Abstract
Interurban road crashes often result in severe Road Traffic Injuries (RTIs). Prehospital emergency care on interurban roads was rarely evaluated in the low- and middle-income countries. The study highlighted the availability and quality of prehospital care facilities on interurban roads in Pakistan, a low-income country. The study setting was a 592-km-long National highway in the province of Sindh, Pakistan. Using the questionnaires adapted from the World Health Organization prehospital care guidelines [Sasser et al., 2005], managers and ambulance staff at the stations along highways were interviewed regarding the process of care, supplies in ambulances, and their experience of trauma care. Ambulance stations were either managed by the police or the Edhi Foundation (EF), a philanthropic organization. All highway stations were managed by the EF; the median distance between highway stations was 38 km (Interquartile Range [IQR]=27–46). We visited 14 stations, ten on the highway section, and four in cities, including two managed by the police. Most highway stations (n=13) received one RTI call per day. Half of stations (n=5) were inside highway towns, usually near primary or secondary-level healthcare facilities. Travel time to the nearest tertiary healthcare facility ranged from 31 to 70 minutes (median=48 minutes; IQR=30–60). Other shortcomings noted for stations were not triaging RTI cases (86%), informing hospitals (64%), or recording response times (57%). All ambulances (n=12) had stretchers, but only 58% had oxygen cylinders. The median schooling of ambulance staff (n=13) was 8 years (IQR=3–10), and the median paramedic training was 3 days (IQR=2–3). Observed shortcomings in prehospital care could be improved by public-private partnerships focusing on paramedic training, making available essential medical supplies, and linking ambulance stations with designated healthcare facilities for appropriate RTI triage.
INTRODUCTION
Road Traffic Injuries (RTI) are a major public health problem worldwide [Peden, 2010]. The RTI burden, however, is disproportionately distributed as more than 90% of RTI deaths occur in Low- and Middle-Income Countries (LMICs) [World Health Organization, 2009]. RTI-related inequalities exist at sub-national levels too, and they are facilitated by several factors such as socioeconomic status, road infrastructure, enforcement, and healthcare access [DiMaggio & Li, 2012]. For instance, RTI statistics suggest that crash severity is higher on interurban roads than urban roads [Observatoire National Interministérial de Sécurité Routière, 2006]. Indeed, high speed is the main determinant of RTI severity on interurban roads [Bhatti, Sobngwi-Tambekou, Lagarde, et al. 2010; Derry, Afukaar, Donkor, et al., 2007].
An appropriate prehospital emergency care provided on site and during transportation to an appropriate health-care facility could reduce RTI fatalities by almost half [Arreola-Risa, Mock, Lojero-Wheatly, et al., 2000; Kobusingye, Hyder, Bishai, et al., 2006; Murad, Issa, Mustafa, et al., 2012; Sasser, Varghese, Kellermann, et al., 2005]. In addition to essential resources, the process of care including, but not limited to, communication, activation, response, assessment, treatment, and transport of injured people to a formal health-care facility, when necessary, is often compromised in LMICs [Mohan, Tiwari, Meleckidzedeck, et al., 2006; Sasser et al., 2005]. A study showed that compared to Seattle (United states) those with a severe RTI in Monterrey (Mexico) and Kumasi (Ghana), two LMIC regions, were twice as likely to die in the prehospital setting [Kobusingye et al., 2006; Mock, Jurkovich, nii-Amon-Kotei, et al., 1998]. Most patients in LMICs are transported to a hospital using whatever means are available to them [Arreola-Risa, Mock, Herrera-Escamilla, et al., 2004; Mock, Tiska, Adu-Ampofo, et al., 2002; Montazeri, 2004]. Poorly trained paramedics, ill-equipped ambulances, and insufficient bystanders’ awareness are other frequently observed problems in LMICs. The World Health Assembly has therefore reiterated its call for reforming in the available prehospital care services worldwide [Anderson, Suter, Mulligan, et al., 2012].
Some LMICs have considered improvements in their healthcare systems with encouraging results [Kobusingye et al., 2006; Sasser, Varghese, Joshipura, et al., 2006]. For instance, RTI fatalities were reduced by almost half in Mexico by making available cervical immobilization, oropharyngeal airways and large bore intravenous lines [Arreola-Risa et al., 2000]. Most of these efforts have focused on urban settings. Though severe RTIs were more frequent on interurban roads than on urban roads, yet the availability and quality of these services were rarely evaluated in interurban settings of LMICs [Hameed, Schuurman, Razek, et al., 2010; Nielsen et al., 2012; Tachfouti, Bhatti, Nejjari, et al., 2011; van Beeck, Mackenbach, Looman, et al., 1991].
Pakistan is a low-income country with over 177 million inhabitants [Government of Pakistan, 2009]. The World Health Organization (WHO) estimated that, in 2007, 41 494 (90% confidence interval= 28 379–76 695) RTI fatalities occurred in Pakistan [World Health Organization, 2009]. A report from the province of Sindh suggested that RTI fatality was significantly higher in rural areas than urban areas [Shah, Khoumbati, & Soomro, 2007]. Pakistan lacked until a few years ago a structured prehospital care system, and private, philanthropic ambulance services provided most of the prehospital care [Razzak, Cone, & Rehmani, 2001]. Since 2004, the province of Punjab has established a government-funded prehospital care system, named Rescue 1122, which is operational in all major cities of the province [Waseem, Naseer, & Razzak, 2011]. Other provinces took similar initiatives, but the situation of prehospital care on more than 9 000 km-long-high capacity interurban road network was apparently not part of these reforms [Bhatti, Razzak, Lagarde, et al., 2011]. The objective of this study was to assess the availability and quality of prehospital care facilities on interurban roads in Pakistan.
METHODS
Study design and setting
The cross-sectional study setting was the section of national highway 5 (N5) situated in the province of Sindh, Pakistan. The N5 links almost all major cities in Pakistan, and almost 90% of the population uses this road section for interurban transport [Government of Pakistan, 2007]. In Sindh, the 592-km-long subsection of N5 extends from Karachi to Kot Sabzal. It is a four-lane roadwith two lanes in each direction [Bhatti et al., 2011]. Lanes are separated, but there are no physical barriers. The National Highway and Motorway Police enforce traffic rules on this road section [Khoso, Ekman, & Bhatti, 2011]. Previous investigations pointed out that the incidence of RTIs on this road section was higher than on a similar road in Western Europe [Bhatti et al., 2011]. A philanthropic organization, the Edhi Foundation (EF), has managed ambulance stations along this road section since early 1980s [Bhatti et al., 2011; Razzak et al., 2001].
Data collection and measures
Three authors (JAB, AKK, and NUS) visited ambulance stations and conducted the survey in September 2009. An ambulance station was formally defined as the location along highways where ambulances were stationed to respond to any medical emergency.
Managers and ambulance staff of the visited ambulance stations were interviewed using predefined grids. The grids were adapted from the WHO “Prehospital Trauma Care Systems” guidelines [Sasser et al, 2005]. Authors (JAR, HW and LRS) participated in adaptation of these grids during previous works in the Eastern Mediterranean region [Baqir, Razzak, Khan, et al., 2010; Razzak, Hyder, Akhtar, et al., 2008; Tachfouti et al., 2011]. Authors (JAB, AKK, and NUS) filled in the grids during face-to-face interviews with ambulance station managers and ambulance staff. All interviews took place in the ambulance station.
Grids about ambulance stations included questions regarding the location of station (km, urban setting, distance from the healthcare facility categorized as primary, secondary or tertiary level; the district headquarter or medical school hospital are considered as tertiary-level healthcare facilities), training of ambulance staff, and process of care (transfer and triage of patients). The ambulance supplies grid corresponded to the advanced prehospital care requirements mentioned in the WHO guidelines, consisting of 94 items of which 12 were desirable (denoted as D),and 82 items were essential (denoted as E) [Sasser et al., 2005]. The interview grid for ambulance staff included information about their age, education, designation, training duration, prehospital care experience, and RTI attended in the previous 30 days.
Analyses
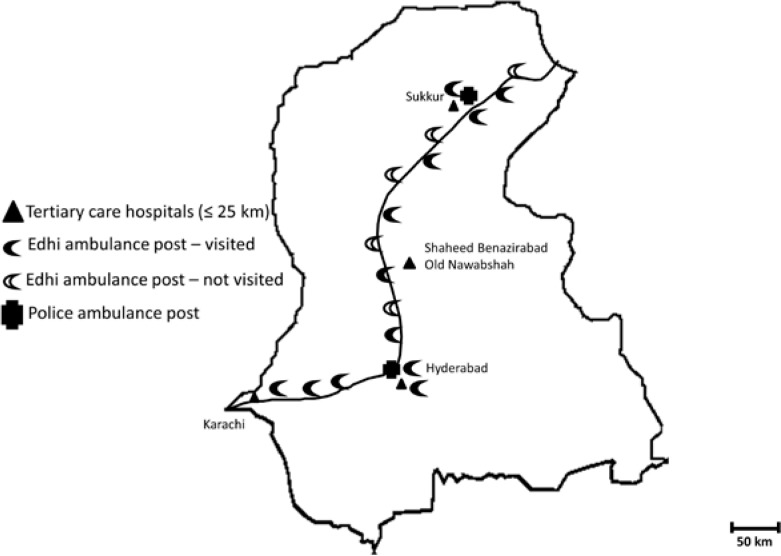
Locations of ambulance stations were depicted on a map. Findings about the characteristics of ambulance stations, available ambulances, and their staff were itemized and presented as percentages or median with Interquartile Range (IQR).
RESULTS
The study identified two types of ambulance stations: One, named Rescue 15, is managed by local police authorities, and the other by the EF. Ambulance stations managed by police are located inside major cities, namely Hyderabad and Sukkur. Police patrol cars have first aid kits, but police relied on EF ambulance services for RTI care. Key informants agreed and authors’ observations confirmed that only EF was providing prehospital care to RTI cases along this road section.
A typical EF station on the highway consists of a slightly elevated room within 20 feet of road shoulder, with one to two parking slots available for ambulances. The EF established 14 stations along selected interurban road section (Figure 1). The median distance between stations was 38 km (IQR=27–46). The longest distance between stations was 193 km, between the most peripheral station in Sindh and that situated in the province of Punjab.
Figure 1.
Ambulance Stations Surveyed in the Province of Sindh
Characteristics of visited stations
Of 14 EF highway stations, 10 (71.4%) were visited. All visited EF stations on highways consisted of one room where a clerk is placed with a telephone. Four other ambulance stations were also located in the major cities of the province, namely Hyderabad and Sukkur, and so these four were also included in this study; two of them were managed by police and two by the EF (Table 1). All stations had dedicated infrastructure with dedicated rooms and ambulance parking stations. All stations were working independently of local healthcare facilities. Forty-three percent of the highway ambulance stations were inside towns, usually in front of the primary- or secondary-level healthcare facilities. All these stations were within 1 to 5 km of the interurban road section.
Table 1.
Characteristics of Ambulance Stations on the National Highway 5, Sindh, Pakistan (September 2009)
| N | % | |
|---|---|---|
| Total stations visited | 14 | 100 |
| Type | ||
| - Philanthropic | 12 | 86 |
| - Police | 2 | 14 |
| Location | ||
| - Highway | 5 | 35 |
| - Inside highway towns (<5km) | 5 | 35 |
| - Inside major city (e.g., Hyderabad) | 4 | 30 |
| Staff composition | ||
| - Clerk | 12 | 86 |
| - Paramedic | 2 | 14 |
| - Drivers | 13 | 93 |
| Number of ambulance | ||
| - 1 | 9 | 64 |
| - 2 | 1 | 7 |
| - >2 | 4 | 29 |
| Registration of crash localization | ||
| - By landmark (e.g. hotel) | 14 | 100 |
| - By km | 0 | 0 |
| Interurban road crash call (per day) | ||
| - 1 | 13 | 93 |
| - 2–3 | 1 | 7 |
| Identification of caller | 8 | 57 |
| Level of nearest healthcare facility | ||
| - Tertiary care | 8 | 57 |
| - Secondary care | 5 | 36 |
| - Private | 1 | 7 |
| Distance from tertiary care facility | ||
| - 30 minutes | 6 | 43 |
| - 31–70 minutes | 8 | 57 |
| Triage for healthcare facility | ||
| - No | 12 | 86 |
| - Partial | 2 | 14 |
| - Yes | 0 | 0 |
| Inform healthcare facility | ||
| - No | 9 | 64 |
| - Yes | 5 | 36 |
| Response time measured | ||
| - No | 8 | 57 |
| - Yes | 6 | 43 |
Travel time to the nearest tertiary healthcare facility ranged from 31 to 70 minutes (median=48 minutes; IQR=30–60). All stations in major towns required at least 30 minutes for transferring interurban RTI cases to nearby tertiary care facilities. Most stations were staffed by non-medical personnel; paramedical staffs were stationed only in those managed by police. Most stations (n=13) received around one RTI call per day. Twelve stations did not participate in the triage of severely injured patients, and nine did not inform the nearest facilities about the imminent arrival of a trauma patient; eight did not record response times.
Characteristics of ambulances
Availability of required supplies could be assessed in 12 ambulances, of which one was managed by the police. The ambulances with more than eight medical supply items were stationed near Karachi (18 items) and in Hyderabad (12 items), i.e., the two most populated urban areas on interurban roads. The focus of EF ambulances was the transport of RTIs on a stretcher to the nearest healthcare facility, irrespective of RTI severity. Only half of the ambulances had an oxygen tank. Wireless communication was available in two thirds of ambulances.
Characteristics of EF ambulance staff
A total of 13 staffs were interviewed; all were designated as drivers, and were males. The median age of staff was 35 years (IQR=29–48). The median education received was 8 years (IQR=3–10). Nine drivers were involved in prehospital care for more than a year. The median prehospital care training received before being deployed was 3 days (IQR=2–3), and no driver attended any structured prehospital care course. The median number of RTI cases attended during the previous 30 days was 11 (IQR=2–30), and median number of RTI deaths observed during last 30 days was 4 (IQR=1–9).
DISCUSSION
This is the first survey of prehospital care facilities on interurban roadsin Pakistan [Nielsen et al., 2012; Razzak et al., 2001; Razzak et al., 2008; Waseem et al., 2011]. Overall, the results showed that prehospital care infrastructure existed along the selected interurban road section, but medical supplies required for providing actual care in the field were inadequate. Underdeveloped communication and triage mechanisms and unavailability of trained staff appeared to be major shortcomings in the current prehospital emergency care system on interurban roads in Pakistan.
Our findings suggest that the focus of private stake holders for road safety has been the establishment and maintenance of ambulance stations along interurban road sections. Like for most philanthropic agencies, personal donations fund the running expenses of the EF [Nielsen et al., 2012; Razzak et al., 2001; Waseem et al., 2011]. In addition to RTI care, ambulances were used to transport patients between healthcare facilities, or they were used in shifting cadavers from hospital to hometowns as a public service. Ensuring emergency care is the responsibility of the Government [Anderson et al., 2012] but, for highways in Sindh, the responsibility was unofficially delegated to private organizations. The EF has indeed facilitated the establishment of prehospital infrastructures along this highway but, at the same time, is providing other services. This could lead to de-prioritization of medical resources in the ambulances. Results were suggestive that a case could be made for a public-private partnership in improving the overall quality of prehospital healthcare services [Arreola-Risa et al., 2000]. For instance in the province of Sindh, the government handed over the management of primary-level healthcare facilities to the private sector. These actions led to improvements in the healthcare service delivery [Shaikh BT, Rabbani F, Safi N, et al., 2010]. Similar partnerships can be established in the prehospital care sector to improve services e.g., by providing funds for supplies, training, feul and salaries.
Furthermore, there are some specific inherent problems in providing prehospital care in selected interurban road settings [Nielsen et al., 2012; Razzak et al., 2001]. For instance, according to Pakistani law, paramedics are not allowed to administer medicines to patients. The current management of prehospital services, therefore, was focused on transferring as early as possible patients to the nearest healthcare facilities. While the services were reasonable close for most stations, the distance to nearby public hospital was more than 30 minutes. Thus, it was likely that the average response times could be higher than 60 minutes if the RTIs occurred 15 minutes away in the direction opposite from the hospital. Presence of ambulance stations within cities could also increase response times because of traffic. Therefore, improving care at the crash scene and during transport of RTI cases represents an important avenue of future interventions [Waseem et al., 2011]. Some of the recent initiatives in urban areas, such as Rescue 1122 services, have advanced the prehospital care agenda in Pakistan, including necessary legislations in this regard. Our study showed that the trickling down of these reforms in terms of improved medical supplies in ambulances and training of staff currently stationed on interurban roads is still lacking.
One of the immediate shortcomings that might need multidisciplinary interventions was the process of triage and communications with healthcare facilities. Informal discussions with managers of ambulance stations (not reported in results) indicated that the usual protocol is to bring the RTI patient to the nearest government facility. This is needed so that local health and police authorities can register information according to the medico-legal requirements without traveling too far and out of their jurisdiction. Consequently, ambulance staffs are, on some occasions, obliged to take serious RTI cases to local low-resourced healthcare facilities rather than heading to tertiary care hospitals. Previous surveys have indeed indicated that most secondary-level healthcare facilities have low capacity to treat severe RTIs [Baqir & Ejaz, 2011; Baqir et al., 2010]. Therefore, cooperation mechanisms with local police authorities, and the designation of trauma care facilities with levels are urgently needed to guide ambulance staff in triage of RTI cases to tertiary care facilities.
Limitations
This survey has several limitations. Firstly, the selected setting was the most used interurban road-section in the province of Sindh; it is likely that the observed prehospital care is more developed on the selected road than on other interurban road sections [Bhatti et al., 2011; Government of Pakistan, 2007]. Secondly, several outcome measures such as RTI cases per day or month were based on key-informant interviews because the available documentation was maintained as personal notes rather being tabulated in official registers. Therefore, care is needed while interpreting outcome measures. Thirdly, the investigators did not verify whether observed medical supply items were actually used in care, e.g., whether oxygen was available in cylinders and whether it was actually used during transportation. It might be possible that available items are not adequately used during prehospital care of RTI cases.
CONCLUSION
This survey confirms the existence of deficiencies in prehospital care on a selected Pakistani interurban road. Establishing public-private partnerships and reinforcing public service should be explored to improve the quality of prehospital care on interurban roads in Pakistan. The focus of these partnerships should be training paramedics and arranging essential supplies on interurban roads in Pakistan. Establishing the formal communication lines between ambulance stations and tertiary healthcare facilities might facilitate triage of RTI cases according to their severity. Furthermore, legislative changes and resources are needed, so that adequate RTI care is provided along with the required medico-legal processes. Lastly, this study illustrated how detailed evaluations of RTI prehospital care can be conducted in semi-urban and rural settings in LMIC settings.
Table 2.
Supplies Available in Ambulances on National Highway 5, Sindh, Pakistan (September 2009)
| N | % | |
|---|---|---|
| Ambulance management | ||
| - Philanthropic | 11 | 92 |
| - Police | 1 | 8 |
| Supplies* | ||
| - Stretcher (E) | 12 | |
| - Light-reflective clothing (E) | 9 | 100 |
| - Wireless communication (D) | 8 | 75 |
| - Oxygen cylinder (E) | 7 | 67 |
| - Writing material e.g. pencils (E) | 7 | 58 |
| - Blankets/Sheets (E) | 6 | 58 |
| - Potable water (E) | 6 | 50 |
| - Bandages (E) | 5 | 50 |
| - Non-sterile single use gloves (E) | 2 | 42 |
| - Torch (E) | 2 | 17 |
| - Flags/traffic control devices (E) | 2 | 17 |
| - Elastic bandages (E) | 2 | 17 |
| - Basic extrication material (E) | 1 | 17 |
| - Gauze rolls (E) | 1 | 8 |
| - Compresses (E) | 1 | 8 |
| - Absorbent cotton wool (E) | 1 | 8 |
| - Adhesive tape (E) | 1 | 8 |
| - Oral rehydrating salt (E) | 1 | 8 |
| - Thermometer (E) | 1 | 8 |
| - Antibiotic cream (E) | 1 | 8 |
| - Fire extinguisher (E) | 1 | 8 |
| - Blood pressure device (E) | 1 | 8 |
| - Stethoscope (E) | 1 | 8 |
| - List of local contacts (E) | 1 | 8 |
D – Desirable according to WHO [Mock et al., 2004]
E – Essential according to WHO [Mock et al., 2004]
Table 3.
Characteristics of Ambulance Staff on the National Highway 5, Sindh, Pakistan (September 2009) – all male drivers
| N | % | |
|---|---|---|
| Designation – Drivers | 13 | 100 |
| Prehospital care experience (in years) | ||
| - ≤ 1 | 4 | 31 |
| - > 1 | 9 | 69 |
| Median | IQR | |
| Age | 35 | 29–48 |
| Education (y) | 8 | 3–10 |
| Training before deployment (days) | 3 | 2–3 |
| Road traffic injury care trips in the last 30 days | 11 | 2–30 |
| Trauma deaths viewed in the last 30 days | 4 | 1–9 |
IQR Interquartile range
Acknowledgments
We are grateful to the managers and ambulance staff of the Edhi Ambulance stations and police officials for providing relevant information. The interpretations here are of the authors and do not represent position of the affiliated institutions.
REFERENCES
- Anderson PD, Suter RE, Mulligan T, et al. World Health Assembly Resolution 60.22 and Its Importance as a Health Care Policy Tool for Improving Emergency Care Access and Availability Globally. Ann Emerg Med. 2012;60:35–44. doi: 10.1016/j.annemergmed.2011.10.018. [DOI] [PubMed] [Google Scholar]
- Arreola-Risa C, Mock C, Herrera-Escamilla AJ, et al. Cost-effectiveness and Benefit of Alternatives to Improve Training for Prehospital Trauma Care in Mexico. Prehosp Disaster Med. 2004;19:318–25. doi: 10.1017/s1049023x00001953. [DOI] [PubMed] [Google Scholar]
- Arreola-Risa C, Mock CN, Lojero-Wheatly L, et al. Low-cost Improvements in Prehospital Trauma Care in a Latin American City. J Trauma. 2000;48:119–24. doi: 10.1097/00005373-200001000-00020. [DOI] [PubMed] [Google Scholar]
- Baqir M, Ejaz K. Role of Pre-Hospital Care and Ambulance Services in Karachi. J Pak Med Assoc. 2011;61:1167–69. [PubMed] [Google Scholar]
- Baqir SM, Razzak JA, Khan UR, et al. Assessment of Knowledge of Physicians about Trauma/Emergency Care in Public and Private Sectors in Four Districts of Sindh, Pakistan. Inj Prev. 2010;16(suppl 1):A289–90. [Google Scholar]
- Bhatti JA, Razzak JA, Lagarde E, et al. Differences in Police, Ambulance, and Emergency Department Reporting of Traffic Injuries on Karachi-Hala road, Pakistan. BMC Res Notes. 2011;4(1):75. doi: 10.1186/1756-0500-4-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatti JA, Sobngwi-Tambekou J, Lagarde E, et al. Situational Factors Associated with Road Traffic Crashes: A Case-Control Study on the Yaounde-Douala Road Section, Cameroon. Int J Inj Contr Saf Promot. 2010;17:215–22. doi: 10.1080/17457301003728510. [DOI] [PubMed] [Google Scholar]
- Derry JD, Afukaar FK, Donkor P, et al. Study of Vehicle Speeds on a Major Highway in Ghana: Implication for Monitoring and Control. Traffic Inj Prev. 2007;8:142–6. doi: 10.1080/15389580601100944. [DOI] [PubMed] [Google Scholar]
- DiMaggio C, Li G. Roadway Characteristics and Pediatric Pedestrian Injury. Epidemiol Rev. 2012;34:46–56. doi: 10.1093/epirev/mxr021. [DOI] [PubMed] [Google Scholar]
- Government of Pakistan . Pakistan Economic Survey 2008–09. Economic Advisor’s Wing, Finance Division, Government of Pakistan; Islamabad: 2009. [Google Scholar]
- Government of Pakistan . Pakistan Transport Plan Study in the Islamic Republic of Pakistan. Tripartite collaboration of the Japan International Cooperation Agency, National Transport Research Center, and Ministry of Communications, Government of Pakistan; Islamabad: 2007. [Google Scholar]
- Hameed SM, Schuurman N, Razek T, et al. Access to Trauma Systems in Canada. J Trauma. 2010;69:1350–61. doi: 10.1097/TA.0b013e3181e751f7. [DOI] [PubMed] [Google Scholar]
- Khoso AK, Ekman DS, Bhatti JA. Comparison of Highway Crash Reporting in Pakistan with the World Health Organization Injury Surveillance Guidelines. Traffic Inj Prev. 2011;12:279–82. doi: 10.1080/15389588.2011.561454. [DOI] [PubMed] [Google Scholar]
- Kobusingye OC, Hyder AA, Bishai D, et al. Emergency Medical Services. In: Jamison DT, Breman JG, Measham AR, et al., editors. Disease Control Priorities In Developing Countries. Second ed. World Bank; Washington, D.C: 2006. [Google Scholar]
- Mock CN, Jurkovich GJ, nii-Amon-Kotei D, et al. Trauma Mortality Patterns in Three Nations at Different Economic Levels: Implications for Global Trauma System Development. J Trauma. 1998;44:804–12. doi: 10.1097/00005373-199805000-00011. [DOI] [PubMed] [Google Scholar]
- Mock CN, Tiska M, Adu-Ampofo M, et al. Improvements in Prehospital Trauma Care in an African Country with no Formal Emergency Medical Services. J Trauma. 2002;53:90–7. doi: 10.1097/00005373-200207000-00018. [DOI] [PubMed] [Google Scholar]
- Mohan D, Tiwari G, Meleckidzedeck K, et al. Road Traffic Injury Prevention Manual. World Health Organization and Indian Insitute of Technology; Geneva: 2006. [Google Scholar]
- Montazeri A. Road-Traffic-Related Mortality in Iran: A Descriptive Study. Public Health. 2004;118:110–3. doi: 10.1016/S0033-3506(03)00173-2. [DOI] [PubMed] [Google Scholar]
- Murad MK, Issa DB, Mustafa FM, et al. Prehospital Trauma System Reduces Mortality in Severe Trauma: A Controlled Study of Road Traffic Casualties in Iraq. Prehosp Disaster Med. 2012;27:36–41. doi: 10.1017/S1049023X11006819. [DOI] [PubMed] [Google Scholar]
- Nielsen K, Mock C, Joshipura M, et al. Assessment of the Status of Prehospital Care in 13 Low- and Middle-Income Countries. Prehosp Emerg Care. 2012;16:381–9. doi: 10.3109/10903127.2012.664245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Observatoire National Interministérial de Sécurité Routière. La sécurité routière en France: Bilan de l’année 2004. La Documentation Française; Paris: 2006. [In French] [Google Scholar]
- Peden M. UN General Assembly Calls for Decade of Action for Road Safety. Inj Prev. 2010;16:213. doi: 10.1136/ip.2010.027839. [DOI] [PubMed] [Google Scholar]
- Razzak JA, Cone DC, Rehmani R. Emergency Medical Services and Cultural Determinants of an Emergency in Karachi, Pakistan. Prehosp Emerg Care. 2001;5:312–6. doi: 10.1080/10903120190939896. [DOI] [PubMed] [Google Scholar]
- Razzak JA, Hyder AA, Akhtar T, et al. Assessing Emergency Medical Care in Low Income Countries: A Pilot Study from Pakistan. BMC Emerg Med. 2008;8:8. doi: 10.1186/1471-227X-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasser SM, Varghese M, Joshipura M, et al. Preventing Death and Disability through the Timely Provision of Prehospital Trauma Care. Bull World Health Organ. 2006;84:507. doi: 10.2471/blt.06.033605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasser S, Varghese M, Kellermann A, et al. Prehospital Trauma Care Systems. World Health Organization; Geneva: 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah SG, Khoumbati K, Soomro B. The Pattern of Deaths in Road Traffic Crashes in Sindh, Pakistan. Int J Inj Contr Saf Promot. 2007;14:231–9. doi: 10.1080/17457300701646792. [DOI] [PubMed] [Google Scholar]
- Shaikh BT, Rabbani F, Safi N, et al. Contracting of Primary Health Care Services in Pakistan: Is Up-scaling a Pragmatic Thinking? J Pak Med Assoc. 2010;60(5):387–9. [PubMed] [Google Scholar]
- Tachfouti N, Bhatti JA, Nejjari C, et al. Emergency Trauma Care for Severe Injuries an a Moroccan Region: Conformance to French and World Health Organization standards. J Healthc Qual. 2011;33:30–8. doi: 10.1111/j.1945-1474.2010.00095.x. [DOI] [PubMed] [Google Scholar]
- van Beeck EF, Mackenbach JP, Looman CW, et al. Determinants of Traffic Accident Mortality in The Netherlands: A Geographical Analysis. Int J Epidemiol. 1991;20:698–706. doi: 10.1093/ije/20.3.698. [DOI] [PubMed] [Google Scholar]
- Waseem H, Naseer R, Razzak JA. Establishing a Successful Pre-Hospital Emergency Service in a Developing Country: Experience from Rescue 1122 Service in Pakistan. Emerg Med J. 2011;28:513–15. doi: 10.1136/emj.2010.096271. [DOI] [PubMed] [Google Scholar]
- World Health Organization . Global Status Report on Road Safety. World Health Organization; Geneva: 2009. [Google Scholar]