Abstract
The purpose of this review was to inform all medical health care professionals about cuboid syndrome, which has been described as difficult to recognize and is commonly misdiagnosed, by explaining the etiology of this syndrome, its clinical diagnosis in relation to differential diagnoses, commonly administered treatment techniques, and patient outcomes. A comprehensive review of the relevant literature was conducted with MEDLINE, EBSCO, and PubMed (1960 - Present) using the key words cuboid, cuboid syndrome, foot anatomy, tarsal bones, manual therapy, and manipulation. Medical professionals must be aware that any lateral foot and ankle pain may be the result of cuboid syndrome. Once properly diagnosed, cuboid syndrome responds exceptionally well to conservative treatment involving specific cuboid manipulation techniques. Other methods of conservative treatment including therapeutic modalities, therapeutic exercises, padding, and low dye taping techniques are used as adjuncts in the treatment of this syndrome. Immediately after the manipulation is performed, the patient may note a decrease or a complete cessation of their symptoms. Occasionally, if the patient has had symptoms for a longer duration, several manipulations may be warranted throughout the course of time. Due to the fact radiographic imaging is of little value, the diagnosis is largely based on the patient’s history and a collection of signs and symptoms associated with the condition. Additionally, an understanding of the etiology behind this syndrome is essential, aiding the clinician in the diagnosis and treatment of this syndrome. After the correct diagnosis is made and a proper treatment regimen is utilized, the prognosis is excellent.
Key Points.
Define the poorly understood condition of cuboid syndrome.
Provide an understanding of the anatomical structures involved.
Provide an explanation as to the cause of this syndrome.
Demonstrate ways to evaluate by making a differential diagnosis.
To inform health care professionals about management and treatment of cuboid syndrome.
Key words: Subluxation, manipulation, tarsal, syndrome, manual therapy
Introduction
Cuboid syndrome has also been referred to in the literature as subluxed cuboid, locked cuboid, dropped cuboid, cuboid fault syndrome, lateral plantar neuritis, and peroneal cuboid syndrome (Gamble and Yale, 1975; Jones, 1973; Main and Jowett, 1975; McDonough and Ganley, 1973; Newell and Woodle, 1981; Subotnick, 1989). Because of the nature and inconsistent terminology associated with this injury, cuboid syndrome remains a poorly understood condition in both athletic and non-athletic populations (Blakeslee and Morris, 1987). Therefore, cuboid syndrome is an often mistreated and misdiagnosed condition (Blakeslee and Morris, 1987). Cuboid syndrome is defined as a minor disruption or subluxation of the structural congruity of the calcaneocuboid portion of the midtarsal joint. The disruption of the cuboid’s position irritates the surrounding joint capsule, ligaments, and peroneus longus tendon (Blakeslee and Morris, 1987).
Newell and Woodle, 1981 have reported that as many as 4% of athletes with foot injuries present with cuboid syndrome. Although, Jennings and Davies, 2005, who specialized in the examination and treatment of this syndrome, found 6.7% of their patients who presented with a plantar flexion and inversion ankle sprain were further diagnosed with cuboid syndrome. However, the manifestation of cuboid syndrome appears much higher in certain sports. In professional ballet dancers, for example, cuboid syndrome may account for 17% of all reported foot and ankle injuries (Marshall and Hamilton, 1992). Furthermore, cuboid syndrome in male ballet dancers was generally acute in nature occurring as a result of a series of repetitive jumps where the foot continuously pronates abruptly (Marshall and Hamilton, 1992). While in the female ballet dancer, cuboid syndrome was experienced as an overuse syndrome, resulting from multiple microtraumas to the ligamentous structures during maneuvers requiring maximum flexibility (Marshall and Hamilton, 1992). Cuboid syndrome has also been noted as a complication of a plantar flexion and inversion ankle injury (Jennings and Davies, 2005). Inversion ankle sprains are one of the most common athletic injuries, accounting for between 38% and 45% of all injuries (Fallat et al., 1998). Up to 40% of these patients may have residual symptoms, cuboid syndrome being a possible culprit (Freeman, 1965).
Medical professionals should possess the ability to correctly and accurately diagnose these injuries with the aim of providing appropriate treatment to facilitate a functional return to activity. Therefore, the purpose of this article was to review the literature and provide an in depth portrayal of cuboid syndrome, its clinical diagnosis in relation to differential diagnoses, common treatment techniques, and patient outcomes.
Anatomical Considerations
Understanding the anatomy of the foot is crucial for an accurate diagnosis of cuboid syndrome. The foot is comprised of 26 bones. The cuboid is unique for the simple fact it is the only bone in the foot that articulates with both the tarsometatarsal joint (Lisfranc complex) and the midtarsal joint (Chopart’s Joint), and is the only bone linking the lateral column to the transverse plantar arch (Kolker et al., 2002). Consequently, the cuboid acts as a keystone of the rigid and static lateral column giving inherent stability to the foot (Kolker et al., 2002).
The cuboid is secured in the lateral column by numerous ligaments, specifically the dorsal and plantar calcaneocuboid, dorsal and plantar cuboideonavicular, dorsal and plantar cuboideometatarsal, and the long plantar ligament (Figure 1) (Draves, 1986; Resnick and Niwayama, 1985; Sarrafian, 1983; Van Langelaan, 1983). These ligaments are more taut dorsomedially than plantar laterally. Therefore, the calcaneocuboid joint will rotate around a medially positioned axis (Huson, 1965).
Figure 1.
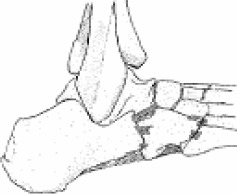
The dorsal and plantar ligaments of the cuboid and its articulations.
The calcaneocuboid and talonavicular joints function together about their respective axes to create the midtarsal joint or Chopart’s joint (Blakeslee and Morris, 1987). The shape and position of the cuboid is also influenced by an extrinsic muscle tendon, the peroneus longus (Blakeslee and Morris, 1987). This muscle originates on the upper one-third of the fibula. It then travels distally down the shaft of the fibula and posteriorly around the lateral malleolus continuing to travel in a plantar lateral direction until the tendon reaches the cuboid. Here the path of the tendon then changes directions and travels anteromedially through the cuboid’s peroneal groove and inserts on the lateral base of first metatarsal and first cuneiform.
Normal Characteristics and Mechanics of the Foot
A thorough knowledge of the foot’s structure and alignment is essential before evaluating injuries, especially overuse injuries. In addition to “normal ”foot structure, normal motion must occur at the articulations within the foot. Discussing all of these motions is beyond the scope of this review, but understanding the normal physiological motion that is permitted at the cuboid articulations is essential to the diagnosis and treatment of cuboid syndrome (Mooney and Maffey-Ward, 1994). The cuboid articulations provide accessory glide along with internal and external rotation (Magee, 1987). The passive physiological motion of the lateral column consists of two patterns of movement. The first combined movement is plantar flexion and adduction along with inversion (Mooney and Maffey-Ward, 1994). The second movement pattern consists of dorsiflexion and abduction with eversion (Mooney and Maffey-Ward, 1994). These combinational movement patterns are more commonly referred to as supination and pronation, respectively. The midtarsal joint consists of two unique axes, the oblique and the longitudinal (Figure 2). Motion about these axes may occur independently from each other, but both are dependant upon the subtalar joint’s position. When the midtarsal joint is fully pronated around both the oblique and longitudinal axes, the midtarsal joint is said to be in its “locked ”position (Root et al., 1977). The relationship between the forefoot and rearfoot is dependant on the position of the subtalar joint. When the subtalar joint is pronated, the forefoot is inverted relative to the rearfoot and the midtarsal joint is unlocked, enabling the foot to adapt to uneven surfaces and act as a shock absorber at ground contact. The supination that occurs at the subtalar joint decreases both supination and pronation at the midtarsal joint thus creating a more stable midfoot during the propulsive phase of gait (Blakeslee and Morris, 1987). Every degree of subtalar pronation that occurs produces an exponential increase in midtarsal joint instability (Blakeslee and Morris, 1987). Biomechanically, the line of pull the intrinsic musculature exerts plays an important role in the dynamic stabilization of the midtarsal joint (Mann and Inman, 1964).
Figure 2.
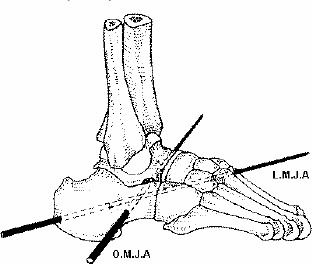
The oblique (O.M.J.A.) and longitudinal (L.M.J.A.) axes of the midtarsal joint as viewed laterally.
Etiology
There are several proposed etiologies that may result in cuboid syndrome. Among these mechanisms, the two that are most consistent throughout the literature are plantar flexion and inversion ankle sprains and an overuse syndrome. Furthermore, plantar flexion and inversion injuries account for the majority of cases, while the overuse syndrome is seldom described (Blakeslee and Morris, 1987; Jennings and Davies, 2005; Khan et al., 1995; Marshall and Hamilton, 1992; Mooney and Maffey-Ward, 1994; Newell and Woodle, 1981; Subotnick, 1989). Some authors have also proposed there are several predisposing factors which have also been associated with the likely occurrence of this syndrome. Factors including, improperly constructed orthoses, uneven running terrain, faulty shoe construction, inversion ankle injuries, and pronated foot structure (Newell and Woodle, 1981; Parks, 1983). However, these factors may increase the likelihood of cuboid syndrome, but are not direct mechanism of injury.
The degree and direction of the force of the peroneus longus and the position of the subtalar joint are thought of as contributing factors in the etiology of cuboid syndrome (Newell and Woodle, 1981). Peroneus longus is a stance phase muscle, contracting midway through the midstance phase and continuing to contract through the late propulsive phase (Root et al., 1977). In a foot that is supinating at the subtalar joint during propulsion, it acts as a dynamic stabilizer of the forefoot as it assists in plantar flexion of the first ray while using the cuboid as a pulley, increasing the mechanical advantage of the peroneus longus (Blakeslee and Morris, 1987). Although, if the subtalar joint is pronating during early propulsion, the soleus muscle relaxes while the peroneus longus lifts the lateral foot which becomes unstable and which may cause a disruption of the cuboid (Root et al., 1977). A pronated foot structure, which Newell and Woodle, 1981 found in 80% of their patients, creates a naturally unstable and hypermobile foot further increasing the mechanical advantage of the peroneus longus. The increase in mechanical advantage is theoretically able to sublux the pronated, unstable cuboid, as the rearfoot resupinates into propulsion (Blakeslee and Morris, 1987). Furthermore, a pronated foot in conjunction with a plantar flexed lateral column may also overwhelm the soft tissues surrounding the cuboid due to the excessive lateral midfoot pressure (Subotnick, 1989). It has also been documented that the pronated foot, a combination of dorsiflexion, abduction, and eversion, requires greater intrinsic muscle activity to stabilize the midtarsal joint than that of the “normal ”foot (Mann and Inman, 1964). However, Marshall and Hamilton, 1992 did not find this pronated foot structure to be true of their patients, but found this syndrome occurred in all types of foot structures, including a pes cavus foot. A pes cavus foot structure is still able to pronate in relation to the hindfoot which may also increase the incidence of cuboid syndrome (Marshall and Hamilton, 1992). Others have noted cuboid syndrome may also occur in those who present with a pes cavus foot and an anterior equines deformity with a plantar flexed lateral column causing them to walk in a more supinated position placing excess lateral pressure on the midfoot (Subotnick, 1989).
However, the increased mechanical advantage of the peroneus longus is only part of the etiologic mechanism. The other part believed to be involved is the anatomical relationship between the calcaneus and cuboid which predisposes certain individuals to this syndrome (Blakeslee and Morris, 1987). The articulation between the calcaneus and cuboid influences the locking mechanism of the midtarsal joint. These two structures must be in maximal congruency if the midtarsal joint’s locking mechanism is to function properly by preventing excessive pronation (Blakeslee and Morris, 1987). If the calcaneocuboid joint is not completely congruous, the excessive ground reaction forces occurring during the propulsive phase of gait overwhelm the soft tissues surrounding the cuboid, predominantly the joint capsule and ligaments that secure the cuboid in the lateral column, theoretically leading to varying degrees of subluxation or cuboid displacement (Blakeslee and Morris, 1987).
Another cause of cuboid syndrome results secondary to plantar flexion and inversion ankle sprains (Freeman, 1965; Jennings and Davies, 2005; Mooney and Maffey-Ward, 1994; Subotnick, 1989). Plantar flexion and inversion ankle sprains are relatively common with an incidence rate of 1 per 10,000 persons per day (Fallat et al., 1998). As the foot and ankle are placed into plantar flexion and inversion, the peroneus longus tendon places a dorsal and lateral force on the forefoot, creating a close packed position and forcing the cuboid in an inferomedial direction tearing the interosseous ligaments (Caselli and Pantelaras, 2004). Therefore, the actual acute trauma is thought to be responsible for the disruption of the cuboid’s position (Jennings and Davies, 2005). The stretch reflex is another theory, regarding plantar flexion and inversion ankle sprains (Blakeslee and Morris, 1987; Caselli and Pantelaras, 2004). When the foot and ankle are forced rapidly into plantar flexion and inversion, there is a reflex contraction of the peroneus longus muscle attempting to get the foot medial to the ground (Blakeslee and Morris, 1987; Caselli and Pantelaras, 2004). During the forceful contraction of the peroneus longus the cuboid is used as a fulcrum to increase the mechanical advantage causing a medial rotation (Caselli and Pantelaras, 2004). The peroneus longus, once again, exerts a dorsal and lateral force on the cuboid hypothetically resulting in inferomedial displacement of the cuboid (Caselli and Pantelaras, 2004). More specifically, the pathomechanics of cuboid syndrome may stem from an eversion of the cuboid from an inverted foot position, such as the mechanism of injury for a lateral ankle sprain (Jennings and Davies, 2005; Subotnick, 1989).
Less commonly suggested etiologies also exist for the secondary occurrence of cuboid syndrome following heel spur surgery as well as the improper construction of orthoses (Subotnick, 1989).
Physical Examination
Subjective
Patients will typically present with pain that developed rapidly or that gradually occurred overtime as a sequalae to an inversion ankle sprain or small microtraumas overwhelming the ligaments and joint capsule of the lateral column (Blakeslee and Morris, 1987; Caselli and Pantelaras, 2004; Jennings and Davies, 2005; Marhsall and Hamilton, 1992). Patients will describe pain that is located directly over the cuboid (Jennings and Davies, 2005). Pain may also radiate into the plantar medial arch or distally along the fourth metatarsal (Marshall and Hamilton, 1992). Patients may also complain of pain during normal weight-bearing or even during non-weight-bearing. Weakness, secondary to pain, during toe-off of the propulsive phase of the gait cycle is also a complaint associated with cuboid syndrome (Blakeslee and Morris, 1987; Marshall and Hamilton, 1992).
Objective
Upon observation of the lateral foot and surrounding structures, swelling, redness, and ecchymosis may be present (Marshall and Hamilton, 1992; Newell and Woodle, 1981). If the subluxation is severe enough, and a plantar subluxation occurs, a slight sulcus may be visible over the dorsum of the cuboid and a lump on the plantar surface (Mooney and Maffey-Ward, 1994). Occasionally, the patient may also present with a subtle forefoot valgus (Khan et al., 1995).
Pain and point tenderness is elicited directly over the cuboid (Figure 3), as well as on the plantar aspect of the foot, during palpation (Blakeslee and Morris, 1987; Jennings and Davies, 2005). Tenderness may also be elicited when palpating the origin of the extensor digitorum brevis muscle, located on the anterolateral surface of the calcaneus in the sinus tarsi, and in the region of the peroneal grove (Blakeslee and Morris, 1987). However, if pain is located predominantly over the calcaneocuboid joint, cuboid-fifth metatarsal articulations, or fourth and fifth metatarsal articulations an alternative diagnosis may be the case (Marshall and Hamilton, 1992). Palpation may also reveal warmth and a slight edematous feel, which is dependant on the amount of swelling in the area (Starkey and Ryan, 2002).
Figure 3.

Palpation directly over the dorsolateral aspect of the cuboid bone will elicit pain in cuboid syndrome. This aspect of the cuboid can be palpated just proximal to the styloid process of the 5th metatarsal and distally of the peroneal tubercle of the calcaneus.
Normal active and passive range of motion at the foot and ankle may be decreased when compared bilaterally (Marshall and Hamilton, 1992; Mooney and Maffey-Ward, 1994). Pain may be elicited during passive inversion and also during active and resistive plantar flexion and eversion (Blakeslee and Morris, 1987; Mooney and Maffey-Ward, 1994; Newell and Woodle, 1981). Resisted inversion, resulting in pain along the peroneus longus as it passes underneath the cuboid, has also been documented as diagnostic procedure used in the evaluation of cuboid syndrome (Subotnick, 1989).
While one specific special test does not exist to diagnose cuboid syndrome, several may be useful in the evaluation process. The tarsometatarsal and midtarsal glide tests may be beneficial (Marshall and Hamilton, 1992). However, it must be noted these tests offer only fair reliability. Since pain is the primary limiting factor in this syndrome, the clinician may not be able to accurately assess mobility due to guarding of the patient and testing for hypermobility versus hypomobility does not provide any additional information aiding in the diagnosis (Jennings and Davies, 2005). Therefore, a positive test is indicated by pain or reproduction of the patient’s symptoms (Marshall and Hamilton, 1992). Testing the midtarsal joint, using the midtarsal adduction test (Figure 4) and the midtarsal supination test (Figure 5) may also replicate the patient’s symptoms as well (Blakeslee and Morris, 1987; Jennings and Davies, 2005). In addition, Jennings and Davies, 2005 have stated pronation and abduction, which compress the structures involved in this syndrome, may occasionally provoke the patient’s symptoms. Gait evaluation and functional testing are beneficial and should also be performed with patients who present with cuboid syndrome symptoms as a reproduction in the patient’s symptoms may be noted (Jennings and Davies, 2005). All of the previously mentioned tests were documented in the literature and will aid the clinician in accurately diagnosing cuboid syndrome. However, other, more commonly, administered special tests are not to be neglected as they are required for a differential diagnosis.
Figure 4.

Midtarsal Adduction Test. To perform this test, the clinician stabilizes the ankle and the subtalar joint with the right (proximal) hand, while the left (distal) hand applies the adduction force (arrow).
Figure 5.

Midtarsal Supination Test. To perform this test, the clinician stabilizes the subtalar joint and ankle with the right (proximal) hand, while the left (distal) hand applies the supination motion (inversion, plantar flexion, and forefoot adduction).
The diagnosis of cuboid syndrome can not be made through the use of X-rays, computerized tomography (CT), or magnetic resonance imaging (MRI). The disruption or subluxation is believed to be so minor that radiological or other imaging studies are of little value in the diagnosis of cuboid syndrome (Blakeslee and Morris, 1987; Marshall and Hamilton, 1992; Mooney and Maffey-Ward, 1994; Newell and Woodle, 1981). The changes are often unnoticeable or, in the acute case, the cuboid is thought to have already returned to its normal position and no deformity or incongruity exists when the images are acquired (Blakeslee and Morris, 1987). Therefore, the diagnosis of cuboid syndrome is based on the patient’s history and findings during the physical examination (Blakeslee and Morris, 1987; Jennings and Davies, 2005). Nonetheless, radiographic imaging should initially be used to rule out any fracture, tumor, or other pathology (Jennings and Davies, 2005).
Differential Diagnosis
Cuboid syndrome often presents with subtle symptoms producing pain over the lateral column of the foot. These symptoms may emulate those of other pathologies. Therefore, a differential diagnosis between several other pathologies is a key element in the accurate diagnosis of cuboid syndrome. This syndrome should not be confused with more serious injuries associated with the cuboid, such as a severe subluxation, dislocation, or fracture. Furthermore, one should also not confuse this syndrome with other injuries presenting with signs and symptoms on the lateral aspect of the foot. These similar injuries include: Jones fracture, fracture of the anterior calcaneal process, tarsal coalition, peroneal and extensor digitorum brevis tendonitis, subluxing peroneal tendons, sinus tarsi syndrome, lateral plantar nerve entrapment, Lisfranc injuries, stress fractures of the cuboid, meniscoid of the ankle, and malalignment of the lateral ankle and subtalar joints (Caselli and Pantelaras, 2004; Dewar and Evans, 1968; Jennings and Davies, 2005; Main and Jowett, 1975; Phillips, 1985; Leerar, 2001).
Treatment
Cuboid syndrome responds exceptionally well to conservative treatment. The primary method of treatment is the cuboid manipulation. Other methods of conservative treatment including various therapeutic modalities, therapeutic exercise, low dye arch taping, and padding are adjuncts to the cuboid manipulation techniques (Blakeslee and Morris, 1987; Jennings and Davies, 2005; Marshall and Hamilton, 1992; Newell and Woodle, 1981). Immediately after the cuboid has been manipulated the patient may report a markedly decrease or a complete cessation of symptoms (Blakeslee and Morris, 1987; Marshall and Hamilton, 1992; Mooney and Maffey-Ward, 1994; Newell and Woodle, 1981).
The original manipulation technique for plantar subluxations as described by Newell and Woodle, 1981 is termed the “black snake heel whip ”or “cuboid whip”. This technique has since been modified by others and may be performed either with the patient standing with the knee flexed to 90 degrees or lying in a prone position with the knee flexed to approximately 70 degrees (Blakeslee and Morris, 1987; Newell and Woodle, 1981). The clinician must position the patient’s knee in flexion to reduce the stress of the gastrocnemius and also to avoid stretching the superficial peroneal nerve (Newell and Woodle, 1981). The manipulation is performed by interlocking the fingers over the dorsum of the foot, while the thumbs are positioned on the plantar aspect of the cuboid. With the knee in 70-90 degrees of flexion and the ankle in zero degrees of dorsiflexion, the manipulation is performed by extending the knee and plantar flexing the ankle with slight supination of the subtalar joint (Figure 6a, 6b and 6c) (Blakeslee and Morris, 1987; Jennings and Davies, 2005; Newell and Woodle, 1981). The “cuboid whip ”works well for cuboid syndrome that has occurred secondary to plantar flexion and inversion ankle injury (Jennings and Davies, 2005). The original cuboid manipulation technique was later adapted to the “cuboid squeeze ”by Marshall and Hamilton, 1992 because any “whipping ”of the foot should be avoided due to the amount of force transmitted to the talocrural joint. Furthermore, Marshall and Hamilton, 1992 stated the “cuboid squeeze ”offered the clinician better control and direction of the manipulation force. This technique differs slightly from the “cuboid whip. ”The clinician gradually places the foot and ankle into maximal plantar flexion, as the soft tissues relax the cuboid is squeezed with the thumbs (Marshall and Hamilton, 1992). Traditionally, it has been documented in the literature that the “cuboid squeeze ”is better suited for the cuboid syndrome which has occurred secondary to an overuse syndrome (Marshall and Hamilton, 1992). As the cuboid manipulation occurs there is often an audible ‘pop’ or ‘snap’ heard by the patient or clinician (Blakeslee and Morris, 1987; Marshall and Hamilton, 1992). However, this does not signify a successful manipulation (Jennings and Davies, 2005).
Figure 6a.

"Cuboid Whip ”Manipulation. The manipulation is performed with the patient in the prone position, starting with the knee flexed to 70° - 90° and the ankle near neutral.
Theoretically, the cuboid manipulation is thought to realign the disruption of the calcaneocuboid joint (Marshall and Hamilton, 1992; Newell and Woodle, 1981). The realignment of this joint is only speculative and the theory yet to be confirmed (Jennings and Davies, 2005). However, the cuboid manipulation may still alter the stresses on the bony and soft tissues that surround the cuboid (Maigne and Vautravers, 2003). Manipulation done to other areas in the body has shown to provide an analgesic effect which was most likely due to the gate theory of pain as well as the elevation in plasma beta endorphin levels (Melzack and Wall, 1965; Vernon et al., 1986). As with all treatments, the placebo effect is thought to also play some role in the success of the cuboid manipulation (Maigne and Vautravers, 2003; Turner et al., 1994).
There are several contraindications regarding the use of a cuboid manipulation including, neoplastic or bone disease, inflammatory arthritis, gout, and neural or vascular disorders (Caselli and Pantelaras, 2004). Some author’s have also found it necessary to attempt to relax the, often spastic, peroneal musculature and the dorsal extensors before the manipulation is performed (Marshall and Hamilton, 1992). This is generally accomplished with a deep tissue massage, heat, or ice.
Occasionally, the manipulation may be unsuccessful and further manipulation should be avoided as this causes unnecessary pain to the patient (Marshall and Hamilton, 1992). In this rare instance, the patient’s symptoms may be treated and the manipulation performed the following day. A cuboid syndrome present for one week will respond to one or two manipulations (Newell and Woodle, 1981). On the other hand, the clinician may need to perform three of four manipulations on a patient with cuboid syndrome present for one month (Newell and Woodle, 1981). However, Jennings and Davies, 2005 found their patients with symptoms lasting one month responded to two manipulations. If the patient has had symptoms longer than six months, it may take up to six months to resolve with a 50% improvement in symptoms immediately after the successful manipulation (Newell and Woodle, 1981). After the clinician has performed a cuboid manipulation, pain should be reassessed, as this is the patient’s chief complaint, to objectively determine whether or not the manipulation was successful. Furthermore, once the manipulation has taken place, it is essential to reassess the patient at a functional level as there should be a decrease in their symptoms. Additionally, after the cuboid manipulation, various therapeutic modalities may be used to control pain and decrease inflammation. Immediately following manipulation, ice should be applied to the lateral foot as needed to reduce pain and inflammation (Blakeslee and Morris, 1987). The use of low intensity pulsed ultrasound is also warranted to facilitate collagen synthesis and should be increased to continuous ultrasound after the initial inflammatory response concludes, further promoting healing of the damaged tissues (Mooney and Maffey-Ward, 1994). Gentle massage has also been described in the literature to ease the patient’s pain following manipulation (Jennings and Davies, 2005; Mooney and Maffey-Ward, 1994).
The use of therapeutic modalities, alone, is not enough to facilitate the patient’s return to activity and prevent a reoccurrence of cuboid syndrome. Therefore, physical therapy may be used in conjunction (Mooney and Maffey-Ward, 1994). The therapeutic exercises should focus on stretching a tight peroneus longus and triceps surae, strengthening the intrinsic and extrinsic muscles of the foot, and proprioception through the use of neuromuscular control exercises (Mooney and Maffey-Ward, 1994).
Patients may return to vigorous activities if they are relatively symptom free following manipulation of the cuboid (Jennings and Davies, 2005; Marshall and Hamilton, 1992). However, if the patient wishes to engage in athletic activity before their symptoms have resolved or if the clinician deems it necessary, low dye taping can be used with or without a cuboid pad to maintain the cuboid’s position (Blakeslee and Morris, 1987; Newell and Woodle, 1981; Prentice, 2003). The cuboid pad should be constructed using a piece of 1/8 to ¼ inch felt approximately 1 ½ inches wide and measuring the distance from the calcaneocuboid articulation to the cuboid-fifth metatarsal articulation to determine the length, normally around 2-3 inches (White, 1996). The pad is placed on the plantar aspect of the cuboid, making sure that it does not extend past the styloid process of the fifth metatarsal, and held in place by a low dye taping technique (Caselli and Pantelaras, 2004).
Patient Outcomes
To date there have been several incidences of cuboid syndrome documented in the literature (Jennings and Davies, 2005; Marshall and Hamilton, 1992; Newell and Woodle, 1981). Unfortunately, the number of patients has been relatively low (N = 1 or N = 2) (Newell and Woodle, 1981; Marshall and Hamilton, 1992). Even though the number of patients was relatively low, immediate relief of symptoms has been reported following cuboid manipulation (Newell and Woodle, 1981). Jennings and Davies, 2005 evaluated 104 patients diagnosed with a plantar flexion and inversion ankle sprain and seven were further diagnosed with cuboid syndrome. These seven patients were then treated with the “cuboid whip ”manipulation (Jennings and Davies, 2005). Following the manipulation, the patients were objectively reassessed on their level of symptoms using the visual analog pain scale (VAS) (Crossely et al., 2004; Salo, et al., 2003). All of the patients reported a substantial resolution of their symptoms. However, two of the seven patients required a second manipulation the following day, due to their longer duration of symptoms than the other patients (Jennings and Davies, 2005). Upon a follow-up consultation period varying from two to eight months, no recurrence of symptoms was reported upon immediate return to their previous functional level (Jennings and Davies, 2005). Marshall and Hamilton, 1992 performed variations of the “cuboid squeeze ”on three patients. One of the three patients reported an immediate cessation of symptoms and was able to return to competition using a cuboid pad and low-dye taping to maintain the reduction. However, the other two patients had symptoms of a longer duration, and therefore required more than one manipulation. After a follow-up of five years, none of the three patients had a reoccurrence of symptoms. Therefore, this syndrome is unique because patients that are treated with the specific cuboid manipulations, as previously described, are able to return to their normal activities of daily living and athletic competition within 24 hours of treatment, if not immediately.
Conclusions
The minor disruption or subluxation of the structural congruity of the calcaneocuboid joint has yet to be clinically proven, but is thought to result in irritation of the surrounding joint capsule, ligaments, and peroneus longus tendon. The signs and symptoms of this condition are collectively known as cuboid syndrome. Many mechanisms have been postulated resulting in cuboid syndrome. Among these etiologies, overuse and plantar flexion and inversion forces are more widely accepted throughout the literature as a likely cause of cuboid syndrome. Therefore, the disruption may stem from an abnormal inversion force acting on the rearfoot when the forefoot is loaded during closed chain kinetics. Along with these more consistent mechanisms of injury, other situations have also contributed to cuboid syndrome, including the improper construction or use of orthoses and the repercussion of heel spur surgery. Once the clinician understands the signs and symptoms associated with cuboid syndrome the diagnosis is relatively straightforward. After a comprehensive evaluation and a differential diagnosis is made, cuboid syndrome responds exceptionally well to conservative treatment consisting of specific cuboid manipulation techniques, with many patients reporting immediate relief of symptoms after manipulation. The clinician may also choose to incorporate therapeutic modalities, therapeutic exercise, padding, and low dye taping into their treatment regimen.
Given that cuboid syndrome is common in athletic populations, some standardized diagnostic criteria must be established to assist the examiner in the clinical decision making processes. To the author’s knowledge, there have been no studies demonstrating the validity and reliability of the different diagnostic tests and treatment options which have been used in the diagnosis and treatment of cuboid syndrome. Therefore, additional research is necessary in the area of incidence, standardized examination procedures, and intervention methods used on the treatment of cuboid syndrome.
Figure 6b.

The knee is then passively extended as the ankle is plantar flexed with slight supination of the subtalar joint.
Figure 6c.

A thrust force is applied using both thumbs on the plantar aspect of the cuboid.
Acknowledgement
I would like to extend a special thank you to Brian E. Udermann, Ph.D, ATC, FACSM for his time and guidance throughout the preparation of this manuscript.
Biography
Stephen M. PATTERSON
Employment
Graduate assistant athletic trainer at the University of Wisconsin-La Crosse, USA.
Degree
Bachelors’ of Science degree in Athletic Training
Research interests
Cyrotherapy and its effects. The evaluation and management of knee and foot conditions.
E-mail: patterson3@mchsi.com patterso.stev@students.uwlax.edu
References
- Blakeslee T.J., Morris J.L. (1987) Cuboid syndrome and the significance of midtarsal joint stability. Journal of the American Podiatry Medical Association 77(12), 638-642 [DOI] [PubMed] [Google Scholar]
- Caselli M.A., Pantelaras N. (2004) How to treat cuboid syndrome in the athlete. Podiatry Today 17(10), 76-80 [Google Scholar]
- Crossley K.M., Bennell K.L., Cowan S.M., Green S. (2004) Analysis of outcome measures for persons with patellofemoral pain: Which are reliable and valid? Archives of Physical Medicine and Rehabilitation 85, 815-822 [DOI] [PubMed] [Google Scholar]
- Dewar F.P., Evans D.C. (1968) Occult fracture-subluxation of the midtarsal joint. Journal of Bone and Joint Surgery 50B, 386. [PubMed] [Google Scholar]
- Draves D.J. (1986) Anatomy of the lower extremity. Williams & Wilkins, Baltimore, MD [Google Scholar]
- Fagel V.L., Ocon E., Cantarella J.C., Feldman F. (1982) Case Report 183. Dislocation of the cuboid bone without fracture. Skeletal Radiology 7, 287-288 [DOI] [PubMed] [Google Scholar]
- Fallat L., Grimm D.J., Saracco J.A. (1998) Sprained ankle syndrome: prevalence and analysis of639 acute injuries. Journal of Bone and Joint Surgery British 37, 669-677 [DOI] [PubMed] [Google Scholar]
- Freeman M.A. (1965) Instability of the foot after injuries to the lateral ligament of the ankle. Journal of Bone and Joint Surgery British 47, 669-677 [PubMed] [Google Scholar]
- Gamble F.O., Yale I. (1975) Clinical foot roentgenology. Williams & Wilkins, Baltimore, MD [Google Scholar]
- Gough D.T., Broderick D.F., Kanuzik S.J., Cusak T.J. (1988) Dislocation of the cuboid bone without fracture. Annals of Emergency Medicine 17(10), 1095-1096 [DOI] [PubMed] [Google Scholar]
- Huson A. (1965) L’articulation calcaneo-cuboidienne. CR Assoc Anatomy 50, 540 [Google Scholar]
- Jahss M. (1982) Disorders of the foot. WB Saunders, Philadelphia, PA [Google Scholar]
- Jennings J., Davies G.J. (2005) Treatment of cuboid syndrome secondary to lateral ankle sprains: a case series. Journal of Orthopedic and Sports Physical Therapy 35(7), 409-415 [DOI] [PubMed] [Google Scholar]
- Jones L.H. (1973) Foot treatment without hand trauma. Journal of the American Osteopathic Association 72, 481. [PubMed] [Google Scholar]
- Khan K., Brown J., Vass N., Crichton K., Alexander R., Baxter A., Butler M., Wark J. (1995) Overuse injures in classical ballet. Sports Medicine 19(5), 341-357 [DOI] [PubMed] [Google Scholar]
- Kolker D., Marti C.B., Gautier E. (2002) Pericuboid fracture-dislocation with cuboid subluxation. Foot and Ankle International 23(2), 163-167 [DOI] [PubMed] [Google Scholar]
- Leerar P.J. (2001) Differential diagnosis of tarsal coalition versus cuboid syndrome in and adolescent athlete. Journal of Orthopedic and Sports Physical Therapy 31(12), 702-707 [DOI] [PubMed] [Google Scholar]
- Maigne J.Y., Vautravers P. (2003) Mechanism of action of spinal manipulative therapy. Joint Bone and Spine, 70, 336-341 [DOI] [PubMed] [Google Scholar]
- Main B.J., Jowett R.L. (1975) Injuries of the midtarsal joint. Journal of Bone and Joint Surgery 57B, 89. [PubMed] [Google Scholar]
- Magee D.L. (1987) Orthopedic physical assessment. WB Saunders Company, , Philadelphia, PA [Google Scholar]
- Mann R., Inman V.T. (1964) Phasic activity of intrinsic muscles of the foot. Journal of Bone and Joint Surgery 46, 469. [PubMed] [Google Scholar]
- Marshall P., Hamilton W.G. (1992) Cuboid subluxation in ballet dancers. American Journal of Sports Medicine 20(2), 169-175 [DOI] [PubMed] [Google Scholar]
- Melzack R., Wall P.D. (1965) Pain mechanisms; a new theory. Science 150, 971-979 [DOI] [PubMed] [Google Scholar]
- McDonough M.W., Ganley J.V. (1973) Dislocation of the cuboid. Journal of the American Podiatry Medical Association 63, 317-318 [DOI] [PubMed] [Google Scholar]
- Mooney M., Maffey-Ward L. (1994) Cuboid plantar and dorsal subluxations: assessment and treatment. Journal of Orthopedic and Sports Physical Therapy 20(4), 220-226 [DOI] [PubMed] [Google Scholar]
- Newell S.G., Woodle A. (1981) Cuboid Syndrome. Physician and Sports Medicine 9, 71-76 [DOI] [PubMed] [Google Scholar]
- Parks R.M. (1983) Biomechanic and sport injuries treatment in sports medicine: fitness, training, injuries. Urban & Scwarzeberg, Baltimore, MD [Google Scholar]
- Phillips R.M. (1985) Dysfunction of the peroneus longus after fracture of the cuboid. Journal of Foot Surgery 24, 99. [PubMed] [Google Scholar]
- Prentice W.E. (2003) Arnheim’s principles of athletic training: A competency based approach. 11th edition McGraw-Hill Higher Education, New York, New York [Google Scholar]
- Resnick D., Niwayama G. (1985) Diagnosis of bone and joint disorders. W.B. Saunders, Philadelphia. PA [Google Scholar]
- Root M., Orien W., Weed J. (1977) Normal and abnormal function of the foot. Clinical Biomechanics, Los Angeles, CA [Google Scholar]
- Salo D., Eget D., Lavery R.F., Garner L., Bernstein S., Tandon K. (2003) Can patients accurately read a visual analog pain scale? American Jounral of Emergency Medicine 21, 515-519 [DOI] [PubMed] [Google Scholar]
- Sarrafian S.K. (1983) Anatomy of the foot and ankle. J.B. Lippincott, Philadelphia, PA [Google Scholar]
- Starkey C., Ryan J. (2002) Evaluation of orthopedic and athletic injuries. 2nd edition.F.A. Davis Company, Philadelphia, PA [Google Scholar]
- Subotnick S.I. (1989) Peroneal cuboid syndrome. Journal of the American Podiatry Medical Association 79(8), 413-414 [DOI] [PubMed] [Google Scholar]
- Turner J.A., Deyo R.A., Loeser J.D., Von Korff M., Fordyce W.E. (1994) The importance of placebo effects in pan treatment and research. Journal of the American Medical Association 271, 1609-1614 [PubMed] [Google Scholar]
- Van Langelaan E.J. (1983) A kinematical analysis of the tarsal joints: an x-ray photogrammetric study. Acta Orthopedica Scandinavia 54, 204. [PubMed] [Google Scholar]
- Vernon H.T., Dhami M.S., Howley T.P., Annett R. (1986) Spinal manipulation and beta-endorphin: a controlled study of the effect of a spinal manipulation on plasma beta-endorphin levels in males. The Journal of Manipulative Physiological Therapy 9, 115-129 [PubMed] [Google Scholar]
- White S.C. (1996) Padding and taping techniques. Clinical Biomechanics of the Lower Extremities. Mosby, St. Louis, MO [Google Scholar]


