Abstract
Actinomyces odontolyticus, a component of normal human flora, has been implicated in cervicofacial actinomycosis, which most commonly involves the perimandibular soft tissues and is characterized by slowly progressive abscess and sinus tract formation. Actinomycosis has rarely been reported to involve the larynx, and the imaging findings of laryngeal involvement have not been reported. We present a case of laryngeal actinomycosis with findings on computed tomography, magnetic resonance imaging, and positron emission tomography.
Cervicofacial actinomycosis (CFA) is a rare but treatable infection that is more commonly seen in patients with poor dental hygiene, immunosuppressed patients, and patients with previous mucosal injury to the upper aerodigestive tract. Actinomycosis rarely involves the larynx and may be mistaken for a mucosal mass. We present a case of laryngeal actinomycosis and illustrate its salient imaging findings on computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET).
CASE DESCRIPTION
A 24-year-old man with a history of inhalational injury and subglottic stenosis had previously undergone multiple airway dilations beginning approximately 1 year before presentation. Two days following his most recent dilation, he presented with acute dyspnea and laryngeal pain. The area over the right thyroid cartilage was tender to palpation. Contrast-enhanced CT imaging of the neck demonstrated diffuse cricoid cartilage enlargement and effacement of adjacent fat planes (Figure 1). Contrast-enhanced MRI of the neck showed increased T2 signal and peripheral nodular enhancement throughout the cricoid cartilage with surrounding inflammation concerning for cricoiditis (Figure 2a, 2b). A pretreatment PET scan demonstrated increased metabolic activity within the cricoid cartilage, suggesting active infection (Figure 2c). The patient underwent urgent tracheostomy and biopsy. A culture of the biopsy specimen grew Actinomyces odontolyticus, a gram-positive anaerobe. The patient received intravenous penicillin for 6 weeks. Subsequent PET-CT imaging revealed resolution of hypermetabolic activity in the larynx and resolution of the soft tissue mass.
Figure 1.
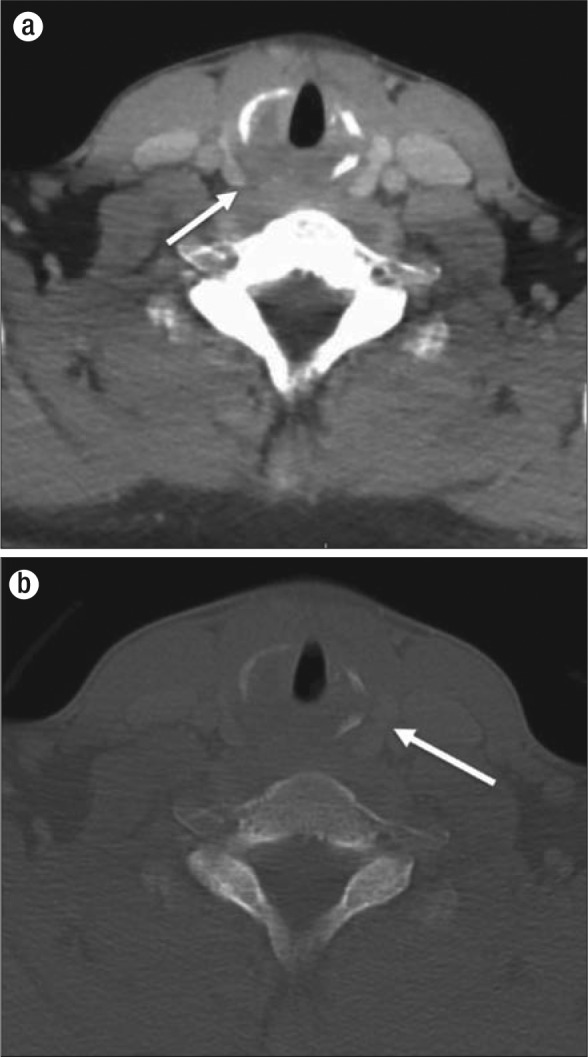
Axial contrast-enhanced CT scans of the neck in (a) soft tissue and (b) bone algorithms demonstrate low attenuation and inflammatory change in the cricoid region (arrow, a) with associated destruction of cricoid cartilage (arrow, b).
Figure 2.
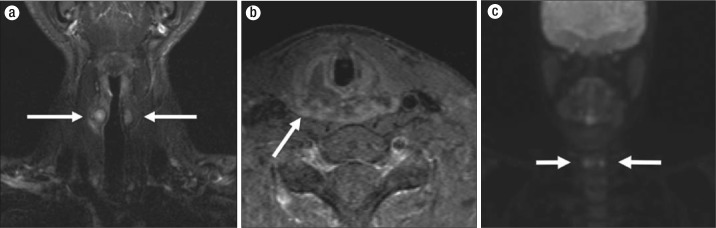
MRI and PET images. (a) Coronal short-tau inversion recovery (STIR) image shows diffuse signal abnormality throughout the cricoid ring, more pronounced on the right (arrows). (b) Fat-saturated T1-weighted postcontrast image demonstrates peripheral enhancement, particularly involving the right posterior cricoid cartilage (arrow). (c) Maximal intensity projection (MIP) reconstruction from a PET scan demonstrates increased metabolic activity throughout the cricoid cartilage (arrows).
DISCUSSION
Actinomycosis was originally described in 1878 by Israel, and the causative organism was isolated in 1891 by Wolfe (1). Actinomyces odontolyticus, a gram-positive anaerobe, is a component of normal human flora. It has been implicated in CFA (1).
CFA has been called a “great masquerader” in diseases of the head and neck (2). Bacteria gain entry via a defect in the mucosa of the upper aerodigestive tract, and infection typically spreads without regard for tissue planes. CFA commonly presents as painless swelling over the mandible, which evolves into multiple abscesses and draining sinus tracts that emit characteristic sulfur granules. Risk factors for the development of CFA include poor dental hygiene, trauma, diabetes mellitus, immunosuppression, and treatment for head and neck neoplasm. Infection is usually treated with a prolonged course of oral penicillin; more complex cases may require surgery (1).
On CT imaging, CFA may present as an ill-defined soft tissue mass with adjacent infiltrative inflammatory change (3–5). Some studies have reported central low attenuation and nonenhancement (4, 5). On MRI, lesions demonstrate elevated T2 and low T1 signal with effacement of adjacent fat planes (4, 5). PET imaging reveals elevated metabolic activity, and PET has been used to monitor response to antibiotic therapy (6). Actinomycosis may be mistaken for a neoplasm on CT, MRI, and PET imaging given its infiltrative and masslike appearance. In one case series, six of seven patients with CFA were initially misdiagnosed with cancer on imaging studies (5).
Laryngeal actinomycosis has been described in case reports, but few have reported imaging findings in the setting of laryngeal involvement (7, 8). Imaging features in our case are similar to those in other head and neck sites: on CT, a masslike soft tissue in the cricoid cartilage with effacement of adjacent fat planes and destruction of cricoid and arytenoid cartilages; on MRI, T2 signal hyperintensity in the cricoid cartilage with infiltration of adjacent fat planes, peripheral enhancement, and central necrosis; and on PET, increased metabolic activity that improves with penicillin therapy.
While rare, actinomycosis remains an important diagnostic consideration in the head and neck, especially when there is a clinical history of mucosal damage. While the imaging features are not specific, CFA is an infection that responds to antibiotics and should be considered before contemplating more invasive treatment approaches.
References
- 1.Smego RA, Foglia G. Actinomycosis. Clin Infect Dis. 1998;26(6):1255–1261. doi: 10.1086/516337. [DOI] [PubMed] [Google Scholar]
- 2.Rankow RM, Abraham DM. Actinomycosis: masquerader in the head and neck. Ann Otol Rhinol Laryngol. 1978;87(2 Pt 1):230–237. doi: 10.1177/000348947808700215. [DOI] [PubMed] [Google Scholar]
- 3.Allen HA, 3rd, Scatarige JC, Kim MH. Actinomycosis: CT findings in six patients. AJR Am J Roentgenol. 1987;149(6):1255–1258. doi: 10.2214/ajr.149.6.1255. [DOI] [PubMed] [Google Scholar]
- 4.Sasaki Y, Kaneda T, Uyeda JW, Okada H, Sekiya K, Suemitsu M, Sakai O. Actinomycosis in the mandible: CT and MR findings. AJNR Am J Neuroradiol. 2013. Aug 8 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 5.Park JK, Lee HK, Ha HK, Choi HY, Choi CG. Cervicofacial actinomycosis: CT and MR imaging findings in seven patients. AJNR Am J Neuroradiol. 2003;24(3):331–335. [PMC free article] [PubMed] [Google Scholar]
- 6.Ho L, Seto J, Jadvar H. Actinomycosis mimicking anastomotic recurrent esophageal cancer on PET-CT. Clin Nucl Med. 2006;31(10):646–647. doi: 10.1097/01.rlu.0000238193.34543.b9. [DOI] [PubMed] [Google Scholar]
- 7.Sari M, Yazici M, Bağlam T, Inanli S, Eren F. Actinomycosis of the larynx. Acta. Otolaryngol. 2007;127(5):550–552. doi: 10.1080/00016480600946954. [DOI] [PubMed] [Google Scholar]
- 8.Artesi L, Gorini E, Lecce S, Mullace M, Sbrocca M, Mevio E. Laryngeal actinomycosis. Otolaryngol Head Neck Surg. 2006;135(1):161–162. doi: 10.1016/j.otohns.2005.03.050. [DOI] [PubMed] [Google Scholar]


