Abstract
The study purpose was to develop mortality-based metrics of injury severity for frequent motor vehicle crash (MVC) injuries. Injury severity was quantified with mortality-based metrics for 240 injuries comprising the top 95% most frequently occurring AIS 2+ injuries in the National Automotive Sampling System – Crashworthiness Data System (NASS-CDS) 2000–2011. Mortality risk ratios (MRRs) were computed by dividing the number of deaths by occurrences for each of the 240 injuries using National Trauma Data Bank Research Data System (NTDB-RDS) MVC cases. MRRMAIS was computed using only patients with a maximum AIS (MAIS) equal to the AIS severity of a given injury. Each injury had an associated MRR and MRRMAIS which ranged from zero (0% mortality representing low severity) to one (100% or universal mortality representing high severity). Injuries with higher MRR and MRRMAIS values are considered more severe because they resulted in a greater proportion of deaths among injured patients. The results illustrated an overall positive trend between AIS severity and the MRR and MRRMAIS values as expected, but showed large variations in MRR and MRRMAIS for some injuries of the same AIS severity. Mortality differences up to 83% (MRR) and 54% (MRRMAIS) were observed for injuries of the same AIS severity. The MRR-based measures of injury severity indicate that some lower AIS severity injuries may result in as many deaths as higher AIS severity injuries. This data-driven determination of injury severity using MRR and MRRMAIS provides a supplement or an alternative to AIS severity classification.
INTRODUCTION
Classification of the severity of an injury is designed to grade the threat to life and mortality associated with an injury. The severity in motor vehicle crash (MVC) injuries is commonly measured using the Abbreviated Injury Scale (AIS). The AIS is an advanced trauma-specific, anatomically-based injury coding lexicon defining injury type and severity [AAAM, 2008]. The “post-dot” component of each AIS code grades injury severity according to the threat to life, tissue damage, complexity of treatment, and impairment using the following severity scores and descriptions: Minor (1), Moderate (2), Serious (3), Severe (4), Critical (5), and Maximum/Unsurvivable (6). These severity scores, or “AIS severity,” are consensus-derived assessments assigned by a group of experts that were last updated in 2008.
The mortality associated with injuries can also be measured using mortality risk ratios (MRRs), the probabilistic complement of survival risk ratios (SRR) first proposed by Osler et al. [Osler, Rutledge, Deis et al., 1996]. An injury’s MRR is both lexicon- and database-specific. MRRs and SRRs have been calculated for both of the major trauma coding systems, AIS and International Classification of Diseases version 9 (ICD-9), and several data sources including the National Trauma Data Bank (NTDB) [Meredith, Evans, Kilgo et al., 2002; Kilgo, Osler and Meredith, 2003; Meredith, Kilgo and Osler, 2003a]. The MRR, a measure of the proportion of people who died that sustained a given injury, is reported to be among the most powerful discriminators of mortality following trauma [Sacco, MacKenzie, Champion et al., 1999; Meredith et al., 2002].
The objective of this study was to develop a mortality-based metric for quantifying the injury severity of frequently occurring MVC injuries.
METHODS
Top 95% AIS 2+ NASS-CDS Injuries
The top 95% most frequently occurring AIS 2+ injuries in MVCs were identified using the National Automotive Sampling System – Crashworthiness Data System (NASS-CDS) [National Highway Traffic Safety Administration, 2011]. NASS-CDS has detailed data on a representative, random sample of thousands of minor, serious, and fatal tow-away crashes in the United States (US). By applying weighting factors to NASS-CDS data, a representative population of MVCs in the US can be analyzed. NASS-CDS includes nearly 1,000 variables specifying vehicle, crash, and occupant characteristics, as well as injuries coded with the AIS coding lexicon.
NASS-CDS 2000–2011 was used in this study. National Highway Traffic Safety Administration (NHTSA) requirements for NASS-CDS crash investigations changed in 2009 and many variables (including all injury data) are not collected for model year (MY) vehicles greater than 10 years old. Thus, NASS-CDS 2009–2011 cases with MY vehicles greater than 10 years old were excluded from this analysis. This resulted in approximately 1/3 of the unweighted NASS-CDS 2009–2011 cases being excluded (11,814 distinct occupants excluded). After applying the exclusion criteria, the resulting NASS-CDS 2000–2011 dataset contained 54,703 cases, 94,283 vehicles, 134,846 occupants, and 303,230 injuries.
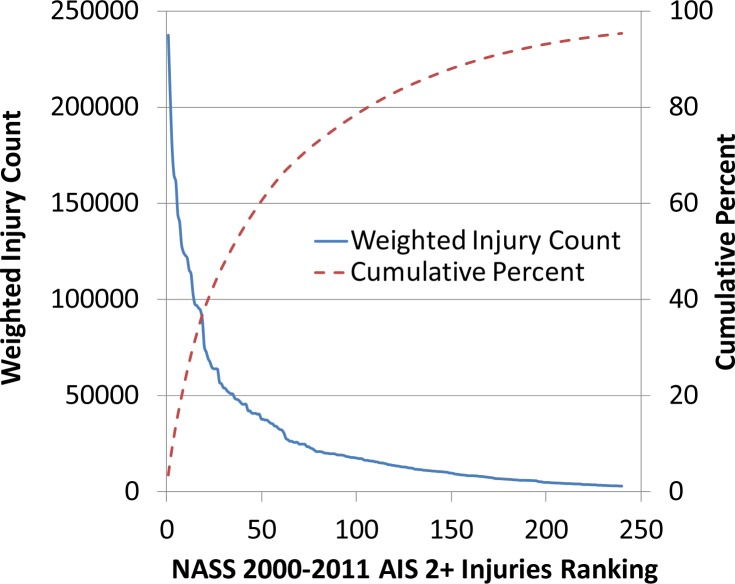
This study focused on a list of the top 95% most frequently occurring AIS 2+ injuries in NASS-CDS 2000–2011 (termed the “Top 95% List”). The Top 95% List was composed of 240 injuries located in the head, face, chest, abdomen, upper extremity, spine, and lower extremity body regions (Figure 1). Inclusion of 100% of the NASS-CDS 2000–2011 AIS 2+ injuries would have resulted in 848 unique AIS codes. The approach taken in this study simplifies the analysis to 240 unique injuries that frequently occur in MVCs.
Figure 1.
The weighted injury count and cumulative percent for injuries on the Top 95% List.
Mortality Risk Ratios
The NTDB Research Data System (NTDB-RDS) version 7.1 was used to calculate the MRR for each of the 240 injuries on the Top 95% List [Committee on Trauma; American College of Surgeons, 2007]. NTDB is the largest aggregation of trauma registry data ever assembled. It is supported by the American College of Surgeons (ACS) which collects information about patients, injuries, and treatments from participating trauma centers on an annual basis. Data submitted to NTDB is rigorously examined using both the National Trauma Registry of the ACS (NTRACS) software institutionally and an additional logical checks system created and enforced by NTDB administrators.
NTDB-RDS version 7.1 contains 1,926,245 cases from 2002–2006 admission years (Table 1). Cases having at least one AIS code in the Top 95% List were selected for analysis (823,499 cases). ICD-9 external cause codes (ecodes) that indicated MVC to be the cause of the injury were used to sub-select MVC cases. Ecodes 810–819 with post-dots of 0 or 1 were used to designate MVC cases, resulting in 241,935 cases used for the computation of MRRs.
Table 1.
NTDB-RDS version 7.1 admission counts.
| Year | Admission Count |
|---|---|
| 2002 | 324,907 |
| 2003 | 356,577 |
| 2004 | 342,881 |
| 2005 | 430,667 |
| 2006 | 471,213 |
| Total | 1,926,245 |
The MRR was calculated by dividing the number of deaths by occurrences for each AIS code in the Top 95% List (Equation 1). Each AIS code therefore had an associated MRR which could range from zero to one with zero representing 0% mortality and one representing 100% or universal associated mortality.
| Equation 1. Mortality Risk Ratio (MRR) |
Trauma patients often sustain multiple injuries and the impact of some of these injuries can have an effect on the computation of MRRs for single injuries, particularly if the co-injuries are of higher severity [Meredith, Kilgo and Osler, 2003b]. Thus, a MRR metric, MRRMAIS that accounts for the patient’s maximum AIS (MAIS) was computed. To compute MRRMAIS for a given injury, only patients with a MAIS equal to the AIS severity of the given injury were included in the calculation (Equation 2).
| Equation 2. Mortality Risk Ratio Adjusted by Maximum AIS (MRRMAIS) |
The MRR and MRRMAIS values for injuries on the Top 95% List were analyzed and compared to other injury severity measures using a variety of descriptive methods and regression analyses.
RESULTS
Sample Sizes
The sample sizes of injured and dead patients available for MRR computation varied depending on the injury. The number of patients sustaining a given injury ranged from 8 to 35,651 with a mean of 2,934, median of 1,314, and standard deviation of 4,332. The first and third quartiles indicated that 50% of the sample sizes of the total injured patients fell within the range of 509 to 3,865. The number of patients who died that sustained a given injury ranged from 0 to 3,223 with a mean of 225, median of 111, and standard deviation of 349. The first and third quartiles indicated that 50% of the sample sizes of the fatally injured patients fell within 42 to 283.
The sample sizes of injured and dead patients available for MRRMAIS computation also varied depending on the injury. The number of patients sustaining a given injury ranged from 1 to 22,852 with a mean of 1,378, median of 595, and standard deviation of 2,285. The first and third quartiles indicated that 50% of the sample sizes of the total injured patients fell within the range of 229 to 1,684. The number of patients who died that sustained a given injury ranged from 0 to 686 with a mean of 54, median of 9, and standard deviation of 111. The first and third quartiles indicated that 50% of the sample sizes of the fatally injured patients fell within 2 to 46. In general, the number of fatally injured patients included in the MRRMAIS calculation was much lower compared to the population of fatally injured patients used for the MRR calculation which could affect statistical power. There were no fatally injured patients available for 14% of the injuries when calculating MRRMAIS and 1% of the injuries when calculating MRR, respectively.
MRR Results and AIS Comparison
The MRR and MRRMAIS values ranged from zero (0% mortality) to one (100% mortality) for the 240 injuries on the Top 95% List. The distributions of the MRR and MRRMAIS values for the 240 injuries on the Top 95% List were right-skewed. The MRR mean and median were 0.13 and 0.07, respectively, with a standard deviation of 0.17. The first and third quartiles indicated that 50% of the MRRs fell within the 0.04 to 0.14 range. The MRRMAIS mean and median were 0.07 and 0.01, respectively, with a standard deviation of 0.16. The first and third quartiles indicated that 50% of the MRRMAIS values fell within the 0.00 to 0.05 range. A complete list of the MRR and MRRMAIS values for the 240 injuries on the Top 95% List is provided in the Appendix.
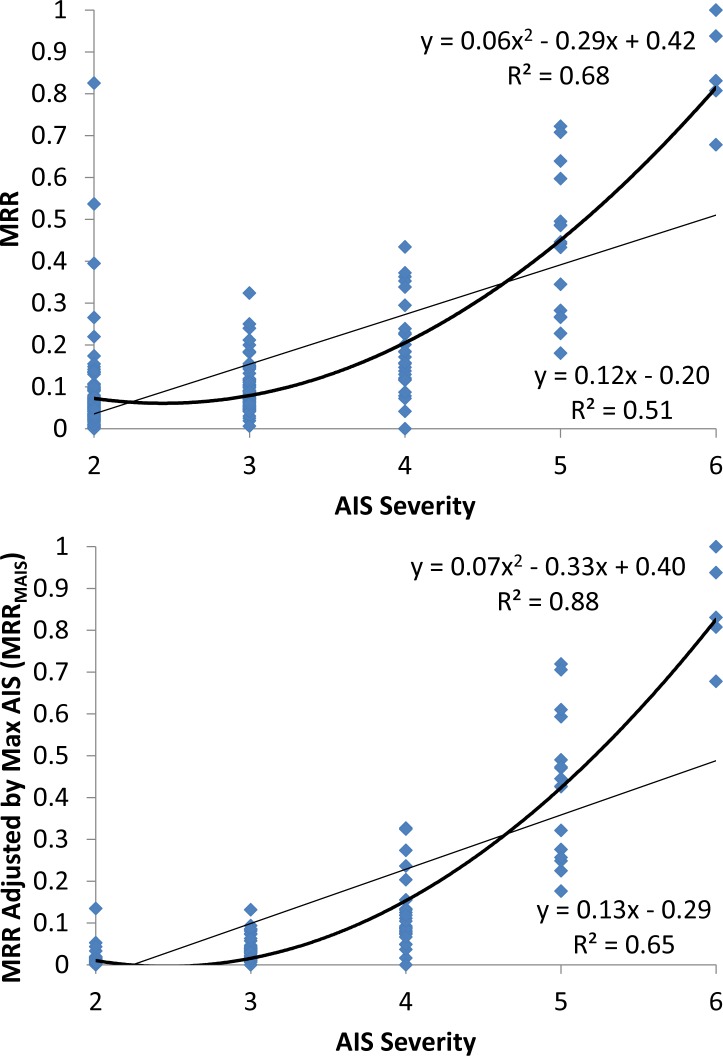
Each injury’s MRR and MRRMAIS were compared to its AIS severity counterpart (Figure 2). Overall positive trends when regressing MRR or MRRMAIS with the AIS severity were observed, but large variations in MRR and MRRMAIS are evident between injuries of the same AIS severity. The variations at a given AIS severity are diminished for MRRMAIS compared to MRR. Figure 2 shows that the MRR and MRRMAIS ranges overlap between AIS severity levels (particularly for the AIS 2–4 levels). Overlap occurs even for MRRMAIS that is adjusted for the patient’s MAIS. Linear and quadratic regressions were fit to the data (R2 values of 0.51 and 0.68, respectively for MRR, and 0.65 and 0.88, respectively for MRRMAIS). The quadratic regressions provided a better fit to the data, but there are many injuries in Figure 2 that are outliers that do not adhere to the linear or quadratic regression relationships.
Figure 2.
MRR and MRRMAIS versus AIS severity for injuries on the Top 95% List. Linear and quadratic regressions are fit to the data.
When stratifying by AIS severity, the mean and median of the MRR and MRRMAIS distributions increased as AIS severity increased (Table 2). The MRR and MRRMAIS values also varied within a given AIS severity level as the minimum and maximum measures in Table 2 demonstrate.
Table 2.
MRR and MRRMAIS summary statistics stratified by AIS severity.
| Severity | Mean | Median | Min | Max | |
|---|---|---|---|---|---|
| MRR | AIS 2 | 0.07 | 0.05 | 0.00 | 0.83 |
| AIS 3 | 0.09 | 0.08 | 0.01 | 0.32 | |
| AIS 4 | 0.19 | 0.16 | 0.00 | 0.43 | |
| AIS 5 | 0.44 | 0.44 | 0.18 | 0.72 | |
| AIS 6 | 0.85 | 0.83 | 0.68 | 1.00 | |
| MRRMAIS | AIS 2 | 0.01 | 0.00 | 0.00 | 0.13 |
| AIS 3 | 0.03 | 0.03 | 0.00 | 0.13 | |
| AIS 4 | 0.12 | 0.09 | 0.00 | 0.33 | |
| AIS 5 | 0.43 | 0.44 | 0.18 | 0.72 | |
| AIS 6 | 0.85 | 0.83 | 0.68 | 1.00 |
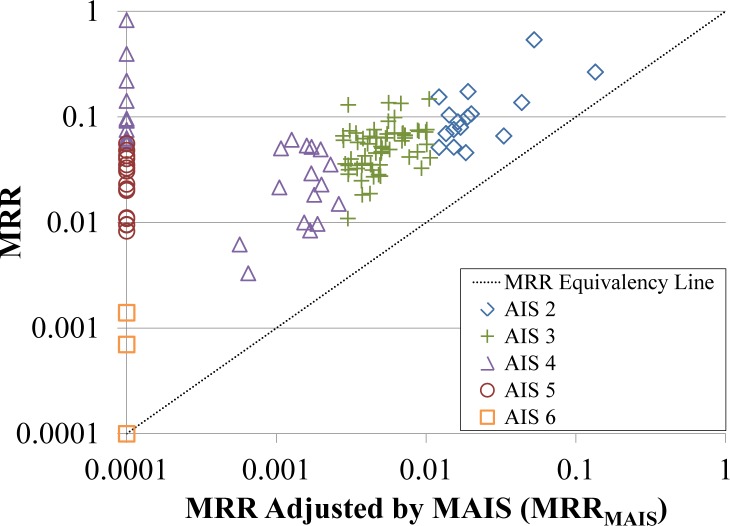
The discrepancies between MRR and MRRMAIS were larger for lower severity injuries, with AIS 2–4 injuries having an MRR that was generally higher than its MRRMAIS counterpart (Figure 3). Linear correlations indicated that MRRs for AIS 2–3 injuries tend to be two times higher than their MRRMAIS counterparts (Table 3). However, the correlation between MRR and MRRMAIS was low (R2 = 0.11) for AIS 2 injuries due to large variation in the MRR-MRRMAIS difference. The MRR-MRRMAIS difference was as much as 0.82 for some injuries. These large differences were likely affected by the smaller sample sizes, particularly in the dead population, that resulted from excluding patients with an MAIS higher than the injury of interest. MRR-MRRMAIS correlations are improved for AIS 3–6 injuries. The linear relationship for AIS 4 injuries indicated that MRRs are approximately 1.2 times higher than their MRRMAIS counterparts (Table 3). Controlling for MAIS affects AIS 5 injuries minimally and does not affect AIS 6 injuries at all since there are no injuries of higher severity that would exclude patients (Table 3 and Figure 3).
Figure 3.
MRR versus MRRMAIS stratified by AIS severity for injuries on the Top 95% List. Axes are plotted using a logarithmic scale. MRR and MRRMAIS values that were equal to zero were assigned a value of 0.0001 to facilitate plotting on the logarithmic scale.
Table 3.
Linear regressions of MRR with MRRMAIS stratified by AIS severity.
| Severity | N | Intercept | Slope | R2 |
|---|---|---|---|---|
| AIS 2 | 123 | 0.05 | 2.28 | 0.11 |
| AIS 3 | 68 | 0.02 | 2.00 | 0.69 |
| AIS 4 | 28 | 0.04 | 1.21 | 0.88 |
| AIS 5 | 16 | 0.01 | 1.00 | 1.00 |
| AIS 6 | 5 | 0.00 | 1.00 | 1.00 |
AIS 6 Injuries
There were five AIS 6 injuries on the Top 95% List with MRRs ranging from 0.68–1.00. The sample sizes of total injured and total dead used for MRR calculations are provided along with the average number of co-injuries (Table 4). Two of these injuries (441016.6, major heart laceration; 140218.6, brainstem transection) had 100% or near 100% mortality. However, three injuries had 68–83% mortality (113000.6, crush head injury; 140212.6 brain stem laceration; 420218.6 major thoracic aorta laceration). The sample sizes of injured and dead for these three injuries appear sufficient, suggesting these mortality rates are not biased by small samples. The injury with the MRR of 0.68 (113000.6) had a lower average number of AIS 2+, 3+, and 4+ co-injuries which could affect the mortality incidence. However, a single AIS 6 injury (with or without co-injuries) is considered to be highly unsurvivable by the AIS lexicon. The AIS lexicon classifies AIS 6 injuries as “Maximum/Unsurvivable” and patients with an AIS 6 injury are automatically assigned the maximum Injury Severity Score (ISS) of 75. While 68–83% mortality rates are certainly high and indicative of high injury severity, this data suggests a substantial number of patients are surviving some AIS 6 injuries. MRRs provide a quantitative measure of the mortality associated with AIS 6 injuries to distinguish between injuries that are truly unsurvivable and those that are severe, but potentially survivable.
Table 4.
MRRs, sample sizes, and average number of co-injuries for AIS 6 injuries.
| AIS Code | MRR | Total Injured | Total Dead | Avg # Co-injuries | ||
|---|---|---|---|---|---|---|
| AIS 2+ | AIS 3+ | AIS 4+ | ||||
| 113000.6 | 0.68 | 59 | 40 | 3.25 | 2.49 | 1.90 |
| 140212.6 | 0.81 | 107 | 87 | 8.21 | 5.90 | 3.62 |
| 420218.6 | 0.83 | 131 | 109 | 6.00 | 4.05 | 2.38 |
| 441016.6 | 0.94 | 16 | 15 | 7.81 | 4.81 | 2.88 |
| 140218.6 | 1.00 | 8 | 8 | 6.13 | 5.38 | 3.25 |
Select Injury Examples
Observations on MRR and MRRMAIS values for select AIS codes are provided in Table 5. The most common AIS 2+ head injury is an AIS 2 injury (160414.2, GCS 15, unconsciousness < 1hr) which has a MRR of 0.001 (<0.1% mortality) and a MRRMAIS of 0 indicating a low severity injury. The most common AIS 2+ lower extremity (852602.2, closed pelvis fracture) and abdomen (544222.2, spleen laceration) injuries are AIS 2 injuries with much higher MRRs of 0.064 and 0.071, respectively (6–7% mortality). The respective MRRMAIS values for these injuries were lower (0.007 and 0.003) indicating that AIS 3+ co-injuries were responsible for some of the increase in mortality associated with these AIS 2 injuries. Interestingly, the most common AIS 2+ chest injury, an AIS 3 unilateral lung contusion (441406.3), has an MRR of 0.064 identical to that of the AIS 2 closed pelvis fracture and less than that of the AIS 2 spleen laceration. However, when controlling for patient MAIS, the MRRMAIS for the AIS 3 unilateral lung contusion is 0.018 which is higher than the MRRMAIS of the aforementioned AIS 2 pelvis and spleen injuries.
Table 5.
MRR and MRRMAIS observations for select AIS codes. A rank is provided in the first column for each of the selected injuries indicating their frequency among NASS-CDS 2000–2011 AIS 2+ injuries. The percentage (%) of NASS-CDS 2000–2011 AIS 2+ injuries is also provided for each injury in the first column. The number of dead patients and total injured patients (ND/NI) used to compute MRR and MRRMAIS is included.
| Rank (%) | AIS Code | AIS Description | MRR (ND/NI) | MRRMAIS (ND/NI) | Observations |
|---|---|---|---|---|---|
| 1 (3.46) | 160414.2 | Awake post resuscitation on Admission or Initial Observation at Scene (GCS 15) unconsciousness known to be < 1 hr | 0.001 (1/1,410) | 0.000 (0/979) | Most common AIS 2+ head injury; AIS 2, low MRR and MRRMAIS |
| 3 (2.61) | 852602.2 | Pelvis fracture closed | 0.063 (1,233/19,526) | 0.007 (39/5,399) | Most common AIS 2+ lower extremity injury; AIS 2, moderate MRR and low MRRMAIS |
| 6 (2.10) | 441406.3 | Lung contusion unilateral with or without hemo-/pneumothorax | 0.064 (1,152/18,043) | 0.018 (208/11,594) | Most common AIS 2+ chest injury; AIS 3, moderate MRR and low MRRMAIS |
| 27 (0.93) | 450210.2 | Rib fractures, multiple, NFS | 0.107 (210/1,961) | 0.020 (11/549) | AIS 2 chest injury; high MRR and low MRRMAIS |
| 31 (0.78) | 544222.2 | Spleen, laceration, simple capsular tear <=3cm parenchymal depth and no trabecular vessel involvement; minor; superficial [OIS I, II] | 0.070 (524/7,453) | 0.003 (6/1,765) | Most common AIS 2+ abdomen injury; AIS 2, moderate MRR and low MRRMAIS |
| 57 (0.50) | 150404.3 | Vault fracture, comminuted; compound but dura intact; depressed <=2cm; displaced | 0.151 (289/1,918) | 0.041 (31/748) | AIS 3 head injury; high MRR and moderate MRRMAIS |
| 129 (0.18) | 140660.3 | Cerebrum injury [includes basal ganglia, thalamus, putamen, globus pallidus], brain swelling NFS | 0.240 (130/542) | 0.131 (18/137) | AIS 3 head injury; high MRR and MRRMAIS |
| 140 (0.16) | 160806.3 | Unconscious post resuscitation on Admission or Initial Observation at Scene (GCS <9) < 1 hr | 0.019 (5/264) | 0.017 (4/242) | AIS 3 head injury; low MRR and MRRMAIS |
| 141 (0.16) | 441602.2 | Pericardium, laceration; puncture | 0.825 (85/103) | 0.000 (0/1) | AIS 2 chest injury; extremely high MRR and low MRRMAIS due to small sample sizes |
| 175 (0.10) | 440604.3 | Diaphragm laceration (OIS Grade II thru IV) | 0.250 (209/835) | 0.094 (29/310) | AIS 3 chest injury; high MRR and MRRMAIS |
In a comparison of chest injuries, an AIS 2 multiple rib fracture injury (450210.2) has a higher MRR (0.107) and similar MRRMAIS (0.020) to the AIS 3 unilateral lung contusion. An AIS 3 diaphragm laceration has much higher MRR and MRRMAIS (0.250 and 0.094, respectively) compared to an AIS 3 unilateral lung contusion. Finally, the AIS 2 injury with the highest MRR (441602.2, pericardium laceration/puncture) has an MRR of 0.825 indicating 83% mortality, but an MRRMAIS of 0 computed from a single injured patient. In the case of an AIS 2 pericardium laceration, all but one patient had accompanying AIS 3+ injuries. AIS 3+ co-injuries were most common in the chest region and were present in 95% of patients sustaining a pericardium laceration with an average of 2.6 AIS 3+ chest co-injuries per patient. AIS 3+ co-injuries in the abdomen, head, and lower extremity regions were also present in 46%, 42%, and 29% of patients. AIS 3+ injuries to the face, spine, and upper extremity occurred in less than 13% of patients. While patient mortality estimated for the pericardium laceration is certainly affected by the co-injuries, MRR is superior to MRRMAIS in capturing the mortality associated with sustaining this particular injury since it is accompanied by AIS 3+ chest injuries 95% of the time.
Three examples of AIS 3 head injuries (150404.3, vault fracture; 160806.3, GCS < 9, unconscious < 1hr; 140660.3, cerebrum injury) have MRRs that range from 0.019–0.240, corresponding to mortality rates of 2–24%. MRRMAIS values for these three head injuries range from 0.017–0.131, corresponding to mortality rates of 2–13%. While MRR and MRRMAIS values are higher for the AIS 3 head injuries compared to the AIS 2 head injury in Table 5, the 11–22% differences in mortality estimated by MRR and MRRMAIS among the AIS 3 injuries are not captured by AIS severity scoring. Higher AIS severity co-injuries explain some of the elevation in MRRs for the vault fracture and the cerebrum injury since these injuries were accompanied by an AIS 4+ head injury in 56% and 64% of patients, respectively. In contrast, only 1% of patients with loss of consciousness coded as 160806.3 also received an AIS 4+ head injury. However, when excluding the patients with AIS 4+ co-injuries in any body region, the MRRMAIS values are still much higher for the vault fracture and cerebrum injury, suggesting that the mortality associated with these particular AIS 3 head injuries is higher than that of the AIS 3 loss of consciousness injury (160806.3).
Thus, the traditional AIS severity measure appears to not fully capture the mortality associated with some injuries frequently sustained in MVCs. It is evident from these select injury examples that the AIS severity scoring system may have limitations in capturing the true mortality associated with injuries and MRR or MRRMAIS metrics could at the very least serve as a supplement to current AIS severity scoring.
Age Effects
Patient age was not adjusted for when computing MRR or MRRMAIS, and may be important for the elderly population which is known to have decreased skeletal and physiological resilience and increased morbidity and mortality [Burstein, Reilly and Martens, 1976; Finelli, Jonsson, Champion et al., 1989; Perdue, Watts, Kaufmann et al., 1998; Zioupos and Currey, 1998]. Regressing the MRR and MRRMAIS values with the mean patient age for each injury, negative relationships with low correlation (R2 = 0.10 and 0.08, respectively) were found. Since the mean patient age was generally lower for injuries with higher MRR and MRRMAIS values, this suggests that there is not a dramatic effect on MRR metrics due to certain injuries being more common in the elderly. Age does appear to have some effect on patient mortality, as the mean age was higher for the dead patients compared to the surviving patients (44 versus 35 years, respectively). The mean age of the dead patients was higher than the mean age of the surviving patients for 95% of the 240 injuries studied.
DISCUSSION
AIS codes with higher MRR and MRRMAIS values are considered to be more severe injuries because they resulted in more deaths. Determining injury severity from MRR and MRRMAIS was used as an 240 alternative to the severity assigned by the AIS coding system. The results illustrated an overall positive trend between the AIS severity and the MRR and MRRMAIS values as expected, but showed large variations in MRR and MRRMAIS for some injuries of the same AIS severity. There was overlap of the ranges of the MRR and MRRMAIS values between different AIS severity levels such that some injuries of different AIS severities had similar MRR and/or MRRMAIS values. Although MRRMAIS values were generally lower than their MRR counterparts due to the adjustment of patient MAIS, MRRMAIS values still demonstrated variation in injury mortality not captured by the categorical AIS severity score. This data-driven determination of severity indicates that some lower AIS severity injuries may result in as many deaths as higher AIS severity injuries. The MRR and MRRMAIS values provide a quantitative mortality metric on a continuous scale that could be used as a supplement or alternative to AIS severity to better quantify an injury’s threat to life.
MRR and MRRMAIS values are presented together for each injury in this paper as each may be of value in particular scenarios and applications. MRRMAIS controls for patient MAIS by excluding patients with a higher MAIS than the AIS severity of the injury of interest and thus would be expected to be a more accurate estimate of the true mortality associated with the individual injury. However, the calculation of MRRMAIS is also limited by smaller sample sizes and reduced statistical power. To calculate the true mortality associated with an individual injury, only patients with isolated injuries should be included, which would reduce the sample size even further [Meredith et al., 2003b]. In contrast, MRRs are calculated using the complete sample of MVC trauma patients which improves statistical power, but the mortality of lower severity injuries (AIS 2–3) is likely overestimated due to higher severity co-injuries in patients with multiple injuries. As the investigation of the pericardium laceration showed, some injuries rarely occur without being accompanied by higher severity co-injuries and for injuries such as these, MRRs may represent a better measure of mortality compared to MRRMAIS. In a MVC scenario, multiple injury patient trauma occurs frequently and MVC researchers may find that MRR represents occupant mortality risk better than MRRMAIS, especially for particular injuries that occur rarely in isolation. However, we advocate for further investigation and are providing both MRR and MRRMAIS measures for the top 95% most frequently occurring AIS 2+ injuries in MVCs.
The majority (67%) of the injuries had MRRs less than 10%. Thus, it may be important to operate in this lower range of MRRs (0–0.10) when identifying a MRR threshold that best discriminates for mortality. Likewise, the majority (76%) of the injuries had MRRMAIS values less than 5%, indicating the 0–0.05 range may be important for establishing a mortality risk threshold that accounts for patient MAIS. While the focus of this study was not to define such thresholds, the methodology and results presented in this study could be used in the future for this purpose.
MRR-based measures of injury severity could be used as an alternative to AIS-based metrics for estimating patient mortality. The International Classification of Diseases Injury Severity Score (ICISS), derived as the product of all the SRRs of a patient’s ICD-9 codes, is a time-tested approach that has been found to be a better discriminator of mortality compared to several AIS-based metrics such as the ISS, New Injury Severity Score (NISS), and MAIS [Sacco et al., 1999; Meredith et al., 2002; Kilgo et al., 2003]. Kilgo et al. (2003) showed that a similar metric to ICISS, known as the Trauma Registry AIS Score (TRAIS) and computed using the product of all the SRRs of a patient’s AIS codes, represented the best AIS-based score for predicting mortality [Kilgo et al., 2003]. MRRs could be used instead of SRRs to derive a metric similar to TRAIS since the MRR is the probabilistic complement of SRR (computed as 1-SRR). The maximum MRR of all the injuries sustained by a patient may also prove to be a good discriminator of patient mortality and could serve as a non-AIS alternative to MAIS. In fact, it has been shown that ICISS and TRAIS discriminate for mortality better when only the SRR from the patient’s worst injury is included in the calculation as opposed to SRRs from all injuries [Kilgo et al., 2003]. Using just the worst injury’s MRR to estimate mortality may reduce the theoretical complexities associated with accounting for interaction between MRRs of individual injuries when mathematically estimating mortality for multiple injury patients. These MRR-based metrics could also be compared to scores such as the Trauma – Injury Severity Score (TRISS) and the Revised Trauma Score (RTS) that account for age or physiological measures [Boyd, Tolson and Copes, 1987; Champion, Sacco, Copes et al., 1989].
Limitations
The exclusion of NASS-CDS 2009–2011 cases with missing data presents a limitation, but allows for inclusion of newer NASS-CDS cases while treating cases with missing data appropriately. An alternate option would be to scale up injury numbers by 50% to account for the 1/3 of cases where this information is missing, but it was decided that excluding the cases with missing data would introduce the least amount of error into the dataset.
NTDB is not a population sample and disproportionately includes large trauma centers with younger and more severely injured patients. These inferences are subject to the biases inherent in any large, retrospective study of a convenience sample. Inter-center variation in measurement standards is known to be inconsistent in the NTDB, particularly with respect to treatment of dead on arrival patients. However, NTDB is the largest aggregation of trauma registry data and is rigorously examined by each institution contributing data and by NTDB administrators to ensure accuracy. The database does not contain information on MVC characteristics, pre-hospital care, or intra-hospital care, and thus these factors are not controlled for in this study. NTDB MVC cases were sub-selected for analysis to broadly control for injury causation, as MRRs for some injuries have been shown to differ for MVC versus non-MVC etiologies [Kilgo PD, Weaver AA, Barnard RT et al., 2013].
MRRs are likely underestimated in the NTDB sample due to an underreporting bias since fatally injured patients that did not survive long enough to be admitted to a hospital or that were dead on arrival may not be included in NTDB. The underestimation of mortality is expected to be higher for higher severity injuries, particularly for AIS 6 injuries. Although MRRs may be underestimated due to limitations associated with the NTDB sample, the data-driven estimation of mortality is still valuable and the data has shown that hundreds of trauma patients do survive after sustaining AIS 6 injuries classified as “Maximum/Unsurvivable” by the AIS coding lexicon.
There are fundamental flaws in the estimation of MRRs in any study since the impact of some injuries gets mathematically transferred to other injuries [Meredith et al., 2003b]. The MRRMAIS metric accounted for patient MAIS to demonstrate the effect higher severity co-injuries can have on MRR estimation. The analysis showed a decrease in the estimated mortality when excluding patients with a MAIS higher than the AIS index of the injury of interest, but excluding these patients resulted in much smaller sample sizes and further investigation is warranted. Additional covariates such as the anatomical region of co-injuries and patient age were not directly adjusted for in this study when computing MRR and MRRMAIS and present a limitation that could be addressed in the future using multivariate statistical models. Despite the limitation in the calculation of MRR, MRR-based measures are still leading discriminators of mortality following trauma and are important to consider when assessing the severity of common MVC injuries [Sacco et al., 1999; Meredith et al., 2002].
Future Work
In the future, the expert opinions of physicians could be used in conjunction with the MRR and AIS severity measures to further quantify injury mortality. Detailed studies on injury combinations could be undertaken to better quantify the mortality associated with single injuries and with particular combinations of injuries. Multivariate statistical studies could be undertaken to adjust for many covariates including the patient age and the anatomical region and severity of co-injuries. The MRR-based measure of severity described in this study will be used as part of a larger study to identify injuries necessitating treatment at a trauma center for incorporation into an advanced automatic crash notification algorithm.
CONCLUSION
MRRs for the top 95% most frequently occurring MVC injuries were computed by dividing the number of deaths by occurrences for each injury using MVC cases in the NTDB-RDS. An MRR-based metric, MRRMAIS, was also computed by including only patients with a MAIS equal to the AIS severity of the injury of interest. Injuries with higher MRR and MRRMAIS values are considered to be more severe because they resulted in a greater proportion of deaths among injured patients. An overall positive trend between AIS severity and the MRR/MRRMAIS values was observed, but there were large variations in MRR and MRRMAIS for some injuries of the same AIS severity. Up to an 83% difference in mortality (0.83 difference in MRR) was indicated by MRRs for injuries of the same AIS severity. When controlling for patient MAIS, up to a 54% difference in mortality (0.54 difference in MRRMAIS) was indicated by MRRMAIS values for injuries of the same AIS severity. Some lower AIS severity injuries had MRRs that were greater than the MRRs for higher AIS severity injuries and similar results were observed for MRRMAIS. The data-driven determination of injury severity using MRR or MRRMAIS provides a supplement or an alternative to AIS severity that may better quantify the true mortality associated with injuries.
Acknowledgments
Funding has been provided by Toyota Motor Corporation and its affiliates. Views expressed are those of the authors and do not represent the views of any of the sponsors. NTDB data was provided by the Committee on Trauma, American College of Surgeons. NTDB Version 7.1 Chicago, IL, 2007. The content reproduced from the NTDB remains the full and exclusive copyrighted property of the American College of Surgeons. The American College of Surgeons is not responsible for any claims arising from works based on the original Data, Text, Tables, or Figures.
APPENDIX. MRR and MRRMAIS values for the AIS codes on the Top 95% List. Injuries are sorted by ascending AIS severity and then by ascending AIS pre-dot code.
| AIS Code | MRR | MRRMAIS | AIS Code | MRR | MRRMAIS | AIS Code | MRR | MRRMAIS |
|---|---|---|---|---|---|---|---|---|
| 110604.2 | 0.090 | 0.016 | 542020.2 | 0.155 | 0.012 | 815000.2 | 0.066 | 0.033 |
| 150400.2 | 0.104 | 0.014 | 542022.2 | 0.092 | 0.000 | 840402.2 | 0.000 | 0.000 |
| 150402.2 | 0.099 | 0.006 | 542810.2 | 0.142 | 0.000 | 840404.2 | 0.010 | 0.000 |
| 160202.2 | 0.008 | 0.002 | 544210.2 | 0.046 | 0.005 | 840600.2 | 0.023 | 0.000 |
| 160406.2 | 0.006 | 0.001 | 544212.2 | 0.053 | 0.005 | 840802.2 | 0.010 | 0.000 |
| 160410.2 | 0.003 | 0.001 | 544220.2 | 0.130 | 0.003 | 841002.2 | 0.020 | 0.000 |
| 160414.2 | 0.001 | 0.000 | 544222.2 | 0.070 | 0.003 | 850210.2 | 0.036 | 0.004 |
| 160602.2 | 0.001 | 0.000 | 650200.2 | 0.011 | 0.000 | 850214.2 | 0.031 | 0.000 |
| 160606.2 | 0.011 | 0.003 | 650204.2 | 0.069 | 0.005 | 850218.2 | 0.056 | 0.000 |
| 160610.2 | 0.000 | 0.000 | 650208.2 | 0.537 | 0.053 | 850610.2 | 0.027 | 0.004 |
| 160699.2 | 0.015 | 0.003 | 650209.2 | 0.043 | 0.000 | 850614.2 | 0.028 | 0.005 |
| 161000.2 | 0.010 | 0.002 | 650216.2 | 0.073 | 0.009 | 850806.2 | 0.046 | 0.018 |
| 210604.2 | 0.043 | 0.004 | 650218.2 | 0.063 | 0.005 | 850818.2 | 0.035 | 0.004 |
| 241202.2 | 0.057 | 0.000 | 650220.2 | 0.061 | 0.001 | 850822.2 | 0.008 | 0.000 |
| 243404.2 | 0.096 | 0.000 | 650230.2 | 0.067 | 0.007 | 850826.2 | 0.010 | 0.002 |
| 250200.2 | 0.033 | 0.000 | 650232.2 | 0.057 | 0.003 | 851400.2 | 0.022 | 0.001 |
| 250608.2 | 0.035 | 0.000 | 650416.2 | 0.059 | 0.007 | 851605.2 | 0.070 | 0.014 |
| 250610.2 | 0.075 | 0.009 | 650418.2 | 0.066 | 0.003 | 851606.2 | 0.047 | 0.009 |
| 250612.2 | 0.035 | 0.003 | 650420.2 | 0.064 | 0.005 | 851608.2 | 0.019 | 0.004 |
| 250616.2 | 0.040 | 0.000 | 650430.2 | 0.049 | 0.002 | 851610.2 | 0.052 | 0.012 |
| 250800.2 | 0.063 | 0.005 | 650432.2 | 0.029 | 0.003 | 851612.2 | 0.029 | 0.002 |
| 250802.2 | 0.076 | 0.010 | 650616.2 | 0.040 | 0.003 | 852000.2 | 0.032 | 0.003 |
| 250806.2 | 0.051 | 0.005 | 650618.2 | 0.063 | 0.000 | 852002.2 | 0.137 | 0.043 |
| 251004.2 | 0.052 | 0.002 | 650620.2 | 0.054 | 0.002 | 852200.2 | 0.018 | 0.002 |
| 251200.2 | 0.070 | 0.007 | 650630.2 | 0.028 | 0.005 | 852400.2 | 0.035 | 0.004 |
| 251202.2 | 0.050 | 0.001 | 650632.2 | 0.023 | 0.002 | 852600.2 | 0.070 | 0.006 |
| 251604.2 | 0.048 | 0.000 | 740400.2 | 0.055 | 0.010 | 852602.2 | 0.063 | 0.007 |
| 251800.2 | 0.076 | 0.004 | 750230.2 | 0.021 | 0.000 | 853200.2 | 0.018 | 0.004 |
| 441602.2 | 0.825 | 0.000 | 751030.2 | 0.035 | 0.002 | 853404.2 | 0.076 | 0.015 |
| 441800.2 | 0.395 | 0.000 | 751230.2 | 0.080 | 0.017 | 853406.2 | 0.033 | 0.009 |
| 450210.2 | 0.107 | 0.020 | 751430.2 | 0.011 | 0.000 | 853412.2 | 0.025 | 0.004 |
| 450220.2 | 0.052 | 0.015 | 751800.2 | 0.266 | 0.135 | 853414.2 | 0.031 | 0.004 |
| 450804.2 | 0.091 | 0.006 | 751900.2 | 0.220 | 0.000 | 853420.2 | 0.047 | 0.005 |
| 540610.2 | 0.075 | 0.000 | 752002.2 | 0.033 | 0.003 | 140466.3 | 0.324 | 0.081 |
| 540810.2 | 0.174 | 0.019 | 752200.2 | 0.070 | 0.007 | 140602.3 | 0.091 | 0.046 |
| 541410.2 | 0.136 | 0.006 | 752402.2 | 0.056 | 0.000 | 140604.3 | 0.055 | 0.015 |
| 541610.2 | 0.062 | 0.004 | 752500.2 | 0.041 | 0.011 | 140606.3 | 0.052 | 0.010 |
| 541612.2 | 0.060 | 0.000 | 752600.2 | 0.100 | 0.019 | 140612.3 | 0.182 | 0.084 |
| 541620.2 | 0.093 | 0.000 | 752602.2 | 0.067 | 0.007 | 140614.3 | 0.098 | 0.036 |
| 541622.2 | 0.056 | 0.004 | 752800.2 | 0.042 | 0.008 | 140620.3 | 0.142 | 0.037 |
| 541810.2 | 0.072 | 0.010 | 752802.2 | 0.036 | 0.003 | 140622.3 | 0.115 | 0.022 |
| 541812.2 | 0.060 | 0.003 | 753000.2 | 0.065 | 0.004 | 140660.3 | 0.240 | 0.131 |
| 541820.2 | 0.148 | 0.010 | 753200.2 | 0.045 | 0.005 | 140662.3 | 0.048 | 0.011 |
| 541822.2 | 0.074 | 0.003 | 753202.2 | 0.035 | 0.005 | 140682.3 | 0.117 | 0.030 |
| 542010.2 | 0.134 | 0.007 | 810604.2 | 0.049 | 0.006 | 140684.3 | 0.184 | 0.063 |
| 150200.3 | 0.105 | 0.040 | 851810.3 | 0.082 | 0.040 | 140656.5 | 0.495 | 0.490 |
| 150202.3 | 0.090 | 0.020 | 851812.3 | 0.073 | 0.033 | 140666.5 | 0.708 | 0.705 |
| 150404.3 | 0.151 | 0.041 | 851814.3 | 0.042 | 0.010 | 160824.5 | 0.597 | 0.593 |
| 160802.3 | 0.049 | 0.041 | 851818.3 | 0.052 | 0.019 | 420210.5 | 0.433 | 0.426 |
| 160806.3 | 0.019 | 0.017 | 851822.3 | 0.052 | 0.019 | 420216.5 | 0.441 | 0.427 |
| 250808.3 | 0.103 | 0.033 | 852604.3 | 0.063 | 0.020 | 441012.5 | 0.640 | 0.610 |
| 251204.3 | 0.069 | 0.011 | 852800.3 | 0.077 | 0.023 | 450242.5 | 0.267 | 0.248 |
| 440604.3 | 0.250 | 0.094 | 853000.3 | 0.083 | 0.028 | 450266.5 | 0.446 | 0.445 |
| 441402.3 | 0.071 | 0.032 | 853405.3 | 0.089 | 0.030 | 541828.5 | 0.486 | 0.473 |
| 441406.3 | 0.064 | 0.018 | 853408.3 | 0.041 | 0.017 | 544228.5 | 0.266 | 0.257 |
| 441430.3 | 0.200 | 0.038 | 853422.3 | 0.059 | 0.015 | 113000.6 | 0.678 | 0.678 |
| 441499.3 | 0.092 | 0.074 | 140410.4 | 0.138 | 0.081 | 140212.6 | 0.808 | 0.808 |
| 442202.3 | 0.111 | 0.043 | 140629.4 | 0.121 | 0.086 | 140218.6 | 1.000 | 1.000 |
| 442204.3 | 0.100 | 0.036 | 140630.4 | 0.078 | 0.049 | 420218.6 | 0.831 | 0.831 |
| 450211.3 | 0.148 | 0.073 | 140632.4 | 0.041 | 0.016 | 441016.6 | 0.938 | 0.938 |
| 450214.3 | 0.071 | 0.033 | 140638.4 | 0.130 | 0.073 | |||
| 450222.3 | 0.089 | 0.036 | 140640.4 | 0.072 | 0.037 | |||
| 450230.3 | 0.075 | 0.034 | 140642.4 | 0.087 | 0.049 | |||
| 450250.3 | 0.089 | 0.036 | 140650.4 | 0.147 | 0.092 | |||
| 521604.3 | 0.212 | 0.074 | 140652.4 | 0.118 | 0.066 | |||
| 540824.3 | 0.155 | 0.057 | 140664.4 | 0.434 | 0.274 | |||
| 541424.3 | 0.089 | 0.034 | 140678.4 | 0.225 | 0.118 | |||
| 541824.3 | 0.119 | 0.039 | 140688.4 | 0.171 | 0.089 | |||
| 544214.3 | 0.073 | 0.039 | 150206.4 | 0.363 | 0.203 | |||
| 544224.3 | 0.098 | 0.022 | 150406.4 | 0.353 | 0.236 | |||
| 544240.3 | 0.146 | 0.086 | 160820.4 | 0.000 | 0.000 | |||
| 650222.3 | 0.046 | 0.013 | 420206.4 | 0.372 | 0.327 | |||
| 650224.3 | 0.048 | 0.016 | 420208.4 | 0.229 | 0.125 | |||
| 650226.3 | 0.051 | 0.020 | 440606.4 | 0.239 | 0.134 | |||
| 650228.3 | 0.077 | 0.039 | 441410.4 | 0.157 | 0.078 | |||
| 650234.3 | 0.087 | 0.018 | 441450.4 | 0.295 | 0.155 | |||
| 650424.3 | 0.071 | 0.019 | 450232.4 | 0.116 | 0.075 | |||
| 650426.3 | 0.044 | 0.021 | 450240.4 | 0.201 | 0.111 | |||
| 650434.3 | 0.053 | 0.018 | 450252.4 | 0.155 | 0.087 | |||
| 650624.3 | 0.025 | 0.009 | 450260.4 | 0.339 | 0.325 | |||
| 650634.3 | 0.030 | 0.006 | 450264.4 | 0.183 | 0.131 | |||
| 752604.3 | 0.066 | 0.017 | 541626.4 | 0.157 | 0.105 | |||
| 752804.3 | 0.044 | 0.012 | 541826.4 | 0.185 | 0.119 | |||
| 753204.3 | 0.047 | 0.016 | 544226.4 | 0.117 | 0.066 | |||
| 840406.3 | 0.006 | 0.000 | 140202.5 | 0.722 | 0.719 | |||
| 851614.3 | 0.041 | 0.022 | 140204.5 | 0.345 | 0.321 | |||
| 851800.3 | 0.132 | 0.063 | 140210.5 | 0.487 | 0.470 | |||
| 851801.3 | 0.111 | 0.030 | 140628.5 | 0.180 | 0.176 | |||
| 851804.3 | 0.056 | 0.031 | 140646.5 | 0.227 | 0.225 | |||
| 851808.3 | 0.045 | 0.010 | 140654.5 | 0.282 | 0.275 |
REFERENCES
- AAAM Abbreviated Injury Scale 2005 (Update 2008) Association for the Advancement of Automotive Medicine. 2008. [PMC free article] [PubMed]
- Boyd CR, Tolson MA, Copes WS. Evaluating trauma care: the TRISS method. Trauma Score and the Injury Severity Score. J Trauma. 1987;27(4):370–8. [PubMed] [Google Scholar]
- Burstein AH, Reilly DT, Martens M. Aging of bone tissue: mechanical properties. J Bone Joint Surg Am. 1976;58(1):82–6. [PubMed] [Google Scholar]
- Champion HR, Sacco WJ, Copes WS, et al. A revision of the Trauma Score. J Trauma. 1989;29(5):623–9. doi: 10.1097/00005373-198905000-00017. [DOI] [PubMed] [Google Scholar]
- Committee on Trauma. American College of Surgeons . National Trauma Data Bank - Research Data System 7.1. Chicago, IL: 2007. [Google Scholar]
- Finelli FC, Jonsson J, Champion HR, et al. A Case Control Study for Major Trauma in Geriatric Patients. J Trauma. 1989;29(5):541–548. doi: 10.1097/00005373-198905000-00001. [DOI] [PubMed] [Google Scholar]
- Kilgo PD, Weaver AA, Barnard RT, et al. Comparison of Injury Mortality Risk in Motor Vehicle Crash Versus Other Etiologies. Journal of Emergency Medicine. 2013 doi: 10.1016/j.aap.2014.03.001. (In Review) [DOI] [PubMed] [Google Scholar]
- Kilgo PD, Osler TM, Meredith W. The worst injury predicts mortality outcome the best: rethinking the role of multiple injuries in trauma outcome scoring. J Trauma. 2003;55(4):599–606. doi: 10.1097/01.TA.0000085721.47738.BD. discussion 606–7. [DOI] [PubMed] [Google Scholar]
- Meredith JW, Evans G, Kilgo PD, et al. A comparison of the abilities of nine scoring algorithms in predicting mortality. J Trauma. 2002;53(4):621–8. doi: 10.1097/00005373-200210000-00001. discussion 628–9. [DOI] [PubMed] [Google Scholar]
- Meredith JW, Kilgo PD, Osler T. A fresh set of survival risk ratios derived from incidents in the National Trauma Data Bank from which the ICISS may be calculated. J Trauma. 2003a;55(5):924–32. doi: 10.1097/01.TA.0000085645.62482.87. [DOI] [PubMed] [Google Scholar]
- Meredith JW, Kilgo PD, Osler TM. Independently derived survival risk ratios yield better estimates of survival than traditional survival risk ratios when using the ICISS. J Trauma. 2003b;55(5):933–8. doi: 10.1097/01.TA.0000085646.71451.5F. [DOI] [PubMed] [Google Scholar]
- National Highway Traffic Safety Administration 2011. National Automotive Sampling System. Department of Transportation.
- Osler T, Rutledge R, Deis J, et al. ICISS: an international classification of disease-9 based injury severity score. J Trauma. 1996;41(3):380–6. doi: 10.1097/00005373-199609000-00002. discussion 386–8. [DOI] [PubMed] [Google Scholar]
- Perdue PW, Watts DD, Kaufmann CR, et al. Differences in Mortality between Elderly and Younger Adult Trauma Patients: Geriatric Status Increases Risk of Delayed Death. J Trauma. 1998;45(4):805–810. doi: 10.1097/00005373-199810000-00034. [DOI] [PubMed] [Google Scholar]
- Sacco WJ, MacKenzie EJ, Champion HR, et al. Comparison of alternative methods for assessing injury severity based on anatomic descriptors. J Trauma. 1999;47(3):441–6. doi: 10.1097/00005373-199909000-00001. discussion 446–7. [DOI] [PubMed] [Google Scholar]
- Zioupos P, Currey JD. Changes in the stiffness, strength, and toughness of human cortical bone with age. Bone. 1998;22(1):57–66. doi: 10.1016/s8756-3282(97)00228-7. [DOI] [PubMed] [Google Scholar]