Abstract
OBJECTIVES
: Pelvic reconstruction after tumor resection is challenging.
METHODS:
A retrospective study had been preformed to compare the outcomes among patients who received pelvic reconstructive surgery with allogeneic bone graft after en bloc resection of pelvic tumors and patients who received en bloc resection only.
RESULTS:
Patients without reconstruction had significantly lower functional scores at 3 months (10 vs. 15, P = 0.001) and 6 months after surgery (18.5 vs. 22, P = 0.0024), a shorter duration of hospitalization (16 day vs. 40 days, P < 0.001), and lower hospitalization costs (97,500 vs. 193,000 RMB, P < 0.001) than those who received pelvic reconstruction. Functional scores were similar at 12 months after surgery (21.5 vs. 23, P = 0.365) with no difference in the rate of complications between the two groups (P > 0.05).
CONCLUSIONS
: Pelvic reconstruction with allogeneic bone graft after surgical management of pelvic tumors is associated with satisfactory surgical and functional outcomes. Further clinical studies are required to explore how to select the best reconstruction method. Level of Evidence IV, Case Series.
Keywords: Pelvic neoplasms; Reconstruction; Transplantation, homologous; Retrospective studies
INTRODUCTION
Osteosarcoma, Ewing's sarcoma, and giant cell tumors of the bone frequently occur in the pelvis. Schwameis et al. 1 reported that among 340 cases of primary malignant bone tumors registered in the Vienna Bone Tumor Center, 9% were pelvic tumors. Pelvic tumors have an occult onset and usually involve a large area. These factors, in combination with the complex anatomical structure of the pelvis, make treatment, especially surgical treatment, complex and challenging. Surgical treatment of pelvic tumors primarily includes ablative methods (hemipelvic resection or modified hemipelvic resection and amputation) and a limb salvage procedure with or without postoperative reconstruction. 2 - 6 Studies have found that the 5-year survival rate is not statistically different between reconstructive surgery with radio- and chemotherapy and non-reconstructive amputation; however, patients who undergo reconstructive surgery with radio- and chemotherapy have a better functional prognosis. 7 , 8 Therefore, limb salvage procedures and functional reconstruction after resection of pelvic tumors are being performed more commonly. 1 , 6 , 9 Further research is clearly needed; however, to determine if outcomes are better with limb salvage procedures.
The purpose of this study is to compare the outcomes of patients who received pelvic reconstructive surgery with allogeneic bone grafts after en bloc resection of pelvic tumors with the outcomes of patients who received en bloc resection only.
MATERIALS AND METHODS
The clinical data of patients who were diagnosed and treated by the same surgeon in the Department of Orthopedics at the PLA General Hospital and received en bloc resection of pelvic tumors with or without functional reconstruction between January 2008 and June 2009 were retrospectively reviewed. This study was approved by the Institutional Review Board of the PLA General Hospital. The requirement of informed patient consent was waived because of the retrospective nature of the study.
Patients who could not complete follow-up treatment (e.g., chemotherapy) or who were unwilling to cooperate with follow-up were excluded. Tumor resections were classified according to the Enneking pelvic tumor resection scheme. 10 , 11 Type I resections are those involving the ilium; type II, those involving the acetabular bone; type III, those involving the pubis and ischium; and type IV, those involving the unilateral sacrum. All patients were treated in accordance with international recognized guidelines, such as those from the American Academy of Orthopedic Surgeons (AAOS) for surgical treatment of giant cell tumors. More complex tumor removal and reconstruction is sometimes necessary in situations where the tumor has caused excessive damage or recurred. In this study, all patients had cortical bone fractures and were therefore not suitable candidates for intralesional procedures.
The range of tumor resection and the type of reconstruction were determined according to preoperative magnetic resonance imaging (MRI) findings. Osteotomy was performed at least 2 cm from the tumor and edge of edema as determined by MRI. Appropriate operative approaches were used according to the tumor location. An arc incision along the iliac crest was used for type I resections; a horn-in-reverse incision was used for type II resections; an abdominal wall transverse incision was used for type III resections; and an arc incision at sacroiliac joint was used for type IV resections. Combined incisions were used when necessary. For reconstruction after resection of a tumor involving the sacroiliac joint, sacroiliac joint fixation with transdermal sacral lag screws was performed. All patients receive perioperative antibiotics (cephalosporin and vancomycin).
Deep frozen pelvic bone allografts were provided by the bone bank of the Orthopedic Institute of the PLA General Hospital. With consents from family members, allografts were originally obtained from donation of deceased individuals who were tested for hepatitis B and syphilis and were processed according to American Academy of Orthopedic Surgeons recommendations (http://www.aaos.org/news/aaosnow/may11/research7.asp). For matching of allogeneic bone to the bone defect, all patients underwent preoperative X-ray and MRI to assess pelvic size and possible resection. Two complete pelvic halves were preselected for each patient according to the preoperative assessments and the most appropriate allograft was selected during surgery with reference to the resection condition of the pelvis.
Steel and screw internal fixation systems were provided by the International Association of Internal Fixation AO/ASIF. Artificial hip prostheses were provided by Waldemar Link GmbH&Co. Tripterygiumwilfordii was routinely prescribed to control rejection in all patients who received allograft reconstruction. Tripterygiumwilfordii improves immune functions to reduce rejection without causing damage to allogeneic bone transplant.
Outcome measures included survival during follow-up period, and functional recovery as assessed according to the international Musculoskeletal Tumor Society (MSTS) tumor functional scoring standard. 12 All patients had follow-up examinations at 3, 6, and 12 months after surgery. Data from the most recent follow-up was used for statistical analysis.
Statistical Analysis
Due to the small sample size, data were compared between the groups by Mann-Whitney U test for continuous variables and Fisher's exact test for categorical variables. Data are presented as a median (interquartile range [IQR]) for continuous data and number (percentage) for categorical data. All statistical assessments were two-sided and evaluated at the 0.05 level of significant difference. Statistical analyses were performed using SPSS 15.0 statistics software (SPSS Inc, Chicago, IL).
RESULTS
A total of 19 patients with primary pelvic tumors who received en bloc resection of pelvic tumors between January 2008 and June 2009 were included in this study. Among these patients, 9 received allograft reconstruction (8 females and 1 male; median age = 38 years, IQR: 34, 40 years). The resection only group had 10 patients (8 females and 2 males) a median age of 35 years (IQR: 26, 44 years). The demographic and disease characteristics of the patients are presented in Table 1. The two groups were similar with respect to age, gender, diagnosis, and Enneking resection type (all, P > 0.05).
Table 1. Demographic data and baseline characteristics.
| Allograft reconstruction (n = 9) |
En bloc resection only (n = 10) |
P value | |
|---|---|---|---|
| Age (years)1 | 38 (34, 40) | 35 (26, 44) | 0.902 |
| Gender2 | 1.000 | ||
| Male | 1 (11.1) | 2 (20.0) | |
| Female | 8 (88.9) | 8 (80.0) | |
| Diagnosis2 | 0.717 | ||
| Giant cell tumor of bone | 6 (66.7) | 3 (30.0) | |
| Chondrosarcoma | 2 (22.2) | 4 (40.0) | |
| Ewing"s sarcoma | 1 (11.1) | 1 (10.0) | |
| Fibrosarcoma | 0 (0.0) | 1 (10.0) | |
| Primitive neuroectodermal tumor |
0 (0.0) | 1 (10.0) | |
| Enneking region2 | |||
| I | 4 (44.4) | 4 (40.0) | 1.000 |
| II | 6 (66.7) | 10 (100.0) | 0.087 |
| III | 3 (33.3%) | 3 (30.0) | 1.000 |
| IV | 1 (11.1) | 0 (0.0) | 0.474 |
Data are presented as median (interquartile range) or number (percentage). 1. Mann-Whitney U test and 2. Fisher's exact test.
In the allograft reconstructive group, 8 patients received allogeneic hemipelvic or partial allogeneic hemipelvic (ilium and acetabular bone) transplantation, 6 patients with involvement of region 2 received allogeneic acetabular bone transplantation and whole hip replacement (a cement fixed acetabular cup was used for the acetabular end and a biological prosthesis was used for the femoral end), 1 patient received allogeneic cortical plate transplantation, and 2 patients received transdermal sacroiliac joint fixation with sacral lag screws to stabilize the posterior pelvic ring. Preoperative iliac vascular embolization was not performed in any patient. Two patients had the superior gluteal artery ligated and all 7 patients with involvement of region 2 had the acetabular branch of the obturator artery ligated. The median surgical time was 4.9 h (IQR: 4.1, 5.6 h) and the median blood loss was 3,000 mL (IQR: 1800, 2600 ml). The surgical time and blood loss were not different between the 2 groups (both, P > 0.05) (Table 2). The median length of follow-up for all patients was 12 months (range: 8-15 months).
Table 2. Functional scores and intra- and postoperative data.
| Allograft reconstruction (n = 9) |
En bloc resection only (n = 10) |
P value | |
|---|---|---|---|
| MSTS1 | |||
| 3 months postoperative | 15 (13, 22) | 10 (9, 11) | 0.001* |
| 6 months postoperative | 22 (18, 27) | 18.5 (16, 21) | 0.024* |
| 12 months postoperative | 23 (20, 25) | 21.5 (20, 23) | 0.365 |
| Operation time (h)1 | 4.9 (4.1, 5.6) | 4.0 (3.3, 4.4) | 0.086 |
| Blood loss (mL)1 | 3000 (2500, 3200) | 2300 (1800, 2600) | 0.093 |
| Length of hospitalization (days)1 |
40 (30, 46) | 16 (14, 17) | <0.001* |
| Cost of hospitalization (*1000 RMB)1 |
193 (164, 201) | 97.5 (95, 103) | <0.001* |
| Complications2 | |||
| Infection | 1 (11.1) | 1 (10.0) | 1.000 |
| Abdominal distention | 1 (11.1) | 0 (0.0) | 0.474 |
*
The functional scores, intra- and postoperative data of the two groups are presented in Table 2. There were significant differences in tumor functional scores (measured by MSTS standard) at 3 and 6 months postoperatively, in surgery duration and the cost of hospitalization between the two groups (all, P < 0.001). Patients who received en bloc resection only had significantly lower functional scores at 3 months (10 vs. 15, P = 0.001) and 6 months after surgery (18.5 vs. 22, P = 0.0024), a shorter duration of hospitalization (16 day vs. 40 days, P < 0.001), and lower cost of hospitalization (97,500 vs. 193,000 RMB, P < 0.001) than those who received allograft reconstruction. There were no differences in tumor functional scores (measured by MSTS standard) at 12 months postoperatively or in the incidence of complications between the two groups (P > 0.05). One patient who received allograft reconstruction developed abdominal distention and incision wound infection and received local wound debridement. One patient in the resection only group developed a postoperative infection and received systemic antibiotics. Images of representative cases that received allograft reconstruction are shown in Figures 1 and 2.
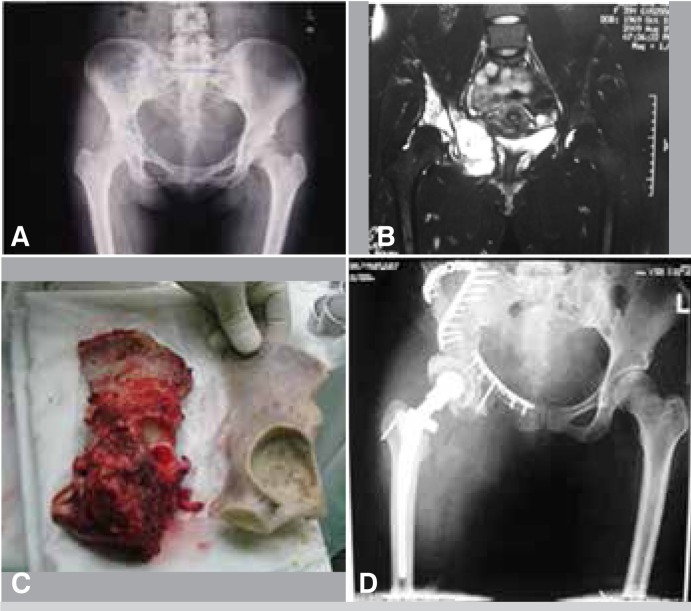
Figure 1. A 40-year-old female was admitted due to pain in the right hip. A) Radiography showed an uneven low density region in the right ilium and acetabulum containing dotted calcification signals. B) T2-weighted magnetic resonance imaging (MRI) showed scattered high signals in the right ilium and acetabulum, and a soft tissue mass within the pelvis. Needle biopsy was consistent with chondrosarcoma. C) The range of tumor resection extended a minimum of 2 cm beyond the edema border as seen on MRI (left, tumor specimen; right, pelvic bone allograft used for reconstruction). D) Postoperative radiography after pelvic reconstruction and total hip arthroplasty. The hip joint was reconstructed using allogeneic ilium and pelvis, fixed with plates and screws, and total hip arthroplasty was performed simultaneously.
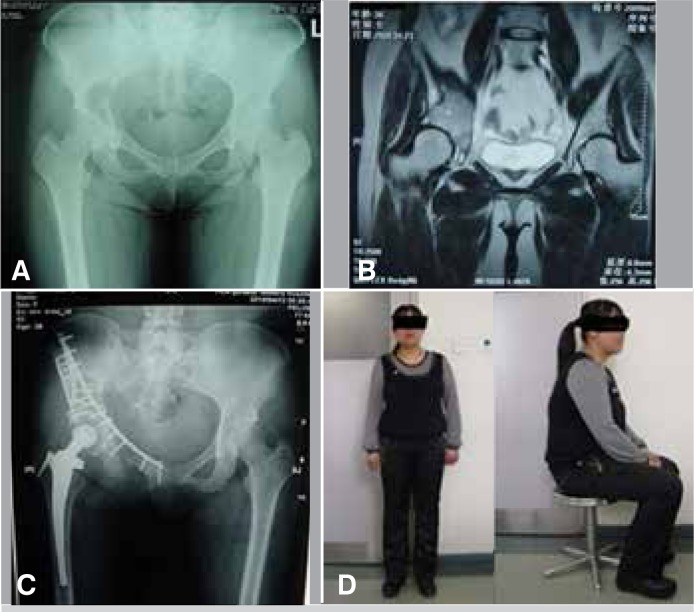
Figure 2. A 36-year-old female with a 6-month history of pain in the right hip while walking. A) Radiography showed osteolytic changes in the right acetabulum. B) T2-weighted magnetic resonance imaging (MRI) showed a lesion protruding into the pelvis and invading the acetabular cartilage. Biopsy was consistent with a giant cell tumor. En bloc tumor resection, pelvic bone allograft, internal fixation, and total hip arthroplasty were performed. C) Radiography at 10-months after surgery showed the prosthesis, implanted bone graft, and plates and screws in the proper locations and bone in growth in the implanted ilium. Bone resorption was observed in the pubic region. D) At 24-months postoperatively, the MSTS score was 24, the patient had nolonger pain and claudication, and had returned to work and resumed normal life activities.
DISCUSSION
Due to the complex anatomy of the pelvis, there is no ideal method for pelvic reconstruction after tumor resection. In the past 20 years, many reconstruction methods including joint fusion, saddle prosthesis, allogeneic bone nail, needle cement, general prosthesis, and constrained prosthesis have been described. 5 , 13 Hoffmann et al. 8 advocated hip exclusion, which is associated with aesthetic defects and progressive pelvic obliquity, although some researchers 5 , 14 believe that structural reconstruction of the pelvic ring after tumor resection can result in satisfactory functional outcomes. Schwameis et al. 1 reported that that the advantages of joint fusion were durability and reduced pain; however, ankylosis and unequal limbs are common. With advancements in surgical techniques and implants, current surgical strategies emphasize repair of the integrity of the pelvic ring and functional recovery. Factors influencing survival of patients with pelvic tumors include tumor type, pathological grading, range of surgical resection, and tumor location. 7 In addition to factors influencing survival, postoperative quality of life should be considered when planning surgical management, especially in patients who are young, have low grade tumors, and a long life expectancy. Although pelvic reconstruction is associated with a high risk of complications, this procedure can significantly improve quality of life by preserving the patient's ability to walk and engage in the normal lifeactivities.
Adequate resection safety margins are difficult to obtain with pelvic tumors because of the complex anatomy of the pelvic region. Patients in this study had tumors which extended beyond the cortical bone. We used MRI with T1-weighted images to identify the tumor boundary and normal tissue. We also identified the boundary of the surrounding soft tissues i.e., iliac muscle (pelvic inner wall), gluteus maximus muscle, gluteus medius muscle, gluteus minimus muscle (pelvic outer wall), and obturator muscle (lower pelvic boundary). In order to ensure complete tumor resection, we first partially or totally removed the gluteus maximus muscle. Vascular and nerve injury can be avoided by locating the greater sciatic foramen and the superior gluteal and inferior gluteal arteries before gluteus maximus resection. The inner wall muscle had excised to facilitate blunt dissection and the inferior wall muscles to clearly strip to avoid damaging the obturator artery.
Our results showed that the allograft reconstruction group had better functional recovery at 3 and 6 months. Hoffmann et al. 8 suggested hip transposition provides the best postoperative long-term function, whereas hemipelvic amputation reduced quality of life. Other authors have reported that allogenic bone transplantation provides better limb function than other types of surgery. 8 , 11 In this study, with the follow-up period of 6 months, the median MSTS function score was 22 points. Our short-term outcomes of pelvic reconstruction were better than that those reported in the literature. 13 Interestingly, there was no difference in MSTS scores 12 months after surgery. Further follow-up is needed to assess longer term outcomes and complications.
Both the length of hospital stay and hospitalization costs were significantly higher in the allograft reconstruction group compared with the en bloc resection group. Neither of these findings is surprising given the greater complexity of preoperative assessment and surgery associated with reconstruction. Further adding to the length of stay and cost is the extended use of postoperative antibiotics and drainage tubes in the allograft reconstruction group. It should be noted that we did not examine after hospitalization costs. These costs could be expected to be different between the groups and affected by functional capacity i.e., the ability to return to normal daily activities.
Many articles 5 , 8 , 13 have reported unsatisfactory functional outcomes following prosthesis implantation and early prosthesis loosening or translocation. This may be because the tumor involved a large portion of the bone, large amounts of muscle were resected leaving insufficient soft tissue support, and extended dead space remained. All the patients in this cohort had extensive soft tissue repair and functional reconstruction of muscles attached to pelvis. Short-term limb function after surgery was satisfactory.
In 2 of the 6 patients who had allogeneic acetabular reconstruction, bone absorption at the pubic end was seen 12 months after surgery; however, limb function and quality of life were not affected. Complications such as bone ingrowth, loosening, and breakage after large allogeneic bone transplantation are problems that remain to be solved. 2 , 8 , 15 - 19
The primary postoperative complications of prosthesis placement combined with allogeneic bone transplantation are wound infection, internal organ and nerve injury, and implant fracture or translocation. 1 , 9 , 20 - 21 The reported incidence of infection after allogeneic bone implantation is 15-50% 14 , 22 with the primary reason for infection being incorrect preparation before implantation. Allogeneic bone tissue used in our cohort was processed at 130°C at 6.8 kg pressure for 3-5 min. This bone tissue had high safety, low immunogenicity, a natural structure, and was easy to apply. Among the 9 patients, only 1 developed an incision wound infection (11%). The infection rate was lower than that reported in the literature. Possible reasons for the low infection rate include improved allogeneic bone preparation (eliminating allogeneic antigens and bacteria), appropriate preoperative disinfection and postoperative wound care, use of a drainage tube for at least 5-7 days, prophylactic antibiotics, skilled surgical technique, and short duration of surgery.
The operative time was not statistically different between the 2 groups, but was clearly greater in the allograft reconstruction group (4.9 h [4.1, 5.6]) as compared to the en bloc resection group (4.0 h [3.3, 4.4]). In both procedures, the tumor resection steps are similar. In allograft reconstruction, the allograft and fixation plates are prepared before the surgery and thus in most cases the reconstructionprocess is smooth and without complications. The most likely reason for the difference in surgical time not being statistically different is the small number of cases. We also noted that the complication rate was similar between the groups, while reconstruction is typically associated with a higher rate of complications than resection. In this study, all surgeries were performed by the same surgeon, and thus the surgical technique including strict hemostasis and the placement of drains were the same for all patients in both groups. In addition, strict protocols were followed for preparation and handling of the grafts. Loosening problems can occur with any prosthesis, though we did not see any in this study up to 12 months. As with the difference in surgical time, it is likely that the similar complication rate is a result of the relatively small number of patients. However, the results do indicate that there are benefits in function and appearance with reconstruction as well as a psychological advantage. Though the complication rate was similar at 12 months, we cannot conclude that both procedures have the same rate of complications, simply because the number of patients was small.
Our study has a number of limitations. These include the retrospective nature and the fact that all procedures were performed at a single institution by the same surgeon. Most importantly, the number of patients was small, and the follow-up duration was only 12 months. Differences in outcomes may become evident with a longer duration of follow-up.
CONCLUSIONS
In summary, we found allograft reconstruction after surgical management of pelvic tumors was associated with satisfactory surgical outcomes, few complications, and good functional outcomes. Additional clinical studies are required to explore how to select the most appropriate reconstruction method. Allogeneic bone transplantation in combination with whole hip replacement is extremely difficult and requires high quality allogeneic bone, surgical experience, and a high level of hospital care.
Footnotes
Study conducted at Department of Orthopedics at the PLA General Hospital, Beijing, China.
Citation: Wang W, Bi WZ, Yang J, Han G, Jia JP . Pelvic reconstruction with allogeneic bone graft after tumor resection. Acta Ortop Bras. [online]. 2013;21(3):150-4. Available from URL: http://www.scielo.br/aob.
REFERENCES
- 1. Schwameis E, Dominkus M, Krepler P, Dorotka R, Lang S, Windhager R, et al. Reconstruction of the pelvis after tumor resection in children and adolescents. Clin Orthop Relat Res. 2002;(402):220–235. doi: 10.1097/00003086-200209000-00022. [DOI] [PubMed] [Google Scholar]
- 2. Abdeen A, Healey JH. Allograft-prosthesis composite reconstruction of the proximal part of the humerus: surgical technique. Pt 2 J Bone Joint Surg Am. 2010;92(Suppl 1):188–196. doi: 10.2106/JBJS.J.00167. [DOI] [PubMed] [Google Scholar]
- 3. Dominkus M, Darwish E, Funovics P. Reconstruction of the pelvis after resection of malignant bone tumours in children and adolescents. Recent Results Cancer Res. 2009;179:85–111. doi: 10.1007/978-3-540-77960-5_8. [DOI] [PubMed] [Google Scholar]
- 4. Guo W, Li D, Tang X, Yang Y, Ji T. Reconstruction with modular hemipelvic prostheses for periacetabular tumor. Clin Orthop Relat Res. 2007;461:180–188. doi: 10.1097/BLO.0b013e31806165d5. [DOI] [PubMed] [Google Scholar]
- 5. Satcher Jr RL, O'Donnell RJ, Johnston JO. Reconstruction of the pelvis afterresection of tumors about the acetabulum. Clin Orthop Relat Res. 2003;(409):209–217. doi: 10.1097/01.blo.0000057791.10364.7c. [DOI] [PubMed] [Google Scholar]
- 6. Wedemeyer C, Kauther MD. Hemipelvectomy- only a salvage therapy? Orthop Ver (Pavia) 2011;3(1): doi: 10.4081/or.2011.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Han I, Lee YM, Cho HS, Oh JH, Lee SH, Kim HS. Outcome after surgical treatment of pelvic sarcomas. Clin Orthop Surg. 2010;2(3):160–166. doi: 10.4055/cios.2010.2.3.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hoffmann C, Gosheger G, Gebert C, Jürgens H, Winkelmann W. Functional results and quality of life after treatment of pelvic sarcomas involving the acetabulum. J Bone Joint Surg Am. 2006;88(3):575–582. doi: 10.2106/JBJS.D.02488. [DOI] [PubMed] [Google Scholar]
- 9. Kitagawa Y, Ek ET, Choong PF. Pelvic reconstruction using saddle prosthesis following limb salvage operation for periacetabular tumour. J Orthop Surg (Hong Kong) 2006;14(2):155–162. doi: 10.1177/230949900601400210. [DOI] [PubMed] [Google Scholar]
- 10. Enneking WF. Local resection of malignant lesions of the hip and pelvis. 1966. Clin Orthop Relat Res. 2002;(397):3–11. doi: 10.1097/00003086-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 11. Enneking WF, Dunham WK. Resection and reconstruction for primary neoplasms involving the innominate bone. J Bone Joint Surg Am. 1978;60(6):731–746. [PubMed] [Google Scholar]
- 12. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;(286):241–246. [PubMed] [Google Scholar]
- 13. Hugate R Jr, Sim FH. Pelvic reconstruction techniques. Orthop Clin North Am. 2006;37(1):85–97. doi: 10.1016/j.ocl.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 14. Harrington KD. The use of hemipelvic allografts or autoclaved grafts for reconstruction after wide resections of malignant tumors of the pelvis. J Bone Joint Surg Am. 1992;74(3):331–341. [PubMed] [Google Scholar]
- 15. Abed YY, Beltrami G, Campanacci DA, Innocenti M, Scoccianti G, Capanna R. Biological reconstruction after resection of bone tumours around the knee:long-term follow-up. J Bone Joint Surg Br. 2009;91(10):1366–1372. doi: 10.1302/0301-620X.91B10.22212. [DOI] [PubMed] [Google Scholar]
- 16. Abdeen A, Hoang BH, Athanasian EA, Morris CD, Boland PJ, Healey JH. Allograft-prosthesis composite reconstruction of the proximal part of the humerus: functional outcome and survivorship. J Bone Joint Surg Am. 2009;91(10):2406–2415. doi: 10.2106/JBJS.H.00815. [DOI] [PubMed] [Google Scholar]
- 17. Biau DJ, Larousserie F, Thévenin F, Piperno-Neumann S, Anract P. Results of 32 allograft-prosthesis composite reconstructions of the proximal femur. Clin Orthop Relat Res. 2010;468(3):834–845. doi: 10.1007/s11999-009-1132-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Friedrich JB, Moran SL, Bishop AT, Shin AY. Free vascularized fibula grafts for salvage of failed oncologic long bone reconstruction and pathologic fractures. Microsurgery. 2009;29(5):385–392. doi: 10.1002/micr.20624. [DOI] [PubMed] [Google Scholar]
- 19. Ogilvie CM, Crawford EA, Hosalkar HS, King JJ, Lackman RD. Long-term results for limb salvage with osteoarticular allograft reconstruction. Clin Orthop Relat Res. 2009;467(10):2685–2690. doi: 10.1007/s11999-009-0726-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Salom EM, Penalver MA. Pelvic exenteration and reconstruction. Cancer J. 2003;9(5):415–424. doi: 10.1097/00130404-200309000-00012. [DOI] [PubMed] [Google Scholar]
- 21. Nazemi TM, Kobashi KC. Complications of grafts used in female pelvic floor reconstruction: Mesh erosion and extrusion. Indian J Urol. 2003;23(2):153–160. doi: 10.4103/0970-1591.32067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ozaki T, Hillmann A, Bettin D, Wuisman P, Winkelmann W. High complication rates with pelvic allografts. Experience of 22 sarcoma resections. Acta Orthop Scand. 1996;67(4):333–338. doi: 10.3109/17453679609002326. [DOI] [PubMed] [Google Scholar]