Recent reports from Australia and Scotland, both reporting peritonitis rates of 0.6 episodes per year at risk, or 1 episode every 20 months, demonstrate clearly that peritonitis is still a major problem for peritoneal dialysis (PD) patients (1,2). The Australian and Scottish reports both also show dramatic differences in peritonitis rates from one program to the next, without a clear explanation (1,2).
To better understand how to prevent peritonitis, a thorough understanding of the pathways that lead to peritonitis is needed. In this commentary, we focus on the literature relating to one of the most avoidable pathways to peritonitis, infection that begins at the exit site of the peritoneal catheter, migrates along the subcutaneous pathway of the catheter, and leads to peritonitis—referred to as “catheter-related peritonitis.”
The association of peritoneal catheter exit-site infections and peritonitis has been recognized since the 1980s, when patients with a history of exit-site infections (ESIs) were shown to be more likely than patients without such a history to develop tunnel infections and peritonitis (3). A subsequent paper by Abraham et al. in 1988 described the natural history of ESIs in patients on continuous ambulatory PD (CAPD) (4). The rate of ESI was 0.83 episodes per year at risk, and one half of the episodes were purulent. The patients with purulent infections were likely to have recurrent ESIs and to eventually develop peritonitis, for a rate of 1.48 episodes of peritonitis per year at risk compared with a rate of 0.57 episodes per year at risk in those with no ESIs. Staphylococcus aureus and Pseudomonas aeruginosa were the organisms that most commonly led to catheter loss in ESI. Therefore, by the late 1980s, the association of ESIs with peritonitis had been firmly established.
Any foreign object extruding from the body—whether a catheter draining ascites in a cirrhotic patient, a catheter for hemodialysis, or a catheter for PD—is prone to colonization and infection. In 1991, Schwartz et al. reported on the concordance of simultaneous effluent and exit-site cultures at the onset of peritonitis (5). The same organism was present both at the exit site and in the effluent in 45% - 55% of peritonitis episodes, but the percentage was significantly higher (85%) when the peritonitis was caused by coagulase-positive Staphylococcus. In many, but not all, of the concordant cases, a clinically overt tunnel exit infection was also present. Triggers for the progression from colonization to infection are not completely understood, but trauma to the exit site, a decline in the patient’s immune status (because of initiation of immunosuppression or malnutrition), or exposure of the exit site to a high bacterial count—P. aeruginosa in a hot tub or heavy nasal colonization with S. aureus for instance—might possibly contribute to the transformation from colonization to infection.
In 1991, Twardowski et al. (6) described the morphology of the peritoneal catheter tunnel in 18 patients whose catheter was removed (10 because of successful transplantation, 6 because of catheter malfunction, 2 because of transfer to hemodialysis, 5 because of tunnel infection combined with peritonitis, and 1 each because of recurrent peritonitis, chronic ESI, and Pseudomonas peritonitis). The tunnels that were infected showed hemorrhagic areas, edema, and many granulocytes. In one particular case in which an ESI developed after trauma to the exit site (and in turn led to refractory peritonitis), the tunnel was filled with an infiltrate of granulocytes, red blood cells, and gram-positive cocci. The appearance of the infected tunnels contrasted with that of tunnels in uninfected patients, which showed giant multinucleated cells, a few mononuclear cells, and collagen fibers mingled with polyester fibers, but no granulocytes. In one patient who clinically had no ESI but who did have peritonitis, the inflammation was close to the deep cuff, indicating the presence of a tunnel infection. In another patient with chronic Pseudomonas ESI without peritonitis, the inflammatory infiltrate was seen in the sinus tract and outer cuff, reaching to the midportion of the intercuff segment; however, it did not involve the deep cuff. This work well illustrated the process of infection extending from the exit site, along the tunnel, to the inner cuff of the peritoneal catheter, and then to the peritoneal space, leading to peritonitis.
In 1996, we defined catheter infection as infection of the exit site, tunnel, or both (but excluding colonization of the biofilm) (7). Catheter-related peritonitis was defined as peritonitis that occurred in temporal conjunction with a catheter infection (either exit-site or tunnel) with the same organism at the exit site and in the effluent (7). In 49% of 87 episodes of catheter-related peritonitis, the ESI was not associated with a clinically obvious tunnel infection (defined as erythema, edema, or tenderness over the subcutaneous portion of the PD catheter). In 56% of cases, the catheter infections were diagnosed when the patient presented with peritonitis attributable to the same organism, although several of the patients had received treatment for ESIs that appeared to resolve. In a home dialysis modality, a peritoneal catheter infection, which generally causes minimal pain, may not bring the patient to the attention of the health care system immediately. On the other hand, symptoms and signs of peritonitis typically cause the patient to present for evaluation. One third of the catheter-related peritonitis episodes were diagnosed with ESI before the development of peritonitis. Another 10% of the ESIs were discovered within 1 week after the onset of peritonitis. That observation is also not surprising, because physicians (some of whom are not so familiar with PD) do not universally conduct a careful examination of the exit site when a patient presents with peritonitis.
Tunnel infections are often clinically occult. Infections that are limited to the exit site are of only minor concern. However, certain organisms have a propensity to migrate along the pathway of the subcutaneous tunnel, leading to peritonitis. S. aureus and P. aeruginosa are particularly troublesome in this regard (7). Vychytil et al. (8) showed that tunnel infections, identified by ultrasonography examination of the subcutaneous tunnel, were present in 36% of patients with ESI, but that the proportion rose to 56% when the organism at the exit site was S. aureus. Once the infection reached the deep cuff of the peritoneal catheter, ultrasonography examination demonstrated that the risk of peritonitis was strikingly elevated unless the catheter was removed (9).
Colonization with S. aureus increases the risk of S. aureus infections in PD patients (10). S. aureus can cause peritonitis by contamination in a patient who is colonized with S. aureus. However, carriage can also lead to colonization of the PD catheter exit site. That colonization can in turn lead to ESI and tunnel infection, and consequently, peritonitis with S. aureus. In 1991, Luzar et al. obtained nose cultures for S. aureus at the start of CAPD in 140 patients and then monitored subsequent PD-related infections over a mean of 10.4 months (10). Of S. aureus ESIs, 92% occurred in the CAPD patients who had a positive nose culture for S. aureus at the start of PD, and all of the S. aureus peritonitis occurred in the carrier group.
Prevention of ESIs has repeatedly been shown to lower the risk of peritonitis (11). The use of antibiotic prophylaxis dramatically lowers the risk of S. aureus ESIs and S. aureus peritonitis. Zimmerman et al. (12) were the first to show that cyclical rifampin (600 mg by mouth daily for 5 days every 12 weeks) leads to a dramatic reduction in S. aureus ESIs. After that study, we performed a single-center, randomized non-inferiority trial comparing the rifampin protocol with mupirocin applied daily as part of routine care of the peritoneal catheter exit site (13). We found that exit-site mupirocin and oral rifampin were equally efficacious and that the rates of S. aureus ESIs and S. aureus peritonitis were dramatically lower than historical rates at our center (data collected prospectively as part of a registry). Subsequently, we undertook a multicenter blinded randomized controlled trial comparing exit-site mupirocin with exit-site gentamicin and found that the latter protocol further lowered the rate of ESIs and peritonitis (14).
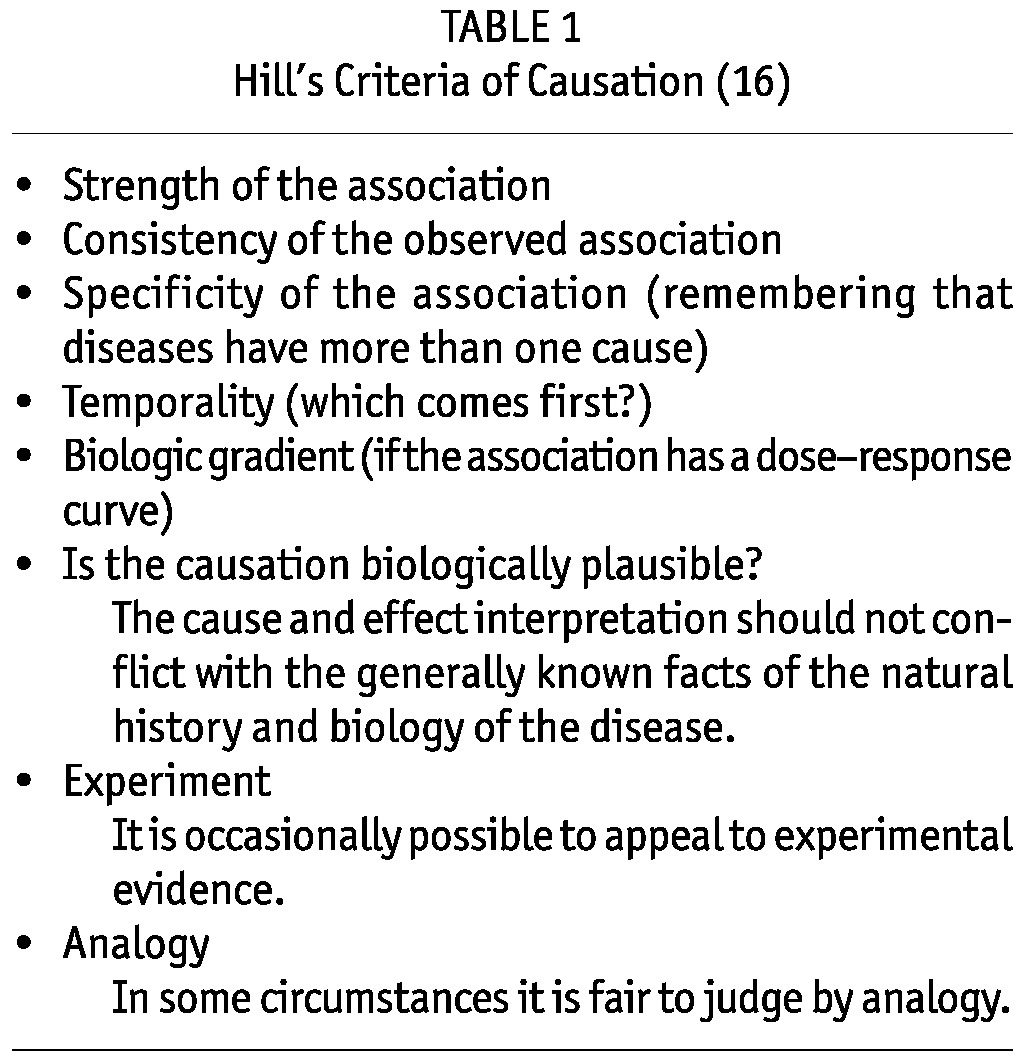
In this issue of Peritoneal Dialysis International, van Diepen and Jassal (15) conclude that ESI and subsequent peritonitis in PD patients are not causally related, but only associated because the Hill postulates are not fulfilled. Table 1 summarizes Hill’s criteria for causation (16). It is important to note that Hill wrote in his seminal paper that “none of my nine viewpoints can bring indisputable evidence for or against the cause-and-effect hypothesis and none can be required as a sine qua non” (16). In view of the overwhelming evidence presented earlier in this commentary to support a causal relationship between infection of the subcutaneous portion of the peritoneal catheter and peritonitis, what are we to make of the conclusion of van Diepen and Jassal that a causal relationship is not supported by the literature?
TABLE 1.
Hill’s Criteria of Causation (16)
A major weakness of the analysis is the limitations placed on the literature reviewed. Because ESIs often lead to peritonitis through tunnel infections, the exclusion of papers on tunnel infection was likely to bias the results from the outset. The analysis included only 9 studies, and yet thousands have been published on the topic, suggesting that the search criteria used by the authors may have been too strict.
To determine causality, the fourth of the Hill criteria has to be met: to be considered causal, the ESI must precede the peritonitis. In a recent paper from Manitoba, patients with an ESI were matched to others without an ESI and were then evaluated for subsequent peritonitis (17). Episodes presenting simultaneously with ESI were excluded from the analysis, as were episodes associated with a tunnel infection. Nonetheless, the authors observed a strong association between ESI and subsequent peritonitis, with a hazard ratio of 1.59 (p >0.001). In addition, the risk of the ESI and the peritonitis being attributed to organisms in the same category was also significant, with an adjusted hazard ratio of 1.55 (p = 0.001). The risk of the appearance of S. aureus peritonitis after S. aureus ESI was especially strong and increased over time [odds ratio of 13 at 6 months (p = 0.02) and of 18 at 9 months (p = 0.007)].
The Manitoba study might underestimate the relationship of ESIs and peritonitis because tunnel infections were again excluded, as were patients presenting simultaneously with ESIs and peritonitis. As we indicated earlier, an ESI might be present, but might not always be diagnosed before the peritonitis episode or even at the time of presentation with peritonitis. Careful questioning will reveal that the ESI was present before the cloudy effluent. It is important that trainees learn not only the importance of obtaining a careful history, but also the necessity of inspecting the exit site for signs of infection whenever a patient presents with peritonitis or is simply making a routine visit to the dialysis center.
To summarize, the literature supports a strong association between ESIs and peritonitis from both an earlier period of PD until more recently. The progression of infection from exit site to tunnel to inner cuff to peritoneal space is biologically plausible. This path to peritonitis is supported both by pathology studies showing inflammation in the tunnel of catheters removed for clinical ESI and peritonitis and by ultrasonography studies of the peritoneal catheter tunnel. Lastly, a reduction in ESIs is associated with a reduction in peritonitis. The literature as a whole therefore fulfills multiple Hill criteria. We urge all PD programs to implement protocols to prevent ESIs in their PD patients and to aggressively treat ESIs that do occur, because those tactics will lower the risk of peritonitis, one of the most serious complications in PD.
Disclosures
JB is a consultant for Baxter Healthcare. BP has no financial conflicts of interest to declare.
References
- 1. Ghali JR, Bannister KM, Brown FG, Rosman JB, Wiggins KJ, Johnson DW, et al. Microbiology and outcomes of peritonitis in Australian peritoneal dialysis patients. Perit Dial Int 2011; 31:651–62 [DOI] [PubMed] [Google Scholar]
- 2. Kavanagh D, Prescott GJ, Mactier RA. on behalf of the Scottish Renal Registry. Peritoneal dialysis-associated peritonitis in Scotland (1999-2002). Nephrol Dial Transplant 2004; 19:2584–91 [DOI] [PubMed] [Google Scholar]
- 3. Piraino B, Bernardini J, Sorkin M. The influence of peritoneal catheter exit-site infections on peritonitis, tunnel infections, and catheter loss in patients on continuous ambulatory peritoneal dialysis. Am J Kidney Dis 1986; 8:436–40 [DOI] [PubMed] [Google Scholar]
- 4. Abraham G, Savin E, Ayiomamitis A, Izatt S, Vas SI, Mathews RE, et al. Natural history of exit-site infection (ESI) in patients on continuous ambulatory peritoneal dialysis (CAPD). Perit Dial Int 1988; 8:211–16 [Google Scholar]
- 5. Schwartz R, Messana J, Starmann B, Weber M, Reynolds J. Preventing Staphylococcus aureus infection during chronic peritoneal dialysis. J Am Soc Nephrol 1991; 2:1085–91 [DOI] [PubMed] [Google Scholar]
- 6. Twardowski ZJ, Dobbie JW, Moore HL, Nichols WK, DeSpain JD, Anderson PC, et al. Morphology of peritoneal dialysis catheter tunnel: macroscopy and light microscopy. Perit Dial Int 1991; 11:237–51 [PubMed] [Google Scholar]
- 7. Gupta B, Bernardini J, Piraino B. Peritonitis associated with exit site and tunnel infections. Am J Kidney Dis 1996; 28:415–19 [DOI] [PubMed] [Google Scholar]
- 8. Vychytil A, Lilaj T, Lorenz M, Horl WH, Haag-Weber M. Ultrasonography of the catheter tunnel in peritoneal dialysis patients: what are the indications? Am J Kidney Dis 1999; 33:722–7 [DOI] [PubMed] [Google Scholar]
- 9. Vychytil A, Lorenz M, Schneider B, Horl WH, Haag-Weber M. New criteria for management of catheter infection in peritoneal dialysis patients using ultrasonography. J Am Soc Nephrol 1998; 9:290–6 [DOI] [PubMed] [Google Scholar]
- 10. Luzar MA, Coles GA, Faller B, Slingeneyer A, Dah GD, Briat C, et al. Staphylococcus aureus nasal carriage and infection in patients on continuous ambulatory peritoneal dialysis. N Engl J Med 1990; 322:505–9 [DOI] [PubMed] [Google Scholar]
- 11. Piraino B, Bernardini J, Brown E, Figueiredo A, Johnson DW, Lye WC, et al. ISPD position statement on reducing the risks of peritoneal dialysis-related infections. Perit Dial Int 2011; 31:614–30 [DOI] [PubMed] [Google Scholar]
- 12. Zimmerman SW, Ahrens E, Johnson CA, Craig W, Leggett J, O’Brien M, et al. Randomized controlled trial of prophylactic rifampin for peritoneal dialysis-related infections. Am J Kidney Dis 1991; 18: 225–231 [DOI] [PubMed] [Google Scholar]
- 13. Bernardini J, Piraino B, Holley J, Johnston JR, Lutes R. A randomized trial of Staphylococcus aureus prophylaxis in peritoneal dialysis patients: mupirocin calcium ointment 2% applied to the exit site versus cyclic oral rifampin. Am J Kidney Dis 1996; 27:695–700 [DOI] [PubMed] [Google Scholar]
- 14. Bernardini J, Bender F, Florio T, Sloand J, PalmMontalbano L, Fried L, et al. Randomized, double-blind trial of antibiotic exit site cream for prevention of exit site infection in peritoneal dialysis patients. J Am Soc Nephrol 2005; 16:539–45 [DOI] [PubMed] [Google Scholar]
- 15. van Diepen ATN, Jassal SV. A qualitative systematic review of the literature supporting a causal relationship between exit-site infection and subsequent peritonitis in patients with end-stage renal disease treated with peritoneal dialysis. Perit Dial Int 2013;35:604–610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hill AB. The environment and disease: association or causation? Proc R Soc Med 1965; 58:295–300 [PMC free article] [PubMed] [Google Scholar]
- 17. Lloyd A, Tangri N, Shafer LA, Rigatto C, Perl J, Komenda P, et al. The risk of peritonitis after an exit site infection: a time-matched, case-control study. Nephrol Dial Transplant 2013; 28:1915–21 [DOI] [PubMed] [Google Scholar]


