Abstract
OBJECTIVE
: The primary purpose of this study was to determine the characteristics and outcomes of the patients admitted at our clinics diagnosed with cauda equina syndrome (CES). Secondarily, this study will serve as a basis for other comparative studies aiming at a better understanding of this condition and its epidemiology.
METHODS
: We conducted a retrospective study by reviewing the medical records of patients diagnosed with CES and neurogenic bladder between 2005 and 2011. The following variables were analyzed: gender, age, etiology, topographic level of the lesion, time between disease onset and diagnosis, presence of neurogenic bladder, time between diagnosis and surgery, neurological damage and neurogenic bladder persistence.
RESULTS
: Considering that CES is a rare condition, we were not able to establish statistic correlation between the analyzed variables and the outcomes of the disease. However, this study brought to light the inadequacy of our public health system in treating that kind of patient.
CONCLUSION
: The study shows that despite the well-defined basis for managing CES, we noted a greater number of patients with sequels caused by this condition, than is seen in the literature. The delayed diagnosis and, consequently, delayed treatment, were the main causes for the results observed. Level of Evidence IV, Case Series.
Keywords: Cauda equina; Intervertebral disc displacement; Urinary bladder, neurogenic
INTRODUCTION
Cauda equina syndrome (CES) is classically characterized by compression of the lumbar, sacral and coccygeal nerve roots distal to the end of the medullary cone at the height of vertebrae L1 and L2. 1 Although it is a disease of low incidence in the population, at around 1 case per 33000 to 1 case per 100000 inhabitants, 2 its sequelae still generate high public health costs.
The characteristic clinical signs of the pathology are: intense low back pain frequently accompanied by sciatica, saddle anesthesia, 1 - 3 sphincterian and sexual dysfunction and weakness of lower limbs. 1 , 4 Not all these signs have to be present for the diagnosis. 1 The clinical history and neurological examination lead to the need for diagnostic confirmation through supplementary exams such as computed tomography (CT), and the gold standard, magnetic resonance imaging (MRI). 1 MRI is mandatory to determine the compression topography and the etiology.
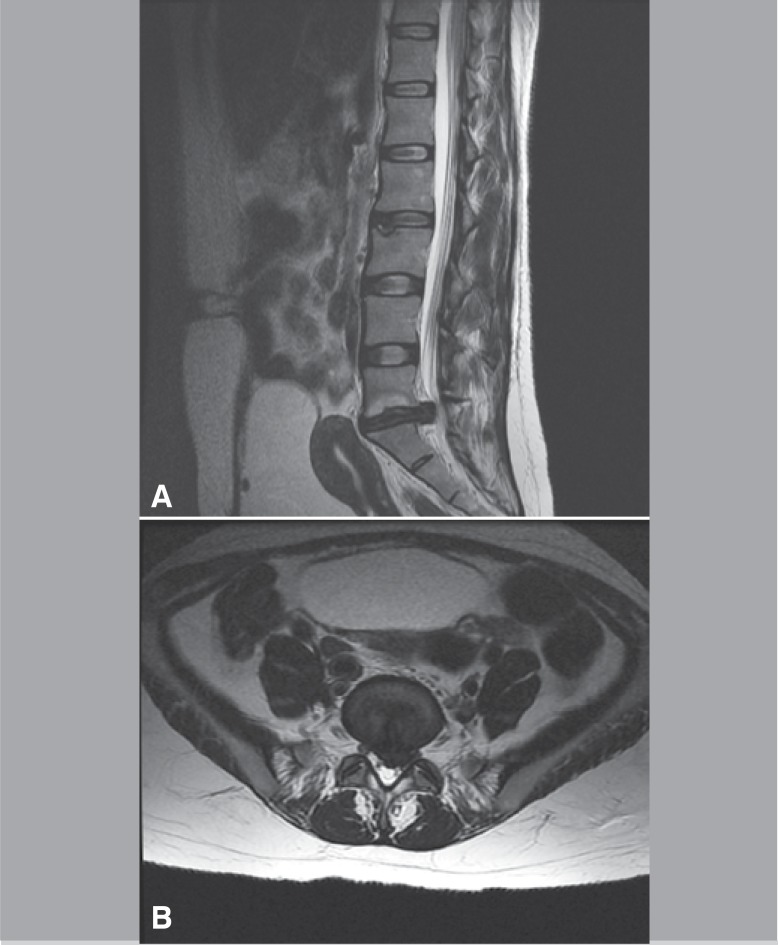
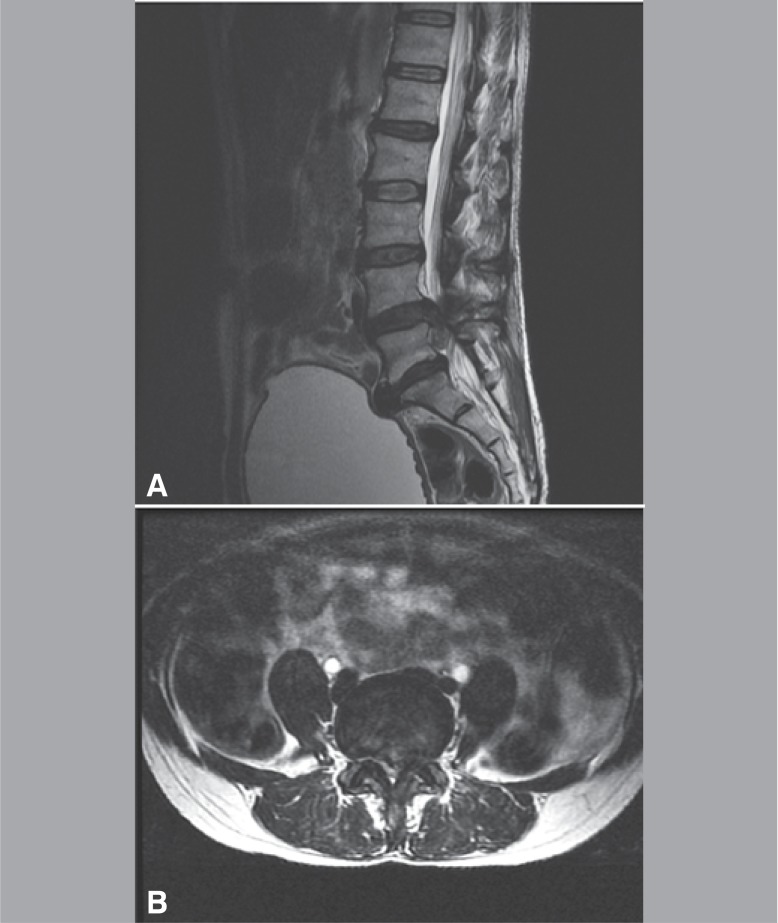
One of the main causes of compression is extruded disc herniation 3 (Figures 1A-B, 2A-B) tumoral lesions (Figure 3), spinal fractures, 5 - 7 canal stenosis, 8 infections, 9 , 10 post-surgical manipulation, post-spinal anesthesia, ankylosing spondylitis and firearm wounds. It requires urgent orthopedic care and its treatment of choice continues to be surgical decompression, 8 , 11 - 13 which, if performed 48 hours before the onset of the symptoms, 14 reduces the neurological damage 2 , 12 , 13 and improves the patient's prognosis.
Figure 1. and B. Magnetic resonance imaging (T1) showing protruding herniated disc at L5-S1 in 37-year-old female patient, hospitalized due to cauda equina syndrome.
Figure 2. and B. Magnetic resonance imaging (T1) evidencing extruded herniated disc at L4-L5 in 49-year-old female patient.
Figure 3. Pathologic fracture of L1 in 55-year-old male patient, admitted with a three-month history of low back pain and presenting neurological deficit and loss of sphincterian control for one week.
The primary goal of this study is to analyze the characteristics of the cases and outcomes of the patients hospitalized for CES treatment by the Spinal Group of IOT-HCFMUSP. Secondarily, this trial will serve as a basis for other comparative studies aiming at a broader understanding of the disease and its epidemiology.
METHODS
We conducted a retrospective study of the medical records of patients hospitalized to treat cauda equina syndrome (CES) in IOT-HCFMUSP in the period from 2005 to 2011. All the medical records with diagnoses classified by the International Disease Code (IDC) under codes G834 and N310/N311/N312, respectively, cauda equina syndrome and neurogenic bladder, were examined. The patients were selected according to criteria of convenience.
Of these medical records, all those that presented spinal cord injury above the level of vertebra T12 as causes were excluded. Patients with a diagnosis of CES confirmed after detailed clinical history and neurological examination upon admission and investigation with computed tomography and magnetic resonance imaging scans of the lumbosacral spine were included. All the cases from the sample had the initial and postoperative physical examinations, and the evolution of the disease well documented in the medical records.
The patients from the sample had the following variables analyzed: sex, age, disease etiology, topographic level of the lesion, time between onset of disease and diagnosis, level of neurological deficit (considered the last normal topographic level with regard to strength and sensitivity), presence of neurogenic bladder, time between diagnosis of CES and the surgical procedure, reversal of deficit or of neurogenic bladder.
In our service, the clinical care, the supplementation with imaging exams (MRI and CT) and the treatment of this pathology - urgent decompression - have very well established and standardized bases. The outcomes (variable) were analyzed by the anamnesis descriptions and initial neurological physical examination (admission in the Emergency Room); of the first postoperative day; and of the outpatient return appointments at two weeks and at 90 to 120 days after hospital discharge. The data were submitted for analysis.
RESULTS
Of the 19 patients included in the study, the vast majority took more than 48 hours, after the onset of symptoms, to be referred to our service. (Table 1)
Table 1. Time up to diagnosis.
| Time | Number of patients (n=19) | % |
|---|---|---|
| more than 48 hours | 15 | 79 |
| less than 48 hours | 4 | 21 |
The most prevalent etiologies evidenced in decreasing order and their respective percentage are contained in Table 2.
Table 2. Etiologies.
| Etiology | Number of patients (n=19) | % |
|---|---|---|
| Hernia | 13 | 69 |
| Tumor | 3 | 16 |
| Trauma | 2 | 10 |
| Vascular | 1 | 5 |
The distribution between genders was seven cases (37%) involving males and 12 cases (63%) involving females. The patients presented average age of 44.16 ± 12.83 years in an age bracket ranging from 22 to 64 years.
The list of the topographic levels affected presented the distribution shown in Table 3.
Table 3. Level of lesion.
| Level of lesion | Number of patients (n=19) | % |
|---|---|---|
| T12 | 1 | 5.3 |
| T12-L1 | 1 | 5.3 |
| L1 | 1 | 5.3 |
| L2-L3 | 1 | 5.3 |
| L3-L4 | 2 | 10.5 |
| L4-L5 | 7 | 36.8 |
| L5-S1 | 6 | 31.6 |
The relationships between symptom onset, diagnosis and surgery times are shown in Table 4. After decompression surgery, we assessed the evolution of the deficit and of the neurogenic bladder on the first postoperative day, in the outpatient return appointment at two weeks and in an outpatient return appointment up to 120 days postoperatively. In the evaluations, we took any neurological recovery in relation to the initial deficit and the complete resolution of the neurogenic bladder to signify an improvement. We obtained the results found in Table 5.
Table 4. Time from onset of the symptoms x diagnosis x surgery.
| Median time | Range | |
|---|---|---|
| Time between onset of CES symptoms and diagnosis |
11 +/- 24 days | 2-90 days |
| Time between diagnosis and surgery | 4 +/- 6 days | 1-25 days |
| Time between onset of symptoms and surgery | 18 +/- 24 days | 5-115 days |
Table 5. Evolution in the postoperative period.
| After decompression and up to 120 days after surgery |
Number of patients (n=19) |
% |
|---|---|---|
| Continuity of initial neurological deficit | 6 | 40 |
| Continuity of neurogenic bladder | 13 | 85 |
DISCUSSION
CES still remains a disease that is often neglected in emergency services, which entails considerable social and financial costs. In our study the patients 79% (n=15) took a much longer time to seek or be referred to our service than the recommended 48 hours. (Figure 3)
Its pathogenesis continues under investigation. 1 The two main hypotheses revolve around mechanical compression or ischemia of the cauda equina. The data encountered in this study show that the main etiology found was disc herniation 69% (13), followed by tumor 16% (3), trauma 10% (2) and vascular 5% (1).
Actually these etiologies somehow combine compressive and/or ischemic mechanisms.
As the most prevalent etiology was disc pathology, consequently the average age bracket (44.16 ± 12.83 years) of our sample corresponds to that in which the occurrence of disc herniation 1 , 6 and the highest prevalence of the topographic and neurological levels found at L4-L5-S1 68.4% (13) were observed the most. 1 , 6
In our casuistry of CES caused by disc herniation, we found a difference between the sexes, men 37% (7) and women 63% (12), yet this difference was not statistically significant, which is consistent with the distribution between genders of this etiology in the literature. 1 , 14 - 16
We observed a considerable time lag between the onset of the symptoms and the final diagnosis of CES (median time:11± 24 days, range: 2-90 days). We believe that health professionals are still very confused about the classic signs and symptoms of the disease, which prevents a fast diagnosis. The Public Health System still suffers with a low availability of supplementary diagnostic resources in the primary health care services, which is another potential cause of delay. In addition there is the low socioeconomic level of several patients, which may postpone the pursuit of medical assistance. We can also mention the overcrowding of the Public Health Services and the long waiting lists as possible aggravating factors of this situation.
Urgent surgical decompression, 17 , 18 even though the exact time limit for the surgery is debated by different authors, 12 , 14 continues to be the most effective treatment. This is the only safe way of preventing the progression of the lesion and its permanent deficits. 19 , 20
In our service patient care is based on a well-defined protocol, with prompt access to supplementary radiological investigation. Nevertheless the patients from this sample did not undergo urgent surgical decompression (median time between diagnosis and surgery: 46 days, range: 1-25 days) in a satisfactory manner. The main possible explanation for the delay in the surgical management of the cases is the high volume of procedures carried out in our surgical center, which involves other orthopedic specialties, besides spinal surgery.
As concerns neurological sequelae, which include permanent sensory-motor deficit and neurogenic bladder, we observed in our study the persistence of the initial deficit in 40% (6) and of the neurogenic bladder in 85% (13) of the patients submitted to the decompression procedure. Owing to the restricted number of cases, we did not obtain statistically significant correlations between variables, yet we observed a tendency for a better prognosis of the patients operated close to the recommended ideal time.
CONCLUSION
The study shows that although the bases for CES conduct are very well defined, we observed a higher number of sequelae caused by the pathology in our service than shown by the literature. The delay in the diagnosis and with a basis hereon, of the performance of the final treatment, was the cause of the high number of sequelae.
Future multicentric studies with a larger number of patients will be able to build up knowledge about CES, and evidence the importance to the Public Health System of optimizing resources to provide adequate care for this disease.
Footnotes
Study conducted in LIM 41 - Laboratory of Medical Investigation of the Musculoskeletal System of the Department of Orthopedics and Traumatology of the School of Medicine of Universidade de São Paulo. São Paulo, SP. Brazil.
Citation: Fuso FAF, Dias ALN, Letaif OB, Cristante AF, Marcon RM, Barros Filho TEP. Epidemiological study of cauda equina syndrome. Acta Ortop Bras. [online]. 2013;21(3):159- 62. Available from URL: http://www.scielo.br/aob.
REFERENCES
- 1. Kostuik JP, Harrington I, Alexander D, Rand W, Evans D. Cauda equina syndrome and lumbar disc herniation. J Bone Joint Surg Am. 1986;68(3):386–391. [PubMed] [Google Scholar]
- 2. Markham DE. Cauda equine syndrome: diagnosis, delay and litigation risk. Curr Orthop. 2004;18:58–62. [Google Scholar]
- 3. Gardner A, Gardner E, Morley T. Cauda equina syndrome: a review of the current clinical and medico-legal position. Eur Spine J. 2011;20(5):690–697. doi: 10.1007/s00586-010-1668-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kennedy JG, Soffe KE, McGrath A, Stephens MM, Walsh MG, McManus F. Predictors of outcome in cauda equina syndrome. Eur Spine J. 1999;8(4):317–322. doi: 10.1007/s005860050180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Harrop JS, Hunt GE Jr, Vaccaro AR. Conus medullaris and cauda equina syndrome as a result of traumatic injuries: management principles. Neurosurg Focus. 2004;16(6): doi: 10.3171/foc.2004.16.6.4. [DOI] [PubMed] [Google Scholar]
- 6. Thongtrangan I, Le H, Park J, Kim DH. Cauda equina syndrome in patients with low lumbar fractures. Neurosurg Focus. 2004;16(6): [PubMed] [Google Scholar]
- 7. Tisot RA, Avanzi O. spinal burst-type fracture on cauda equina area: correlation between neurological function and structural changes on spinal canal. Acta Ortop Bras. 2008;16(2):85–88. [Google Scholar]
- 8. Kostuik JP. Medicolegal consequences of cauda equina syndrome: an overview. Neurosurg Focus. 2004;16(6): doi: 10.3171/foc.2004.16.6.7. [DOI] [PubMed] [Google Scholar]
- 9. Cohen DB. Infectious origins of cauda equina syndrome. Neurosurg Focus. 2004;16(6): doi: 10.3171/foc.2004.16.6.2. [DOI] [PubMed] [Google Scholar]
- 10. Medeiros RS, Abdo RCT, de Paula FC, Narazaki DK, Correia LS, AraújoMP et al. Treatment of spinal tuberculosis: conservative or surgical? Acta OrtopBras. 2007;15(3):128–131. [Google Scholar]
- 11. Gleave JR, Macfarlane R. Cauda equina syndrome: what is the relationship between timing of surgery and outcome? Br J Neurosurg. 2002;16(4):325–328. doi: 10.1080/0268869021000032887. [DOI] [PubMed] [Google Scholar]
- 12. Hussain SA, Gullan RW, Chitnavis BP. Cauda equina syndrome: outcome and implications for management. Br J Neurosurg. 2003;17(2):164–167. doi: 10.1080/0268869031000109098. [DOI] [PubMed] [Google Scholar]
- 13. O'Laoire SA, Crockard HA, Thomas DG. Prognosis for sphincter recovery after operation for cauda equina compression owing to lumbar disc prolapse. Br Med J (Clin Res Ed) 1981;282(6279):1852–1854. doi: 10.1136/bmj.282.6279.1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ahn UM, Ahn NU, Buchowski JM, Garrett ES, Sieber AN, Kostuik JP. Cauda equine syndrome secondary to lumbar disc herniation: a meta-analysis of surgical outcomes. Spine (Phila Pa 1976) 2000;25(12):1515–1522. doi: 10.1097/00007632-200006150-00010. [DOI] [PubMed] [Google Scholar]
- 15. Shapiro S. Medical realities of cauda equina syndrome secondary to lumbar disc herniation. Spine (Phila Pa 1976) 2000;25(3):348–351. doi: 10.1097/00007632-200002010-00015. [DOI] [PubMed] [Google Scholar]
- 16. Busse JW, Bhandari M, Schnittker JB, Reddy K, Dunlop RB. Delayed presentation of cauda equina syndrome secondary to lumbar disc herniation: functional outcomes and health-related quality of life. CJEM. 2001;3(4):285–291. doi: 10.1017/s1481803500005789. [DOI] [PubMed] [Google Scholar]
- 17. McCarthy MJ, Aylott CE, Grevitt MP, Hegarty J. Cauda equina syndrome: factors affecting long-term functional and sphincteric outcome. Spine (Phila Pa 1976) 2007;32(2):207–216. doi: 10.1097/01.brs.0000251750.20508.84. [DOI] [PubMed] [Google Scholar]
- 18. Qureshi A, Sell P. Cauda equina syndrome treated by surgical decompression:the influence of timing on surgical outcome. Eur Spine J. 2007;16(12):2143–2151. doi: 10.1007/s00586-007-0491-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kohles SS, Kohles DA, Karp AP, Erlich VM, Polissar NL. Time-dependent surgical outcomes following cauda equina syndrome diagnosis: comments on a meta-analysis. Spine (Phila Pa 1976) 2004;29(11):1281–1287. doi: 10.1097/00007632-200406010-00019. [DOI] [PubMed] [Google Scholar]
- 20. de César Netto C, Gaia LF, Sattin AA, Cristante AF, Marcon RM, Barros TE, Filho, et al. Effects of decompression time after spinal cord injury on neurologic recovery in wistar rats. Acta Ortop Bras. 2010;18(6):315–320. [Google Scholar]