholar]
- 7.Harrop J.S., Styliaras J.C., Ooi Y.C. Contributing factors to surgical site infections. J Am Acad Orthop Surg. 2012 Feb;20:94–101. doi: 10.5435/JAAOS-20-02-094. [DOI] [PubMed] [Google Scholar]
- 8.The American Academy of Orthopaedic Surgeons Patient Safety Committee. Evans R.P. Surgical site infection prevention and control: an emerging paradigm. J Bone Jt Surg Am. 2009;91:2–9. doi: 10.2106/JBJS.I.00549. [DOI] [PubMed] [Google Scholar]
- 9.Zgonis T., Jolly G.P., Garbalosa J.C. The efficacy of prophylactic intravenous antibiotics in elective foot and ankle surgery. J Foot Ankle Surg. 2004 Mar-Apr;43:97–103. doi: 10.1053/j.jfas.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 10.Brooks R.A., Hollinghurst D., Ribbans W.J., Severn M. Bacterial recolonization during foot surgery: a prospective randomized study of toe preparation techniques. Foot Ankle Int. 2001;22:347–350. doi: 10.1177/107110070102200415. [DOI] [PubMed] [Google Scholar]
- 11.Ostrander R., Brage M., Botte M. Bacterial skin contamination after surgical preparation in foot and ankle surgery. Clin Orthop. 2003;406:246–252. doi: 10.1097/01.blo.0000030176.56585.d3. [DOI] [PubMed] [Google Scholar]
- 12.Taylor G., Bannister G., Calder S. Perioperative wound infection in elective orthopaedic surgery. J Hosp Infect. 1990 Oct;16:241–247. doi: 10.1016/0195-6701(90)90112-2. [DOI] [PubMed] [Google Scholar]
- 13.Zacharias J., Largen P., Crosby L. Results of preprocedure and postprocedure toe cultures in orthopedic surgery. Foot Ankle Int. 1998;19:166–168. doi: 10.1177/107110079801900310. [DOI] [PubMed] [Google Scholar]


