Abstract
OBJECTIVE:
To study the outcome of subtrochanteric hip fractures treated with proximal lateral femur locking plate.
METHOD:
We retrospectively reviewed the clinical results of 48 cases of femoral subtrochanteric fractures treated with proximal lateral femur locking plates from January 2008 to May 2010. The progress of fracture healing, as well as the occurrence of complications, was recorded. The function of the hip joint was evaluated by the Harris social index and the Parker and Palmer mobility score one year after the operation.
RESULT:
45 patients were followed up until fracture union or a revision surgery. Among the 45 patients, 43 patients obtained fracture union without further intervention. Thirty-eight fractures healed with no loss of position at 1-year follow-up. There were no cases of hip screw cutting through the femoral head. The mean score of the Harris social index was 86.5±9.8 (73~95). The mean Parker and Palmer mobility score was 7.4±2.1 (3~9).
CONCLUSION:
The proximal lateral femur locking plate is the kind of stable and effective internal fixation for treating subtrochanteric hip fractures which has the advantage of stable fixation especially for the lateral femoral wall fracture. Level of Evidence IV, Case Series.
Keywords: Femoral neck fractures; Fracture fixation, internal; Bone plates; Bone screws
INTRODUCTION
The peritrochanteric fracture is one of the most serious causes of mortality and morbidity in the elderly. Subtrochanteric fractures account for approximately 10-30% of all peritrochanteric fractures, and they affect persons of all ages. 1 , 2 The subtrochanteric region of the femur is generally recognized to be the area of the femur below the inferior border of the lesser trochanter, extending distally 7.5 cm to the junction of the proximal and middle third of the femur. 3 Most frequently, these fractures are seen in two patient populations, namely older osteopenic patients after a low-energy fall and younger patients involved in high-energy trauma. 1 - 3 In elderly patients, minor slips or falls that lead to direct lateral hip trauma are the most frequent mechanism of injury. This age group is also susceptible to metastatic disease that can lead to pathologic fractures. In younger patients, the mechanism of injury is always high-energy trauma, either direct or from axial loading (e.g., a fall from height), which often creates a comminuted fracture.
Early surgical intervention is advocated in the majority of these patients to reduce the complications associated with long-term immobilization. 4 The aim of the surgery is to achieve initial stability and early mobilization of the patients to avoid complications, such as deep vein thrombosis, thrombophlebitis, pulmonary embolism, urinary and lung infection and ulcers. 5 , 6
The difficulty involved in the treatment of this fracture is partly due to the fact that this injury pattern is anatomically different from other proximal femoral peritrochanteric fractures and also to the difficult features of femoral shaft fractures. As a result, it must be treated with specially designed implants that can sustain significant muscular forces for prolonged periods of healing. Not surprisingly, this fracture has significantly higher rates of malunion and nonunion than other femoral fractures. 1 - 3 , 6
A number of treatment alternatives exist, each with its own subset of complications. However, the main treatment choices of femoral subtrochanteric fractures can be divided into two groups, the cepholomeduallary hip nails and the lateral plate-screw systems. 6 - 10 The use of intramedullary nail fixation in peritrochanteric fractures has been increasing, but some problems exist when treating comminuted peritrochanteric fractures. 8 , 9 Traditional devices, such as dynamic hip screws (DHS) and angular blade plates can only provide limited treatment for peritrochanteric fractures. For example, the reoperation rate of DHS and intramedullary nails is reported to be 8.2% and ~24%, respectively. 9 - 11
The lateral trochanteric wall is believed to be an important factor in stabilizing peritrochanteric fractures. 12 keeping the lateral intact or stable can assist fracture healing and greatly reduce the rate of malunion or nonunion. 13 A proximal lateral femur locking compression plate (PFLCP) can provide a stress shield for the lateral trochanteric wall and prevent the lateral migration of proximal fragments. This kind of inner plant may be a choice for subtrochanteric or transverse intertrochanteric fractures. 14
We retrospectively reviewed the clinical results of proximal lateral femur locking plates used in 48 cases of subtrochanteric fractures. The factors that affected clinical results were analyzed. The efficiency of the PFLCP was tested by assessing its ability to maintain radiographic reduction and evaluating its functional outcome according to time-course measurement after the operation.
MATERIALS AND METHODS
Between January 2008 and May 2010, 48 patients were admitted to our institute with subtrochanteric fractures and underwent surgical intervention. To be included in this study, patients were supposed to be, cognitively intact, living in their own home or apartment before fracture. Clinical records and radiographs were reviewed to identify the subtrochanteric fractures. Patients were identified at the time of hospital admission and information was collected. The mean age of the patients was 76 years (range 43 to 85 years). Patients with these criteria were excluded: pathologic fracture, polytraumatic patients associated with ipsilateral pelvis fracture (floating hip) or knee injuries, severe systemic diseases that could prevent the operation.
Two classifications of subtrochanteric fractures were used in this study, the Russell-Taylor classification and the Seinsheimer classification. 15 - 18 However, the AO/OTA classification which was popular in many fields classifies them as 31-A3 (31-A2.3). 16 Patients who underwent surgery met the following criteria: Seinsheimer classification type III-V, or Russell-Taylor classification type II. 18
Detailed information was recorded individually, including blood loss, drainage, length of incision, and duration of image intensification. Patients were revisited at 6 weeks, 3 months, 6 months and 1 year after operation, with clinical and radiographic assessment of the progress of healing and complications. The function of the hip joints was evaluated by the Harris social index and the Parker and Palmer mobility score 1 year after the operation.
Surgical technique
All patients underwent routine laboratory tests and organ function assessment after admission. Arterial blood gas analysis was performed as the baseline assessment for patients who were extremely weak or had heart or pulmonary diseases. Systemic diseases were actively treated. During the perioperative period, fluid infusion was supplied according to physiological need and daily amount lost. Those who had low blood capacity required expansion treatment. The blood sugar and blood pressure were regulated to normal. All patients underwent surgery as soon as the preoperative preparation was finished (mean of 3 days, 2 to 7 days).
Surgery was performed with the patient in supine position on a fracture table in traction. Closed fracture reduction was performed before surgery under fluoroscopic view in the anteroposterior and lateral/axial views and subsequently secured in traction. We abducted, adducted and rotated the lower extremity to reduce the fracture. Achieving proper rotation of the femur with the patella in a horizontal position was important. In highly comminuted and unstable fractures that could not be adequately reduced by traction on a fracture table, we preferred free draping of the lower extremity in the supine position on a radiolucent operating table.
The proximal lateral femur locking compression plate (PFLCP) we used was designed for placement anatomically precontoured to the metaphyseal region of the proximal femur. The proximal part of the plate is diamond-shaped with three holes which were used for insertion of femoral neck screws, while the locked screws go through the femoral neck to the femoral head. The remaining 5-13 screw holes are classical holes, which allow the fixation of the lesser trochanter to the shaft.
A lateral longitudinal incision of about 7.0 cm was made about 2.0 cm below the top of the greater trochanter. After the longitudinal incision of the skin and subcutaneous tissue, we split the fascia of the lateral vastus at its proximal insertion, and the muscle was flipped to visualize the lateral aspect of the proximal femur. For complex and comminuted fractures that could not be reduced with closed reduction, we chose to open and correct displacement under fluoroscopy in two X-ray views. When the fracture was successfully reduced, the plate was placed on the lateral aspect of the proximal femur. The femoral neck pin was inserted into the femoral head in the anterior-posterior view to guide the placement of the plate. The femoral neck screws were approximately in the middle third of the femoral head. The most distal screw was first inserted to maintain the femoral neck-shaft angle. After adjusting the anteversion angle under fluoroscopy, we twisted the remaining screws. In the case of subtrochanteric comminution, we also used screws to fix the free fragments. This allowed a larger area of stress distribution on the plate and screws, which can reduce the strain on the fracture.
All patients had closed suction drainage of the wound and received antibiotic prophylaxis with intravenous injection of 1.5 g of cefuroxime before induction of anesthesia. This was followed postoperatively for two days. Patients were allowed to get out of bed and sit in a wheelchair on the third postoperative day. Standing and walking with a was permitted until the fracture was initially healing. Partial weight bearing started about eight weeks after operation. The actual time was controlled according to the fracture healing extent. Weight bearing was gradually increased to the tolerance level. Patients were evaluated at 6 weeks, 3 months, 6 months and 1 year, postoperatively.
RESULTS
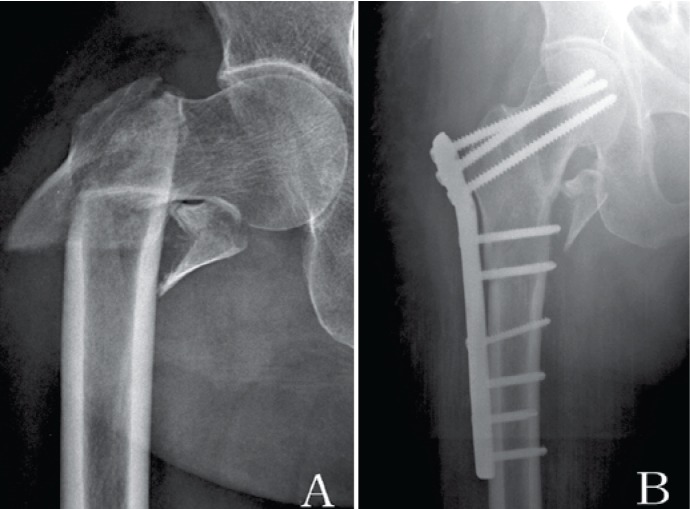
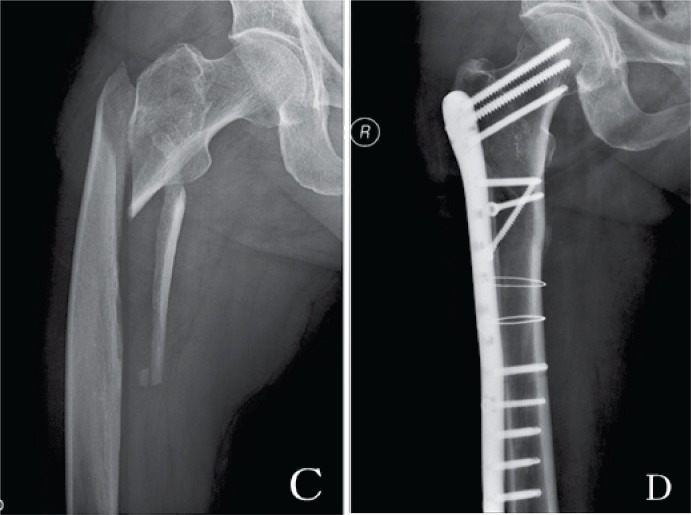
Among all patient admissions, 48 patients underwent surgery. Two patients were lost to follow-up. One patient died three weeks after the operation and the reasons for death were pneumonia and congestive heart failure, which were not related to the surgical intervention or the implant. The remaining 45 patients were followed until fracture union or revision surgery for an average of 16 months (range 6 to 28 months). There was one case of severe infection after operation, which was cured by debridement and intravenous drip of vancomycin. Three cases of superficial infection were observed (1.8%, 3/45) and cured by oral antibiotic therapy and dressing changes. Among the 45 patients who were followed up for more than 6 months, 43 (95.6%) obtained fracture union without further intervention and two patients had implant failure and underwent surgery again. The reason for implant failure was that the two patients started bearing weight four weeks after surgery. Among the 43 cases, 40 fractures (93%) healed with no loss of position at the 3-month follow-up check-up; among the 40 cases, 38 fractures (95%) healed with no loss of position at the 6-month follow-up, and among the 38 cases, all fractures (100%) healed with no loss of position at the 1-year follow-up, including those with severely comminuted fractures. Two patients had femoral neck screw breakage at three months postoperatively, but the fracture healed after delaying the weight-bearing time. Moreover, there were no cases of screw cutting through the femoral head. Figures 1 and 2 show images of classical cases.
Figure 1. Case 1 (A) Female, 78 years, Seinsheimer V, AP radiograph before operation. (B) AP radiograph shows the fracture healed 12 months after surgery.
Figure 2. Case 2 (C) Female, 72 years, Seinsheimer III, AP radiograph before operation. (D) AP radiograph shows the fracture healed 16 months after surgery.
The Harris social index and the Parker and Palmer mobility score were used to evaluate the surgery outcome. The range of score of the Harris social index was 73-95 (86.5±9.8), including 16 excellent cases, 22 good cases, and 5 median cases. Good-excellent rate was 84.4% (38/45). Assessment by the Parker and Palmer mobility score was 3-9 (7.4±2.1).
DISCUSSION
Applied anatomy of the subtrochanteric region
The subtrochanteric region of the femur consists primarily of cortical bone. The femoral head and neck are anteverted approximately 10°~15° in relation to the plane of the femoral shaft. The piriformis fossa lies at the base of the neck and is oriented in line with the femoral shaft. The lesser trochanter is posteromedial, and it is the point of insertion for the psoas and iliacus tendons. The femoral shaft has both an anterior and a lateral bow. The major muscles that surround the hip create significant forces that contribute to fracture deformity. The gluteus medius and minimus tendons attach to the greater trochanter and abduct the proximal fragment. The psoas and iliacus attach to the lesser trochanter and flex the proximal fragment. The adductors pull the distal fragment medially. All of these muscles are well vascularized, and this can lead to significant hemorrhage at the time of injury or during surgical approaches.
In order to approach the proximal lateral femur, the vastus lateralis must be split or elevated off the intermuscular septum close to the large perforating branches of the profunda femoris artery. Division of these vessels can lead to copious bleeding, making surgical exposure difficult. High failure rates sometimes can be partly attributed to bad technique. In some series focusing on unstable fractures treated with hip screws failures are as low as 4%, which in turn highlights that some centers adhere to the proper operative technique. 7 , 17 , 19
The lateral trochanteric wall
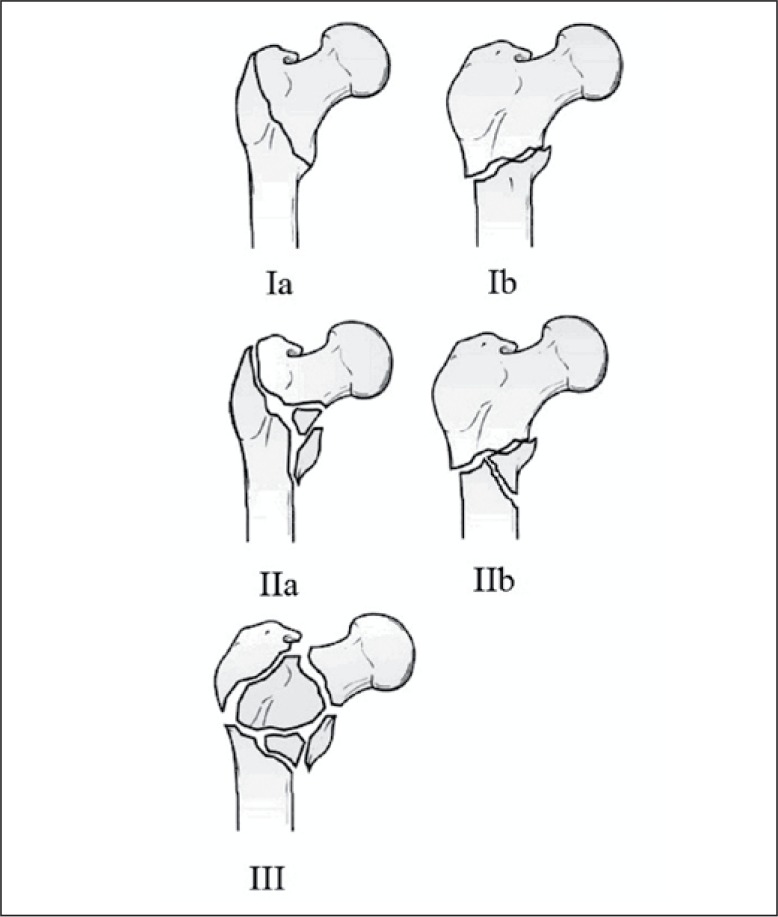
Traditionally, the medial and posteromedial fracture fragments have been considered to be important elements in determining the severity of the peritrochanteric hip fractures. However, the importance of the lateral trochanteric wall in stabilizing the peritrochanteric fractures has been recognized by several authors. 12 , 20 - 22 The lateral wall, first reported by Gotfried 12 , is the proximal extension of the femoral shaft. In an unstable three-part or four-part peritrochanteric hip fracture, the lateral wall is a fragile bony structure. An intact lateral wall plays a key role in the stabilization and fixation of unstable peritrochanteric hip fractures, which is even more important than implant placement such as TAD (tip apex distance). 22 All peritrochanteric fractures are divided into groups according to the damage on the lateral trochanteric wall: type I, intact lateral wall; type II, intact lateral wall but in danger; type III, lateral wall rupture.
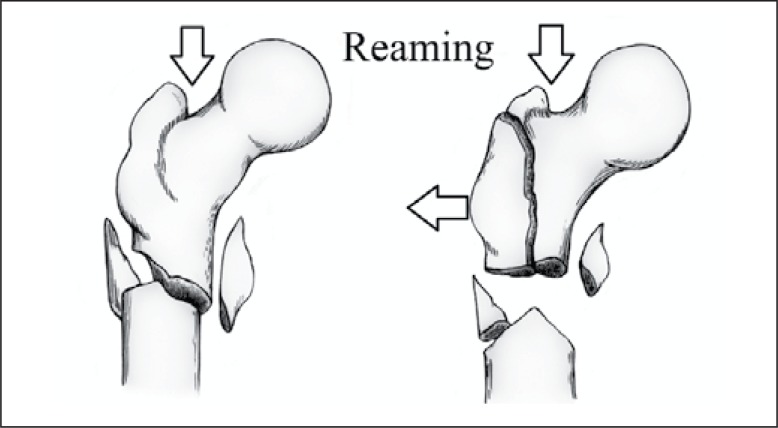
Three subtypes of AO/OTA-31A1 and A2.1, and three subtypes of Seinsheimer II can be classified as type I fracture. In these types of fractures, the greater trochanter is intact with proximal or distal fragment and is not easily refractured during or after surgery. AO/OTA-31A2.2 A2.3 and Seinsheimer III-IV belong to type II, as the lateral wall in these types is intact, but is easily refractured during or after surgery. In type II (AO/OTA-A2.2 A2.3) fractures, the superolateral part of the distal fracture fragment, which corresponds to the lateral part of the greater trochanter, anchors to the proximal fragment like a wall, preventing medial displacement. Fracture of the lateral trochanteric wall occurs in some subtrochanteric fractures or during reaming for the insertion of the DHS screw in the femoral head. 20 It also occurs in reaming for the insertion of the end of intramedullary nails in some Seinsheimer III-IV subtrochanteric fractures. When there is no intact lateral wall to act as a buttress, medialization and subsequent failure is likely. This is due to the decreased contact and ineffective healing of the bone ends. In type III (AO/OTA-A3) fractures, fracture line goes across the vastus lateralis crest, and, in Seinsheimer V fractures, the lateral wall forms a fragment, with no buttress from large aspects, and it is considered ruptured. (Figures 3 and 4)
Figure 3. (Ia, Ib) Lateral wall is intact, the fracture can be fixed with DHS or intramedullary nail. (IIa, IIb) Lateral wall is intact but in danger, and may refracture during operation. (III) Lateral wall is ruptured.
Figure 4. The lateral wall fragment displaces laterally when reaming the piriformis fossa.
Treatment choices of femoral subtrochanteric fractures
The treatment choices of femoral subtrochanteric fractures can be divided into two groups: cepholomeduallary hip nails and lateral plate-screw systems. The use of intramedullary nail fixation in peritrochanteric fractures has been increasing and more and more scholars choose it, because it is easy and fast to apply and can guarantee stability even in inherently unstable fractures. 23 , 24 However, the meta-analysis by Parker and Handoll of all prospective randomized trials comparing intramedullary to extramedullary devices did not support the perceived superiority of nails. They failed to find statistically significant differences in mortality, nonunion, infection, cut-out, blood loss, operative time and radiation time in 3500 patients. 25 The authors of this meta-analysis concluded that the sliding hip screw was a better fixation device for intertrochanteric fractures than the intramedullary nail. But they also admitted that no concrete conclusions could be drawn from existing publications regarding unstable fractures, especially of the reverse obliquity variety. Jiang and his meta-analysis of randomized controlled trials had a similar view. 26 After intramedullary nails fixation, stiffness and a high axial load can result in failure, which is more likely to happen in second-generation cepholomeduallary nails than in the first-generation ones in unstable subtrochanteric fractures. 27 Therefore, evaluation of their results is difficult and controversial especially for subtrochanteric fractures.
The dynamic compression hip screw (DHS) has been a popular method of internal fixation for subtrochanteric fractures. 28 - 32 It provides compression along the femoral neck, and if the reduced fracture is stable, load-sharing between the bone and implant can occur. 33 However, if the fracture is not stable, progressive medial displacement of the femoral shaft can occur, which may result in fixation failure and nonunion. Failures increase sevenfold if medialization of more than 1/3 of the femoral diameter at the fracture site occurs. 34 The most common mode of mechanical failure of the sliding hip screw is the progressive varus collapse of the femoral head with proximal migration and eventual cutting out of the femoral head screw. 32
The concept of the DHS with a trochanteric stabilizing plate is to prevent or reduce medial displacement. However, if the trochanteric stabilizing plate impedes further compression of the fracture before the fracture has become stable, the ends may angulate into varus with lag screws cut-out, loosening or breaking the plate as a result. Even in dealing with intertrochanteric fracture which is proven to be suitable for DHS, failures can exceed 15% when sliding hip screws are used. 34 , 35
In unstable subtrochanteric fractures, such as Seinsheimer IV-V with fragments that cannot be reduced by close reduction in a traction table, proximal lateral femur should be exposed open to reduce the fracture. 36 Medullary nails do not present the same advantage of the minimally invasive procedures. When using cepholomeduallary hip nails to fix comminuted subtrochanteric fractures with the lateral wall ruptured or with a lateral fragment, the reaming of proximal femur would distract the fragments and cause peritrochanteric instability. (Figure 4) The use of binding wire affects the blood supply at the fracture site, causing delayed union or nonunion. So under these circumstances we would choose the PFLCP for the fractures. Combining our experience, we concluded that PFLCP offers the following advantages and disadvantages for femoral subtrochanteric fractures:
The plate is placed at the lateral side of the proximal femur and can provide a stress shield for the lateral fragment, preventing the lateral migration of proximal fragments. 14 , 37 , 38 This characteristic is similar to that of the percutaneous compression plates (PCCP) designed by Gotfried 21 , which can not only prevent rotation of proximal femoral head fragment, but also control the locked compression of the fragments. 39 The use of a DHS or DCS (dynamic condylar screw) provides no stress shielding, and the proximal fragment excessively slides along the axial lag screw. PFLCP, however, has clear differences. As the screws lock with the plate, the system is just like an external fixator frame, which can hold all the major fragments without lateral stress on the greater trochanter fragment. 40 Dissection of periosteum is not always needed, and some minimally invasive techniques can be used to reduce blood loss. As precise reduction and strong fixation are the main objective of the operation, closed reduction may not be able to achieve this goal but open reduction can. However, some problems still exist with the use of the PFLCP. Open reduction of proximal femur causes blood loss and requires proficient technique. The current research on biomechanical stability between femoral head-neck-shaft with intramedullary nails is inadequate, and long-term follow-up is needed to obtain the outcome.
CONCLUSION
The greater trochanter fragment and the lateral trochanteric wall play an important role in stability after implant fixation of subtrochanteric fractures. The PFLCP can be a feasible alternative for the treatment of unstable subtrochanteric fractures because it provides proper fixation of the lateral fragments and prevents the lateral migration of proximal fragments.
Footnotes
Acta Ortop Bras. [online]. 2012;20(6):329- 33. Available from URL: http://www.scielo.br/aob.
Study conducted at the Department of Orthopaedics, Tongji Hospital, Tongji University, Shanghai, PR China.
REFERENCES
- 1. Nieves JW, Bilezikian JP, Lane JM, Einhorn TA, Wang Y, Steinbuch M, et al. Fragility fractures of the hip and femur: incidence and patient characteristics. Osteoporos Int. 2010;21(3):399–408. doi: 10.1007/s00198-009-0962-6. [DOI] [PubMed] [Google Scholar]
- 2. Ekström W, Németh G, Samnegård E, Dalen N, Tidermark J. Quality of life after a subtrochanteric fracture: a prospective cohort study on 87 elderly patients. Injury. 2009;40(4):371–376. doi: 10.1016/j.injury.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 3. Wiss DA, Brien WW. Subtrochanteric fractures of the femur. Results of treatment by interlocking nailing. Clin Orthop Relat Res. 1992;(283):231–236. [PubMed] [Google Scholar]
- 4. Stern R. Are there advances in the treatment of extracapsular hip fractures in the elderly? Injury. 2007;38(Suppl 3):S77–S87. doi: 10.1016/j.injury.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 5. Dobbs RE, Parvizi J, Lewallen DG. Perioperative morbidity and 30-day mortality after intertrochanteric hip fractures treated by internal fixation or arthroplasty. J Arthroplasty. 2005;20(8):963–966. doi: 10.1016/j.arth.2005.04.035. [DOI] [PubMed] [Google Scholar]
- 6. Ehmke LW, Fitzpatrick DC, Krieg JC, Madey SM, Bottlang M. Lag screws for hip fracture fixation: Evaluation of migration resistance under simulated walking. J Orthop Res. 2005;23(6):1329–1335. doi: 10.1016/j.orthres.2005.05.002.1100230614. [DOI] [PubMed] [Google Scholar]
- 7. Kokoroghiannis C, Aktselis I, Deligeorgis A, Fragkomichalos E, Papadimas D, Pappadas I. Evolving concepts of stability and intramedullary fixation of intertrochanteric fractures--a review. Injury. 2012;43(6):686–693. doi: 10.1016/j.injury.2011.05.031. [DOI] [PubMed] [Google Scholar]
- 8. Banan H, Al-Sabti A, Jimulia T, Hart AJ. The treatment of unstable, extracapsular hip fractures with the AO/ASIF proximal femoral nail (PFN)-our first 60 cases. Injury. 2002;33(5):401–405. doi: 10.1016/s0020-1383(02)00054-2. [DOI] [PubMed] [Google Scholar]
- 9. Tyllianakis M, Panagopoulos A, Papadopoulos A, Papasimos S, Mousafiris K. Treatment of extracapsular hip fractures with the proximal femoral nail (PFN): long term results in 45 patients. Acta Orthop Belg. 2004;70(5):444–454. [PubMed] [Google Scholar]
- 10. Saarenpää I, Heikkinen T, Ristiniemi J, Hyvönen P, Leppilahti J, Jalovaara P. Functional comparison of the dynamic hip screw and the Gamma locking nail in trochanteric hip fractures: a matched-pair study of 268 patients. Int Orthop. 2009;33(1):255–260. doi: 10.1007/s00264-007-0458-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Park JH, Lee YS, Park JW, Wang JH, Kim JG. A comparative study of screw and helical proximal femoral nails for the treatment of intertrochanteric fractures. Ortopedia. 2010;33(2):81–85. doi: 10.3928/01477447-20100104-11. [DOI] [PubMed] [Google Scholar]
- 12. Gotfried Y. The lateral trochanteric wall: a key element in the reconstruction of unstable pertrochanteric hip fractures. Clin Orthop Relat Res. 2004;(425):82–86. [PubMed] [Google Scholar]
- 13. Im GI, Shin YW, Song YJ. Potentially unstable intertrochanteric fractures. J Orthop Trauma. 2005;19(1):5–9. doi: 10.1097/00005131-200501000-00002. [DOI] [PubMed] [Google Scholar]
- 14. Hasenboehler EA, Agudelo JF, Morgan SJ, Smith WR, Hak DJ, Stahel PF. Treatment of complex proximal femoral fractures with the proximal femur locking compression plate. Ortopedia. 2007;30(8):618–623. doi: 10.3928/01477447-20070801-18. [DOI] [PubMed] [Google Scholar]
- 15. Rockwood CA, Green DP, Bucholz RW, Heckman JD. Rockwood, Green, and Wilkins' handbook of fractures. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2001. [Google Scholar]
- 16. Senter B, Kendig R, Savoie FH. Operative stabilization of subtrochanteric fractures of the femur. J Orthop Trauma. 1990;4(4):399–405. [PubMed] [Google Scholar]
- 17. Jensen JS, Sonne-Holm S, Tøndevold E. Unstable trochanteric fractures. A comparative analysis of four methods of internal fixation. Acta Orthop Scand. 1980;51(6):949–962. doi: 10.3109/17453678008990900. [DOI] [PubMed] [Google Scholar]
- 18. Coleman NP, Greenough CG, Warren PJ, Clark DW, Burnett R. Technical aspects of the use of the Russell-Taylor reconstruction nail. Injury. 1991;22(2):89–92. doi: 10.1016/0020-1383(91)90061-i. [DOI] [PubMed] [Google Scholar]
- 19. Rao JP, Banzon MT, Weiss AB, Rayhack J. Treatment of unstable intertrochanteric fractures with anatomic reduction and compression hip screw fixation. Clin Orthop Relat Res. 1983;(175):65–71. [PubMed] [Google Scholar]
- 20. Palm H, Jacobsen S, Sonne-Holm S, Gebuhr P, Hip Fracture Study Group Integrity of the lateral femoral wall in intertrochanteric hip fractures: an important predictor of a reoperation. J Bone Joint Surg Am. 2007;89(3):470–475. doi: 10.2106/JBJS.F.00679. [DOI] [PubMed] [Google Scholar]
- 21. Gotfried Y. Percutaneous compression plating of intertrochanteric hip fractures. J Orthop Trauma. 2000;14(7):490–495. doi: 10.1097/00005131-200009000-00005. [DOI] [PubMed] [Google Scholar]
- 22. Gotfried Y. Integrity of the lateral femoral wall in intertrochanteric hip fractures: an important predictor of a reoperation. J Bone Joint Surg Am. 2007;89(11):2552–2553. doi: 10.2106/00004623-200711000-00039. [DOI] [PubMed] [Google Scholar]
- 23. Park SY, Yang KH, Yoo JH, Yoon HK, Park HW. The treatment of reverse obliquity intertrochanteric fractures with the intramedullary hip nail. J Trauma. 2008;65(4):852–857. doi: 10.1097/TA.0b013e31802b9559. [DOI] [PubMed] [Google Scholar]
- 24. Wiss DA, Brien WW. Subtrochanteric fractures of the femur: results of treatment by interlocking nailing . Clin Orthop Rel Res. 1992;(283):231–236. [PubMed] [Google Scholar]
- 25. Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2008;(3):CD000093–CD000093. doi: 10.1002/14651858.CD000093.pub4. [DOI] [PubMed] [Google Scholar]
- 26. Jiang SD, Jiang LS, Zhao CQ, Dai LY. No advantages of Gamma nail over sliding hip screw in the management of peritrochanteric hip fractures: a meta-analysis of randomized controlled trials. Disabil Rehabil. 2008;30(7):493–497. doi: 10.1080/09638280701355538. [DOI] [PubMed] [Google Scholar]
- 27. Ekström W, Karlsson-Thur C, Larsson S, Ragnarsson B, Alberts KA. Functional outcome in treatment of unstable trochanteric and subtrochanteric fractures with the proximal femoral nail and the Medoff sliding plate. J Orthop Trauma. 2007;21(1):18–25. doi: 10.1097/BOT.0b013e31802b41cf. [DOI] [PubMed] [Google Scholar]
- 28. Larsson S, Friberg S, Hansson LI. Trochanteric fractures. Mobility, complications, and mortality in 607 cases treated with the sliding-screw technique. Clin Orthop Relat Res. 1990;(260):232–241. [PubMed] [Google Scholar]
- 29. Massoud EI. Fixation of subtrochanteric fractures : Does a technical optimization of the dynamic hip screw application improve the results? Strategies Trauma Limb Reconstr. 2009;4(2):65–71. doi: 10.1007/s11751-009-0058-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kinast C, Bolhofner BR, Mast JW, Ganz R. Subtrochanteric fractures of the femur. Results of treatment with the 95 degrees condylar blade-plate. Clin Orthop Relat Res. 1989;(238):122–130. [PubMed] [Google Scholar]
- 31. Vaidya SV, Dholakia DB, Chatterjee A. The use of a dynamic condylar screw and biological reduction techniques for subtrochanteric femur fracture. Injury. 2003;34(2):123–128. doi: 10.1016/s0020-1383(02)00319-4. [DOI] [PubMed] [Google Scholar]
- 32. Chirodian N, Arch B, Parker MJ. Sliding hip screw fixation of trochanteric hip fractures: outcome of 1024 procedures. Injury. 2005;36(6):793–800. doi: 10.1016/j.injury.2005.01.017. [DOI] [PubMed] [Google Scholar]
- 33. Haynes RC, Pöll RG, Miles AW, Weston RB. Failure of femoral head fixation: a cadaveric analysis of lag screw cut-out with the gamma locking nail and AO dynamic hip screw. Injury. 1997;28(5-6):337–341. doi: 10.1016/s0020-1383(97)00035-1. [DOI] [PubMed] [Google Scholar]
- 34. Watson JT, Moed BR, Cramer KE, Karges DE. Comparison of the compression hip screw with the Medoff sliding plate for intertrochanteric fractures. Clin Orthop Relat Res. 1998;(348):79–86. [PubMed] [Google Scholar]
- 35. Davis TR, Sher JL, Horsman A, Simpson M, Porter BB, Checketts RG. Intertrochanteric femoral fractures. Mechanical failure after internal fixation. J Bone Joint Surg Br. 1990;72(1):26–31. doi: 10.1302/0301-620X.72B1.2298790. [DOI] [PubMed] [Google Scholar]
- 36. Sanders S, Egol KA. Adult periarticular locking plates for the treatment of pediatric and adolescent subtrochanteric hip fractures. Bull NYU Hosp Jt Dis. 2009;67(4):370–373. [PubMed] [Google Scholar]
- 37. Lundy DW, Acevedo JI, Ganey TM, Ogden JA, Hutton WC. Mechanical comparison of plates used in the treatment of unstable subtrochanteric femur fractures. J Orthop Trauma. 1999;13(8):534–538. doi: 10.1097/00005131-199911000-00003. [DOI] [PubMed] [Google Scholar]
- 38. Zha GC, Chen ZL, Qi XB, Sun JY. Treatment of pertrochanteric fractures with a proximal femur locking compression plate. Injury. 2011;42(11):1294–1299. doi: 10.1016/j.injury.2011.01.030. [DOI] [PubMed] [Google Scholar]
- 39. Langford J, Pillai G, Ugliailoro AD, Yang E. Perioperative lateral trochanteric wall fractures: sliding hip screw versus percutaneous compression plate for intertrochanteric hip fractures. J Orthop Trauma. 2011;25(4):191–195. doi: 10.1097/BOT.0b013e3181ecfcba. [DOI] [PubMed] [Google Scholar]
- 40. Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma. 2004;18(8):488–493. doi: 10.1097/00005131-200409000-00003. [DOI] [PubMed] [Google Scholar]