Highlights
► We consider a case of laparoscopic aortic lymphadenectomy for an early ovarian cancer including a comprehensive surgical staging. ► The patient was found to have a congenital anatomic abnormality: a right renal malrotation with an accessory renal artery. ► We used a preoperative CT angiography study to diagnose such anatomical variations and to adequate the proper surgical technique.
Keywords: Kidney malrotation, Lumboaortic lymphadenectomy, Ovarian cancer
Introduction
Kidneys are susceptible to a great morphological variety: number, position, shape, size, rotation and especially vascularization. The rotation has been postulated to be a consequence of unequal branching of successive orders of ureteral trees, with excessive ventral versus dorsal branching. As ureteral branching induces differentiation of the metanephric tissue, more parenchyma develops ventrally and the renal pelvis seems to rotate medially. The most common type of malrotation is the persistent anterior position of the renal pelvis (non-rotation or incomplete rotation). Moreover, there is a strong correlation between renal malrotation and vascularization with the presence of multiple renal arteries in 20–30% of the cases [1].
Adequate and complete surgical intervention, with pelvic and paraaortic lymphadenectomy, is mandatory primary therapy for early ovarian cancer and in case of detection of bulky lymph nodes during surgical exploration of the abdomen, permitting precise staging, accurate diagnosis, and optimal cytoreduction. It is not uncommon to encounter kidney and vascular anomalies during aortic lymphadenectomy. For the surgeon, such anomalies are potentially hazardous and can result in vascular injury [2].
In this study, we report a rare case of renal malrotation with vascular anomaly in a patient who underwent systematic infrarenal paraaortic lymphadenectomy for ovarian cancer.
Case presentation
A 49-year old woman was admitted to another institute in December of 2010 for an ovarian cyst up to 5 cm in diameter discovered occasionally and surgically removed with a laparoscopic right ovariectomy. The full histological report suggested the diagnosis of a clear cell cystadenocarcinoma presumed FIGO stage IA. A month later she was admitted to the Department of Surgery of the “Tor Vergata” University of Rome for a laparoscopic ovarian cancer staging procedure.
A total body CT scan documented a congenital right incomplete inward rotation of the renal pelvis so that the renal pelvis was located anteriorly and had an accessory renal artery which coursed ventrally to the kidney (Fig. 1).
Fig. 1.
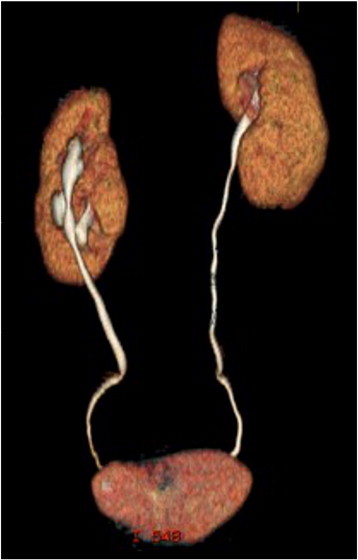
Volume rendering reconstruction of CT scan in 49 year-old woman showing a right laterally malrotated kidney.
The first step of our laparoscopic technique consisted in opening the retroperitoneal spaces according to the following sequence: paravesical space, pararectal lateral space (Latzko), pararectal medial space (Okabayashi), rectovaginal space and vesicovaginal space. The second and third steps were the “en bloc” level 1 and level 2 pelvic lymphadenectomy and the “en bloc” level 3 and level 4 aortic lymphadenectomy respectively, according to Querleu and Morrow classification [3].
To best display the anatomical changes in the region of the right kidney, aortic lymphadenectomy was started in the left para-aortic region, incising the peritoneum covering the upper part of the left common iliac artery and then the subperitoneal areolar tissue was dissected over the aorta until the left renal vein. The sigmoid mesentery was retracted laterally exposing the psoas muscle and left ureter. The left ovarian vein was identified underneath the descendent mesocolon and the confluents of left ovarian and renal veins were isolated. The left ureter was identified and pushed laterally. Following identification of the left ureter and the inferior mesenteric artery, the lymph nodes were dissected from the anterior and lateral aspect of the aorta up to the level of the left renal vein respecting the superior hypogastric nerve. The left ovarian vein and the left renal vein were the lateral and upper limits of the left aortic dissection. The left infundibulopelvic ligament containing the ovarian vessels was pulled through underneath the mesosigmoid and was resected en bloc at their origin at the aorta and left renal vein preserving the inferior mesenteric artery.
After this surgical step, renal and vascular anomalies of the right side were identified and the right aortic nodes over the vena cava and aorta and the inter-aortic nodes were removed. The lymph nodes were placed into an endobag to prevent implantation of tumor cells. Afterwards, type A radical hysterectomy is performed as described by Querleu and Morrow [3] and the open vagina was used to remove nodal packet. Total operative time was 150 min. Blood loss was 1.5 g Hb and there were no intra and post-operative complications. The patient was discharged home on postoperative day 2. In the post-operative period adynamic ileus lasted 12 h.
The histological examination showed that among the 16 aortic lymph nodes removed 2 of the 4 paraaortic right inferior mesenteric and 1 of the 4 from right infra-renal aortic space were sites of residual disease. The resection margins, the infracolic omentum and the 24 pelvic lymph nodes were negative.
On 6 months follow-up the patient is disease-free, she is following the platinum based chemotherapy regimen.
Discussion
Such anomalies are often incidental findings during operative procedures in the paraaortic region and are associated with an increased risk for intraoperative hemorrhage, thromboembolic events or preoperative diagnostic errors.
Renal anomalies, including all malformative pictures, were observed by Anson and Kurth [4] in as few as six (1.2%) cases of 500 successive post-mortem examinations. Anomaly in the present case showing a right laterally malrotated kidney (“reversed rotation”) with a hilum facing anteriorly ﴾90° rotated compared with the fisiological location) and an accessory renal artery which coursed ventrally to the kidney to enter the laterally facing hilum (Fig. 2) that has been reported very infrequently [5].
Fig. 2.
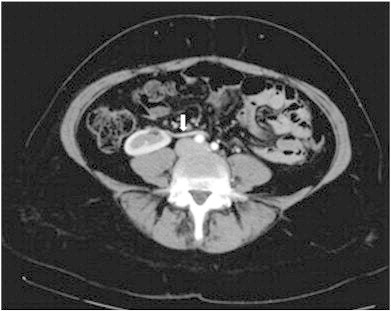
Axial CT scan showing a right laterally malrotated kidney with an accessory renal artery which coursed ventrally to the kidney.
Accessory renal arteries occur unilaterally or bilaterally as a single or a double vessel with a frequency of 9–31.3%. In a study by Laky, examining 230 cadavers a unilateral supranumerary renal artery was found in 31.3% and bilateral supranumerary renal arteries in 11.7%. Bilateral accessory renal arteries can be accompanied by various abnormalities of the ovarian arteries and of the ureter which may lead to hydronephrosis. Accessory lower polar arteries usually originate from the abdominal aorta, run ventrally over the vena cava to the right kidney and directly to the lower pole of the kidney on the left side. In addition, polar arteries may originate from the common iliac artery or the median sacral artery. Since these accessory renal arteries are functional end arteries and do not have collaterals, inadvertent transaction is not accompanied by severe hemorrhage, but leads to infarction of the lower kidney pole [6].
Pelvic and aortic lymphadenectomy is an integral part of staging and surgical treatment of patients with early ovarian cancer. Benedetti-Panici et al. [7] reported urinary and vascular anomalies in five (1.6%) and 42 (13.6%) cases, respectively of 309 patients who underwent open lymphadenectomy for the treatment of cervical, endometrial or ovarian cancer. Preoperative diagnosis was made by intravenous pyelography and computed tomographic scan in 14.9% (seven of 47) of patients with malformations. In 3 (1%) out of these 309 patients abnormalities were diagnosed following a hemorrhagic event.
Preoperative radiologic evaluation of patient waiting for a laparoscopic aortic lymphadenectomy is used to help the surgeon to perform the better dissection, to assess lymph nodes status and to diagnose any possible anatomical varieties that can contribute to complications. Several studies have shown that helical CT angiography can replace excretory urography and renal angiography in this evaluation [8]. We could assert that if we didn't performed CT study we couldn't planned the correct approach in this particular case. So that even if in the past congenital renal defect such as malrotations were considered of little importance nowadays a correct preoperative diagnosis could allow a minimally invasive approach without complications.
In conclusion, kidney malrotation though comparatively rare assumes great importance in view of the present day surgical procedures [9]. Performing a preoperative CT angiography study could improve anatomic knowledge and help the surgeon to plan the surgical procedure and avoid complications.
Conflict of interest statement
The authors declare that they have no competing interests.
References
- 1.Bauer S.B. Anomalies of the kidney and ureteropelvic junction. In: Walsh P.C., Retik A.B., editors. 7th ed. vol. 2. WB Saunders; Philadelphia: 1998. pp. 1728–1733. (Campbell's Urology). (Ch.58) [Google Scholar]
- 2.Klemm P., Fröber R., Köhler C., Schneider A. Vascular anomalies in the paraaortic region diagnosed by laparoscopy in patients with gynaecologic malignancies. Gynecol. Oncol. 2005;96(2):278–282. doi: 10.1016/j.ygyno.2004.09.056. [DOI] [PubMed] [Google Scholar]
- 3.Querleu D., Morrow C.P. Classification of radical hysterectomy. Lancet Oncol. 2008;9:297–303. doi: 10.1016/S1470-2045(08)70074-3. [DOI] [PubMed] [Google Scholar]
- 4.Anson B.J., Kurth L.E. Common variations in the renal blood supply. Surg. Gynecol. Obstet. 1955;100:157–162. [PubMed] [Google Scholar]
- 5.Nathan H., Glezer I. Right and left accessory renal arteries arising from a common trunk associated with unrotated kidneys. J. Urol. 1984;132:7–9. doi: 10.1016/s0022-5347(17)49439-0. [DOI] [PubMed] [Google Scholar]
- 6.Laky D. Anatomicoclinical considerations on ramification anomalies of the renal vessels. Rom. Med. Rev. 1967;11(4):14–22. [PubMed] [Google Scholar]
- 7.Benedetti-Panici P., Maneschi F., Scambia G., Greggi S., Mancuso S. Anatomic abnormalities of the retroperitoneum encountered during aortic and pelvic lymphadenectomy. Am. J. Obstet. Gynecol. 1994;170(1 Pt 1):111–116. doi: 10.1016/s0002-9378(94)70394-9. [DOI] [PubMed] [Google Scholar]
- 8.Behar J.V., Nelson R.C., Zidar J.P., DeLong D.M., Smith T.P. Thin-section multidetector CT angiography of renal artery stents. AJR. 2002;178:1155–1159. doi: 10.2214/ajr.178.5.1781155. [DOI] [PubMed] [Google Scholar]
- 9.Patil S.T., Meshram M.M., Kasote A.P. Bilateral malrotation and lobulation of kidney with altered hilar anatomy: a rare congenital variation. Surg. Radiol. Anat. 2011;33(10):941–944. doi: 10.1007/s00276-011-0826-6. (Dec., Epub 2011 May 29) [DOI] [PubMed] [Google Scholar]


