Highlights
► Mohs' paste is made of a mixture of zinc chloride paste. ► Recent reports show that hemostasis could be achieved in various kinds of cancer. ► Mohs' paste can save a patient's life from fatal genital bleeding.
Keywords: Genital bleeding, Mohs' paste, Uterine cervix
Introduction
Atypical genital bleeding is the most common and serious manifestation in patients with advanced gynecologic malignancies. In the 1930s, Frederic F Mohs originated a method for the chemical fixation of a cutaneous tumor using 20% of zinc chloride (Mohs' paste), which causes necrosis, but preserves microscopic details of the tissue (Mohs et al., 1941). He developed a technique of micrographic tumor serial excision as a chemosurgery technique (Mohs et al., 1941; Swanson, 1983). Nowadays, such a technique has become widely accepted as the treatment option for primary or recurrent cutaneous neoplasms (Swanson, 1983).
Recent reports show that hemostasis could be achieved using Mohs' paste in a malignant wound including unresectable breast cancer and skin metastasis of various kinds of cancer (Kakimoto et al., 2010). We describe a successful treatment using Mohs' paste for life-threatening genital bleeding in a patient with recurrent cervical cancer. This is an important case report with promising results for future patients and this clearly provides evidence that Mohs' paste can save a patient's life from fatal genital bleeding of the uterine cervix.
Case
Before writing this case report, full informed consent was obtained from the patient. This study was conducted in accordance to the Declaration of Helsinki (as revised in Tokyo 2004). In April 2012, a 55-year-old, multiparous woman was urgently referred to our hospital with massive genital bleeding. One year earlier, the patient had undergone concurrent chemo-radiation (pelvic radiation and intra-cavitary radiation) for FIGO stage IIIb squamous cell carcinoma of the uterine cervix. However, she had a relapse in the uterine cervix four months after finishing the initial treatment. She had been treated with systemic chemotherapy using cisplatin and irinotecan. Computed tomography demonstrated the presence of an irregular solid tumor 45 mm in diameter in the uterine cervix. Her height and body weight were 149 cm and 50 kg, respectively.
On admission, serious vaginal bleeding from the cervical tumor continued and the patient complained of pelvic pain. Her mental status was altered because of the pain. She was in a state of hypovolemic shock because of a 1300 mL or more blood loss. Blood pressure and heart rate were 78/42 mm Hg and 120 b.p.m., respectively. Her serum hemoglobin level was 5.4 g/dL and she received 8 units of red blood cell transfusion. Vaginal examination revealed that the tumor was fragile and infiltrating the whole vaginal wall. Copious oozing of blood was observed from the dorsal side of the tumor in the cervix with a penetrating odor. Although a vaginal pack was inserted under intravenous fentanyl administration, the bleeding persisted and exceeded the capacity of the gauze (Fig. 1).
Fig. 1.
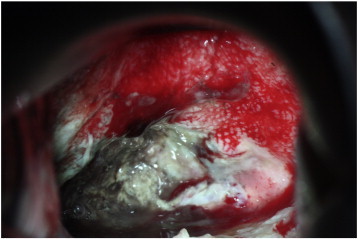
Cervical tumor before applying Mohs' paste. Copious oozing of blood was mainly observed from the dorsal side of the tumor in the cervix.
Twelve hours after admission, Mohs' paste was directly applied to the most actively-bleeding region of the tumor using a large pledget, with care being taken not to apply it to the vagina, and soft pressure was applied to the tumor for a few minutes (Fig. 2). Twenty-four hours later, the pledget was removed and as much paste as possible was wiped from the tumor surface. Complete hemostasis and amelioration of the bad odor were achieved by single direct usage of Mohs' paste. The tumor surface became hard and the vaginal discharge almost disappeared. She was discharged 10 days after admission (Fig. 3). Hemostasis lasted for more than six months and she died of multiple organ failure but had no further vaginal bleeding.
Fig. 2.
Mohs' paste was directly applied to the tumor using a large pledget.
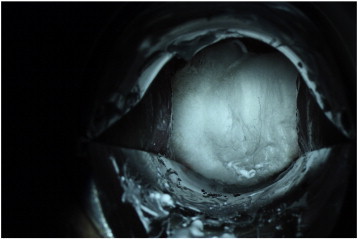
Fig. 3.

Two weeks after applying Mohs' paste.
Comment
Hemostasis for massive genital bleeding is difficult when the vaginal stump or a cervical vascularity neoplasm disintegrates, particularly in progressive patients with recurrent cervical cancer. Tumor infiltration through pathways of lower resistance such as tissue planes, blood vessels, lymphatics, and perineural spaces can lead to bleeding. Angiogenesis factors promote vascularity, and a solid neoplasm often causes massive fatal bleeding due to the destruction of fragile blood vessels (Prommer, 2005).
In general, external palliative radiotherapy is considered when hemostasis cannot be achieved by gauze tampons. Hypogastric artery ligations or uterine artery embolization is also considered as a more invasive treatment for fatal bleeding (Yalvac et al., 2002; Sobiczewski et al., 2002).
Chemosurgery using zinc chloride paste preoperatively with in situ fixation is a process called fixed tissue technique in dermatology (Trost and Bailin, 2011). Although the fixed tissue technique offers a high cure rate, it takes some days to complete. Mohs' Surgery by modifying the fixed tissue technique without using zinc chloride paste is practiced all over the world as part of a multidisciplinary approach to treat skin cancer (Trost and Bailin, 2011). Therefore, many health professionals are unaware of the strong hemostatic effect of zinc-chloride components on bleeding from a neoplasm (Kakimoto et al., 2010). Braun et al. outlined some locations where the fixed tissue method may be the better choice, including (1) squamous cell carcinomas invading deeply and around narrow spaces, (2) lesions on highly vascular structures, such as the penis, and miscellaneous situations for the palliative removal of large, unresectable neoplasms (Braun, 1981).
Mohs' paste is made of a mixture of zinc chloride (50 g), distilled water (25 mL), zinc starch (19 g), and glycerol (15 mL). Zinc chloride in Mohs' paste changes into zinc ions by ulcerative exudate, and then the zinc ions precipitate wound proteins. Tissues, vessels, and cell membranes of bacteria are fixed chemically. Glycerol is used to adjust viscosity. This mixture can be preserved at room temperature in a plastic ointment tub for one year. Mohs' paste softens at body temperature. This change should be taken into account during its application. The preparation should be applied with plastic gloves in order to prevent skin irritation (Kakimoto et al., 2010). Before Mohs' paste application, fentanyl is routinely administered intravenously because penetrative fixation of zinc chloride paste has the effect of normal skin stimulation and often causes irritant contact dermatitis accompanied by pain. Kakimoto et al. (2010) used Mohs' paste in five patients with bleeding due to breast cancer. This paste was effective in all patients including a hemorrhagic shock patient on the first application. Bleeding control was maintained from three weeks to three months or more. Odor and exudates were also reduced.
The eight palliative stage patients who received Mohs' paste as a treatment for continuous genital bleeding showed great improvement in their quality of life (Yanazume et al., in press). To our knowledge using a MEDLINE search (search terms: Mohs paste or Mohs' paste, bleeding or gynecology), this is the first report on the successful application of Mohs' paste for vaginal bleeding. Almost complete hemostasis could be achieved using Mohs' paste in all patients. The effect of Mohs' paste continued for four days to one year. None of the patients died of genital bleeding. There were no side effects, except for pain requiring opioids. This case report has not been included in our previous report. The present case developed massive genital bleeding complicated by hypovolemic shock following anti-cancer chemotherapy. Mohs' paste achieved complete hemostasis with a single application without any complications. Mohs' paste can be easily integrated in outpatient clinic pharmacies because it uses cheap materials. However, we have encountered only a small number of subjects. Further extensive studies including side effects are necessary and warranted.
Conflict of interest statement
None of the authors have a conflict of interest.
Acknowledgments
The authors thank Phillip Allen Suzuki for his critical comments on this paper.
References
- Braun M., III The case for Mohs' surgery by the fixed-tissue technique. J. Dermatol. Surg. Oncol. 1981;7:634–640. doi: 10.1111/j.1524-4725.1981.tb00711.x. [DOI] [PubMed] [Google Scholar]
- Kakimoto M., Tokita H., Okamura T., Yoshino K. A chemical hemostatic technique for bleeding from malignant wounds. J. Palliat. Med. 2010;13:11–13. doi: 10.1089/jpm.2009.0238. [DOI] [PubMed] [Google Scholar]
- Mohs F.E., Sevringhaus E.L., Schmidt E.R. Conservative amputation of gangrenous parts by chemosurgery. Ann. Surg. 1941;114:274–282. doi: 10.1097/00000658-194108000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prommer E. Management of bleeding in the terminally ill patient. Hematology. 2005;10:167–175. doi: 10.1080/10245330500093237. [DOI] [PubMed] [Google Scholar]
- Sobiczewski P., Bidzinski M., Derlatka P. Laparoscopic ligature of the hypogastric artery in the case of bleeding in advanced cervical cancer. Gynecol. Oncol. 2002;84:344–348. doi: 10.1006/gyno.2001.6486. [DOI] [PubMed] [Google Scholar]
- Swanson N.A. Mohs surgery. Technique, indications, applications, and the future. Arch. Dermatol. 1983;119:761–773. doi: 10.1001/archderm.119.9.761. [DOI] [PubMed] [Google Scholar]
- Trost L.B., Bailin P.L. History of Mohs surgery. Dermatol. Clin. 2011;29:135–139. doi: 10.1016/j.det.2011.01.010. (vii) [DOI] [PubMed] [Google Scholar]
- Yalvac S., Kayikcioglu F., Boran N., Tulunay G., Kose M.F., Bilgic S., Haberal A. Embolization of uterine artery in terminal stage cervical cancers. Cancer Invest. 2002;20:754–758. doi: 10.1081/cnv-120003543. [DOI] [PubMed] [Google Scholar]
- Yanazume, Y., Douzono, H., Yanazume, S., Kojima, N., Iio, K., Mukaihara, K., Douchi, T., in press. Clinical usefulness of Mohs' paste for genital bleeding from the uterine cervix or vaginal stump in gynecologic cancer. J. Palliat. Med. [DOI] [PubMed]


