Abstract
Background
Most studies on the ocular manifestations of human immunodeficiency virus (HIV) infection are on cases of acquired immunodeficiency syndrome (AIDS), not including asymptomatic carriers of HIV. With this background, we proceeded to study all the HIV-infected individuals attending our centre, with the aim:
a. To study the ocular manifestations of HIV.
b. To correlate those manifestations with the CD4+ T-lymphocyte counts.
c. To compare our findings with other studies.
Method
A cross-sectional study involving a detailed ocular examination of 321 cases of HIV/AIDS was done. Automated perimetry, digital fundus photography and fundus fluorescein angiography were done for relevant cases. The last 125 cases were subjected to Schirmer's test and tear film break-up time.
Results
We studied 321 male HIV cases (642 eyes), with a mean age of 36.78 years, mean CD4+ count of 276.54 cells/μL, 78.82% of them being on anti-retroviral therapy. Ocular manifestations were seen in 87 out of 321 cases, 72.41% of them being asymptomatic carriers of HIV. The ocular findings seen were conjunctival microvasculopathy, molluscum contagio-sum, dry eye, neuro-ophthalmic manifestations, anterior uveitis, posterior uveitis, and HIV retinopathy, only the last three of which had a significant association with CD4+ counts. The overall prevalence of ocular lesions also had a significant association with CD4+ counts.
Conclusion
Ocular manifestations are common in asymptomatic carriers of HIV. Anterior uveitis, posterior uveitis and HIV retinopathy have a significant association with CD4+ counts and are reliable indicators of low CD4+ count.
Keywords: Asymptomatic carriers, Human immunodeficiency virus, Ocular manifestations
Introduction
A wide spectrum of direct or indirect manifestations of human immunodeficiency virus (HIV) in the eye may occur any time during the natural course of the disease.1 CD4+ T-lymphocyte counts are a reasonable predictor of the risk of ocular complications of HIV infection2; however, the use of anti-retroviral therapy (ART) has allowed a substantial repopulation of T-lymphocytes to occur in many patients.3,4 The recovery of CD4+ T-lymphocytes takes months to years and patients have already had long-lasting depletion of CD4+ T-lymphocyte counts.4,5 A recent report on cytomegalovirus (CMV) retinitis in patients on ART and with CD4+ cells >200 cells/μL suggests that reconstituted CD4+ cells may fail to provide protective immunity. Alternatively, the onset of CMV retinitis preceded the recovery of CD4+ T-lymphocytes.6 Hence, the classical school of thought, of correlating most HIV-related ocular lesions with blood CD4+ cell counts might not be reasonable in the present era of ART. Most of the studies on ocular manifestations of HIV are on patients with acquired immunodeficiency syndrome (AIDS)-defining criteria or with low CD4+ counts, and the association of the ocular findings with the CD4+ counts has not been analysed.7–11 We could not find a study on ocular manifestations in asymptomatic cases detected to be HIV-positive on voluntary screening. Human immunodeficiency virus-positive on voluntary screening.
Hence, a cross-sectional study was carried out in which all the cases attending the HIV-referral centre of our hospital between July 2009 and August 2010 were examined with the aim to:
-
a.
study the ocular manifestations of HIV;
-
b.
correlate the observed manifestations with the CD4+ T-lymphocyte counts;
-
c.
compare our findings with the other similar studies.
Materials and method
All patients reporting to the HIV-referral centre at our hospital were subjected to ophthalmic examination. All were serologically confirmed cases of HIV/AIDS. A total of 321 cases (642 eyes) were studied. The cases were classified according to the centres for disease control and prevention (CDC) classification system for HIV/AIDS which is based on the lowest documented CD4+ cell count and on previously diagnosed HIV-related conditions.
A detailed history was followed by ophthalmic examination which included Snellen's visual acuity, ocular motility, visual field by confrontation test, and automated perimetry whenever required. The eyelids, adnexae, and the anterior segment were examined by torchlight and slit lamp biomicroscope. Posterior segment was examined by indirect ophthalmoscopy after my-driasis. Retinal lesions were studied with digital fundus photography with or without fundus fluorescein angiography (FFA). The CD4+ cell counts, haemogram, biochemical profile, venereal disease research laboratory (VDRL) test, Mantoux test, chest radiograph, and ultrasonography of abdomen of all the cases, and serum TORCH titres of relevant cases were done.
The last 125 cases were subjected to the following two tests, which are indicators of dry eye:
-
a.
Schirmer’s test. The Schirmer’s test strip (5 × 35 mm2) was inserted at the junction of middle and lateral one-third of the inferior fornix of the eye. The wetting of the strip at the end of five minutes was recorded (Fig. 1).
-
b.
Tear film break-up time (TBUT). Fluorescein dye was instilled into the eye (1 mg fluorescein sodium per strip) and the time taken for the appearance of the first random dry spot on the cornea was noted under cobalt blue filtred light of a slit lamp (Fig. 1).
Fig. 1.
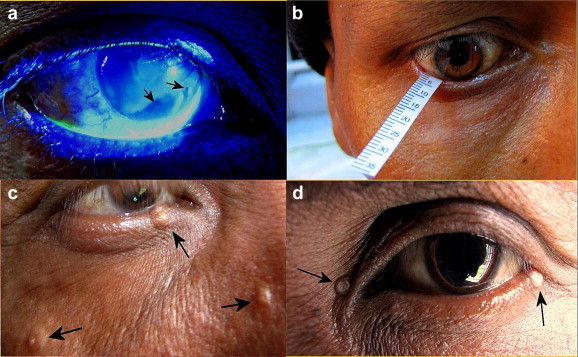
(a) Tear film break-up time test. Arrows indicate the dry spots on the cornea, (b) Schirmer’s test, (c, d) Molluscum contagiosum (indicated by arrows).
A TBUT of < 10 seconds or a wetting of Schirmer’s strip of < 15 mm was taken as indicative of dry eye. The findings were statistically analysed to find the association of the ocular lesions both collectively and individually with the CD4+ count levels.
Results
A total of 321 male cases (642 eyes), 23-53 years of age (mean 36.78 years), with CD4+ counts in the range of 6-1,481 cells/μL (mean 276.54 cells/μL) were studied. Out of the total 321 cases, 253 cases (78.82%) were on ART for an average duration of 2.17 years. The average duration of the disease in this study from the date of detection was 34.16 months. The clinical and the CD4+ count based categories of these patients are outlined in Table 1.
Table 1.
Centres for disease control and prevention staging of human immunodeficiency virus patients studied.
| CD4+ cell-based categories | Clinical categories |
Total | ||||||
|---|---|---|---|---|---|---|---|---|
|
A |
B |
C |
||||||
|
Asymptomatic acute HIV or PGL |
Symptomatic conditions,not A or C |
AIDS-indicator conditions |
||||||
| Cases studied | Cases with ocular lesions | Cases studied | Cases with ocular lesions | Cases studied | Cases with ocular lesions | Cases studied | Cases with ocular lesions | |
| 1. > 500 cells/μL | 35 | 7 | 0 | 0 | 1 | 0 | 36 | 7 |
| 2. 200-499 cells/μL | 126 | 19 | 4 | 0 | 23 | 7 | 153 | 26 |
| 3. < 200 cells/μL | 95 | 37 | 10 | 2 | 27 | 15 | 132 | 54 |
| Total | 256 | 63 | 14 | 2 | 51 | 22 | 321 | 87 |
CDC: centres for disease control and prevention; HIV: human immunodeficiency virus; AIDS: acquired immunodeficiency syndrome; PGL: persistent generalised lymphad-enopathy.
Ocular manifestations excluding dry eye were seen in 87 cases (27.10% of all cases), with many cases out of these 87 having more than one type of lesion. Of these 87 cases, 75 cases (86.21 %) were on ART, and 63 cases (72.41 %) were in the asymptomatic stage A of HIV infection, detected to be HIV-positive on routine voluntary screening. The duration of ART in these 75 cases was two months to nine years (average 2.13 years). The clinical and the CD4+ count based categories of these patients are given in Table 1. A statistically very significant association was found between the levels of CD4+ counts and the overall occurrence of ocular involvement (P = 0.000019), the maximum prevalence being in the CD4+ range of < 200 cells/μL. There was no significant difference between the occurrence of ocular manifestations in the asymptomatic carriers of HIV and symptomatic HIV patients (P = 0.994).
Six cases (1.87% of 321) with a CD4+ range of 76−345 (mean 216) cells/μL had molluscum contagiosum either on the eyelids or on the periorbital skin (Fig. 1). Of these six cases, three had CD4+ count between 200 cells/μL and 499 cells/μL, and the remaining three had CD4+ count <200 cells/μL; five cases were in clinical stage A, and the remaining one in stage C. The association of this finding with the CD4+ count could not be analysed because of the few number of cases with the lesion.
Conjunctival microvasculopathy, seen as capillary dilatation, isolated vascular fragments, irregular vessel calibre, and a granular appearance of blood column within blood vessels was seen in 31 cases (9.66% of 321) with a CD4+ range of 58-560 (mean 220.74) cells/μL (Fig. 2).12,13 Of these 31 cases, one case (3.23%) had CD4 + count >500 cells/μL, 15 cases (48.39%) had CD4+ count between 200 cells/μL and 499 cells/μL, and the remaining 15 (48.39%) <200 cells/μL; 27 cases (87.10%) were in clinical stage A and the remaining four (12.9%) in stage C. The association of these findings with the CD4+ count was not significant (P = 0.302).
Fig. 2.
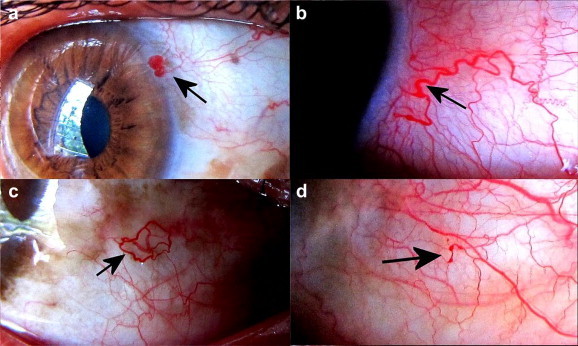
(a−d) Conjunctival microvasculopathy. Arrows indicate isolated vascular segments, comma-shaped vascular dilatations, and tortuosity of vessels.
Signs of healed anterior uveitis in the form of pigmented keratic precipitates/flare in anterior chamber/pigment on anterior capsule of the lens/posterior synechiae or complicated cataract were found in 25 cases (7.79% of 321) with a CD4+ range of 52-576 (mean 232.52) cells/μL (Fig. 3). Of these 25 cases, four cases (16%) had CD4+ count >500 cells/μL, another four (16%) between 200 cells/μL and 499 cells/μL, and the remaining 17 cases (68%) <200 cells/μL; 20 cases (76.92%) were in clinical stage A, one (3.85%) in stage B and the remaining four (15.38%) in stage C. There was a statistically significant association between the occurrence of anterior uveitis and the CD4+ counts (P = 0.004).
Fig. 3.
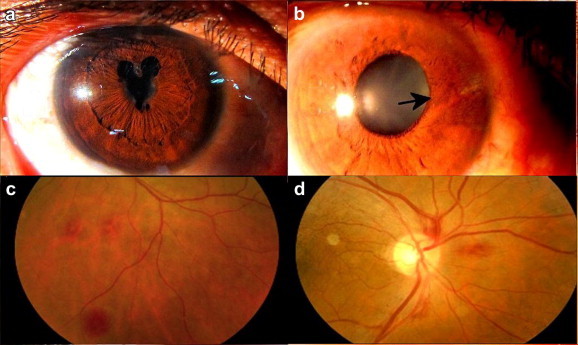
(a) Posterior synechiae in resolved anterior uveitis, (b) arrow indicates sectoral iris atrophy suggestive of herpes zoster iridocyclitis, (d, c) human immunodeficiency virus retinopathy (seen as retinal haemorrhages).
Human immunodeficiency virus retinopathy in the form of soft exudates or retinal haemorrhages was seen in 12 cases (3.74% of 321) with a CD4+ range of 52−837 (mean 169.83) cells/μL (Fig. 3). Of these 12 cases, one case (8.33%) had CD4+ count >500 cells/μL, another two (16.67%) between 200 cells/μL and 499 cells/μL, and remaining nine (75%) <200 cells/μL; seven cases (58.33%) were in clinical stage A, and the remaining five (41.67%) in stage C. This finding also had a significant association with the CD4 + count (P = 0.048).
Eighteen cases (5.6% of 321) with a CD4+ range of 51−269 (mean 156.88) cells/μL had posterior uveitis. Of these 18 cases, four cases (27.78%) had CD4+ count between 200 cells/μL and 499 cells/μL, and remaining 14 cases (72.22%) <200 cells/μL; 11 cases (61.11%) were in clinical stage A, one (5.56%) in stage B and the remaining six (33.33%) in stage C. Of these 18 cases,13 had healed patches of choroiditis or chorioretinitis; one of them with a raised Mantoux test reading of 20 mm and CD4+ count of 269 cells/μL had a healed choroid tuberculoma. However, none of the cases were in the active infective stage needing aggressive management. Three cases had healed retinal vasculitis, one with complicated cataract in both eyes. Two cases had CMV retinitis in both eyes (Fig. 4). Of these two cases, one with a CD4+ count of 54 cells/μL had healed patches of retinitis with complicated cataract in both eyes. The other with a CD4+ count of 51 cells/μL had active CMV retinitis in both eyes with a typical pizza-pie appearance and a complicated cataract in the right eye, and was already on oral valgan-ciclovir. This case had a best corrected distant visual acuity of perception of light in right eye and 20/30 vision in the left eye. None of the cases had immune recovery uveitis (IRU). There was a statistically significant association between the occurrence of posterior uveitis and the CD4+ counts (P = 0.004).
Fig. 4.
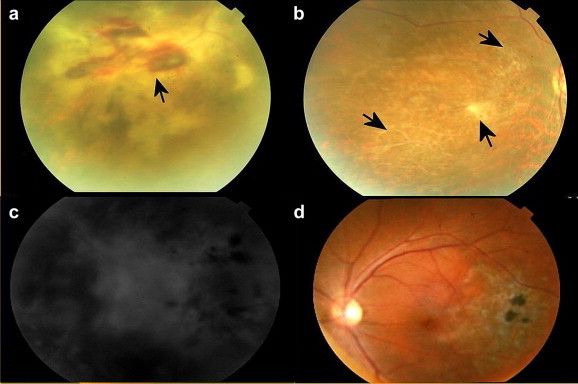
(a) Arrow indicates active cytomegalovirus retinitis, (b) arrows indicate healed lesions of cytomegalovirus retinitis in the other eye of the same patient, (c) fundus fluorescein angiogram in another case of cytomegalovirus retinitis, (d) healed retinochoroiditis.
Three cases (0.93% of 321) with a CD4+ range of 22−222 (mean 143.67) cells/μL had neuro-ophthalmic manifestations. One of these had HIV encephalitis and disseminated tuberculosis (TB), with a CD4+ count of 222 cells/μL, and right congruous homonymous hemianopia. Magnetic resonance imaging (MRI) of brain revealed focal lesions in the left occipital cerebral lobe (Fig. 5A). The second case, had progressive multi-focal leucoencephalopathy and disseminated TB, had a CD4+ count of 187 cells/μL, with multiple bilateral lesions in both temporoparietal and occipital lobes in MRI scan, and corresponding bilateral visual field defects (Fig. 5B). The third case with a CD4+ count of 22 cells/μL had a left-sided third and sixth nerve palsy. The association of these findings with the CD4+ count could not be analysed because of the few number of cases with the lesion.
Fig. 5.
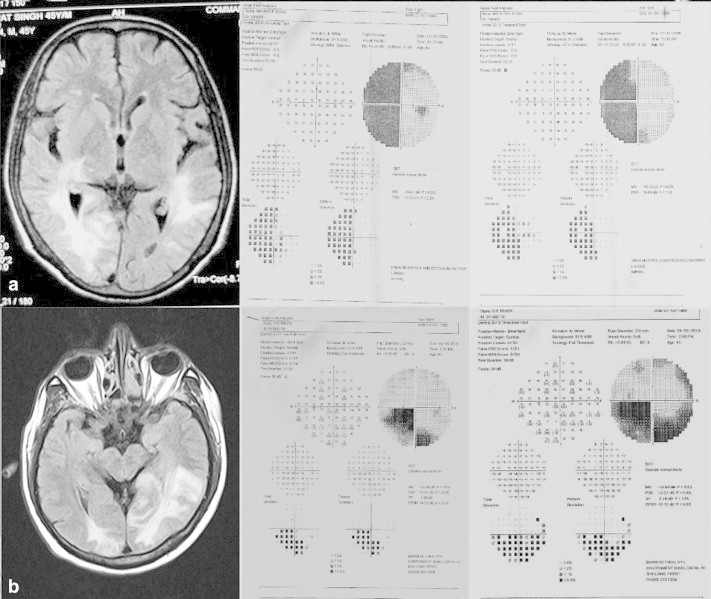
(a) Congruous left homonymous hemianopia with focal lesions in left occipital cortex in a case of human immunodeficiency virus encephalitis, (b) bilateral visual field defects in a case of progressive multiple leukoencephalopathy.
Out of the 125 cases subjected to Schirmer’s test and TBUT, 24 cases (19.2% of 125) with an average CD4+ count of 234.52 cells/μL had a positive Schirmer’s test and a normal TBUT. Sixteen cases (12.8% of 125) with an average CD4+ count of 275 cells/μL had a subnormal TBUT and a normal Schirmer’s test. Five cases (4% of 125) had both, a subnormal TBUT and a positive Schirmer’s test. So a total of 45 cases (36% of 125) with a CD4+ range of 52-837 (average 256.96) cells/μL had a positive Schirmer’s test and/or a subnormal TBUT (Fig. 1). Out of these 45 cases, five cases (11.11%) had CD4+ count >500 cells/μL, 20 cases (44.44%) between 200 cells/μL and 499 cells/μL and another 20 cases <200 cells/μL; 32 cases (25.6%) were in clinical stage A, four (3.2%) in stage B and the remaining nine (7.2%) in stage C. The observed difference in the frequency of these abnormal test results in various CD4+ categories of HIV-positive patients was not statistically significant (P = 0.07). Even though the duration of ART in these cases was known, a detailed drug history was not available with regard to these patients. Hence the association of positive Schirmer’s test or subnormal TBUT with ART could not be statistically analysed.
No significant difference was found between the mean CD4+ counts of the patients with ocular signs and those without ocular signs in the three individual groups based on CD4+ counts (P = 0.39 in > 500, P = 0.15 in 200-499, and P = 0.17 in < 200 group) (Fig. 6).
Fig. 6.
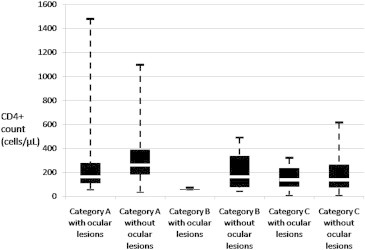
Box and whiskers plot showing CD4+ T-lymphocyte counts of patients in clinical stages (A−C) of human immunodeficiency virus infection, with and without ocular manifestations of human immunodeficiency virus.
In summary, ocular findings in the 87 cases with decreasing order of prevalence were conjunctival microvasculopathy (9.66% of total, 35.63% of 87), anterior uveitis (7.79% of total, V 28.74% of 87), posterior uveitis (5.6% of total, 20.69% of 87), HIV retinopathy (3.74% of total, 13.79% of 87), molluscum contagiosum (1.87% of total, 6.90% of 87), and lastly neuro-oph-thalmic manifestations (0.09% of total, 3.45% of 87). However, a large proportion of cases (36% of 125) had subnormal TBUT and/or Schirmer’s test. The range of CD4+ counts at which these manifestations were seen has been illustrated in Fig. 7.
Fig. 7.
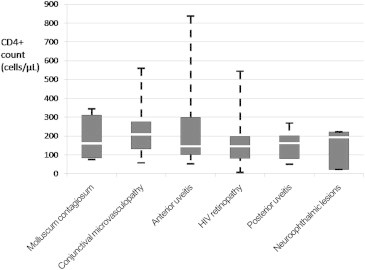
Box and whiskers plot showing CD4+ T-lymphocyte counts of patients with different ocular manifestations of HIV. HIV: human immunodeficiency virus.
Discussion
This study was carried out on subjects among whom 79.75% (256 cases) had the asymptomatic category A, 4.36% (14 cases) had category B, and only 15.89% (51 cases) had category C HIV infection. Contrary to this, a study done by Sujit Gharai et al consisted of 100 consecutive HIV cases, of whom only 17% had category A, 23% had category B, and the majority (60%) had category C HIV infection.7 The ophthalmic manifestations in their study in decreasing order of frequency were CMV retinitis (20%), neuro-ophthalmic manifestations (12%), complicated cataract (6%), IRU in (5%), acute retinal necrosis (3%), choroiditis (2%), keratouveitis (1%), and corneal ulcer (1 %). Only 68% of these patients were on ART as compared to 85.05% cases in our study. It was 45% of cases in their study as compared to 27.10% (87 cases) in our study who had ophthalmic manifestations of HIV.
Another study on South-Indian patients done by Sahu et al examined 19 cases of AIDS (group A) and their 6 relatives (group B) who were asymptomatic HIV-seropositive cases.8 All cases in group A had ocular lesions whereas none of the cases in group B had the same. In our study too, we had 51 cases (15.89% of 321) fulfilling the CDC criteria of stage C of HIV infection and 43.14% (22 cases) of them had ocular manifestations. Only 24.07% (65 cases) of the remaining 270 cases, who were in stages A or B of HIV disease, had ocular lesions.
In another cross-sectional study done at a tertiary care centre in Western India, 112 HIV-positive patients, all with CD4+ count < 200 cells/μL, and all being on ART, were enrolled.10 The prevalence of ocular manifestations in these cases was only nine out of 112 (8%). The ocular manifestations included HIV retinopathy (5%), IRU (3%), immune recovery vitreitis (3%), and CMV retinitis (2%). The presence of CMV retinitis in their study was comparable to that in our study (two out of 132 cases in the same CD4+ category), the difference not being statistically significant (P = 0.86). Also the presence of HIV retinopathy of 5% in their study was comparable to that in our study (nine out of 132 cases in the same CD4+ category), the difference not being statistically significant (P = 0.63). This study group had 100% of the cases with a CD4+ count <200 cells/μL as compared to only 41.12% in our study group. Only 8% (nine out of 112) of the cases in their study had ocular lesions as compared to 40.90% (54 out of 132) of the cases of the same CD4+ category in our study, the difference being statistically significant. This difference was prevalent because we had additional findings of molluscum contagiosum, conjunctival microvasculopathy, anterior uveitis, posterior uveitis, and neuro-ophthalmic lesions in our study.
Ours was a study group larger as compared to most other studies. Secondly the profile of our subjects was very different from those studies since 79.75% of our cases had asymptomatic category A HIV infection and were found to be HIV-positive on voluntary screening. The average CD4+ count of cases in our study is 276.54 cells/μL. We know that CMV retin-istis is known to occur mostly at CD4 counts of <50 cells/μL. We had only 39 cases with CD4+ counts <100 cells/μL in our study. Out of these 39 cases, only five cases had CD4+ count <50 cells/μL. This surely explains the low prevalence of CMV retinitis in our study. Since, the prevalence of CMV retinitis was low, we can explain why we did not have any case of IRU. Moreover, our cases had already been timely started on ART, antitubercular therapy (ATT), prophylactic antifungal medication, and prophylactic cotrimoxazole as per latest CDC guidelines. This could have cured most of the infective causes of uveitis like TB and toxoplasmosis leaving mostly inactive uveitic lesions when screened by the ophthalmologist during the study. All these factors have contributed to a varied profile of ophthalmic manifestations in our study as compared to the other studies.
Dry eye is a manifestation which has not been stated in most of the other studies. We do have a two year prospective, non-comparative study of 232 registered HIV patients done by Dhawan at a tertiary care centre, in which 93 (40.08%) patients were found to be of the category of mild dry eye on the basis of various tests. About 29 (12.5%) patients and 12 (5.17%) patients were of moderate and severe dry eye categories, respectively. So 57.75% cases in that study had dry eye. In our study, we found 36% (45 out of 125) with a subnormal TBUT and/or a positive Schirmer's test. However, the sensitivity and specificity of the Schirmer’s test and TBUT is poor, especially when the reading has been taken only once and the findings are not supported by more specific tests.14 Hence, further studies with more reliable tests and correlation with the drug history will have to done to find the actual prevalence of dry eye in HIV patients.
To summarise, in our study, CD4+ counts correlated with the prevalence of: (a) total ocular findings/lesions; (b) anterior uveitis; (c) posterior uveitis; and (d) HIV retinopathy, and did not correlate with (a) conjunctival microvasculopathy. Because the number of cases with the following lesions was very few, a reliable statistical analysis could not be done for (a) molluscum contagiosum, and (b) neuro-ophthalmological lesions. Most of the ocular lesions were seen in the CD4+ category of < 200 cells/μL. However, 13 cases (14.94% of the 87 cases with ocular findings) in this study had sight-threatening ocular lesions in spite of CD4+ count of >200 cells/μL.
We conclude that anterior uveitis, HIV retinopathy, and posterior uveitis had a significant association with the CD4+ count in our study and can therefore be considered as reliable markers of low CD4+ cell count in centres where the facility of CD4+ analysis does not exist. Secondly, there was a significant association of the overall occurrence of HIV-related ocular lesions with the CD4+ counts, most of the findings occurring at CD4+ counts < 200 cells/μL. Thirdly, there was no significant difference in the occurrence of ocular lesions between the symptomatic cases and the asymptomatic carriers of HIV. Hence, we can infer that even asymptomatic cases of HIV and also the cases with CD4+ cell count >200 cells/μL may be harbouring sight-threatening ocular lesions, and must be routinely screened for the same.
Intellectual Contributions of Authors
Study concept: Maj Vikas Ambiya, Lt Col Amitabh Sagar Drafting and manuscript revision: Maj Vikas Ambiya, Lt Col Amitabh Sagar, Col Sagarika Patyal, Brig AP Mohanty, vsm Statistical analysis: Maj Vikas Ambiya, Lt Col Amitabh Sagar Study supervision: Col Sagarika Patyal, Brig AP Mohanty, vsm.
Conflicts of interest
None identified.
References
- 1.Chiou S.H., Liu C.Y., Hsu W.M. Ophthalmic findings in patients with AIDS. J Microbiol Immunol Infect. 2000;33:45–48. [PubMed] [Google Scholar]
- 2.Turner B.J., Hecht F.M., Ismail R.B. CD4+ T-lymphocyte measures in the treatment of individuals infected with human immunodeficiency virus type 1: a review for clinical practitioners. Arch Intern Med. 1994;154:1561–1573. [PubMed] [Google Scholar]
- 3.Stephenson J. The art of ‘HAART’: researchers probe the potential and limits of aggressive HIV treatments. JAMA. 1997;277:614–616. [PubMed] [Google Scholar]
- 4.Autran B., Carcelain G., Li T.S. Positive effects of combined antiretroviral therapy on CD4+ T cell homeostasis and function in advanced HIV disease. Science. 1997;277:112–116. doi: 10.1126/science.277.5322.112. [DOI] [PubMed] [Google Scholar]
- 5.Connors M., Kovacs J.A., Krevat S., Gea-Banacloche J.C., Sneller M.C., Flanigan M. HIV infection induces changes in CD4 + T-cell phenotype and depletions within CD4+ T-cell repertoire that are not immediately restored by antiviral or immune based therapies. Nat Med. 1997;3:533–540. doi: 10.1038/nm0597-533. [DOI] [PubMed] [Google Scholar]
- 6.Jacobson M.A., Zegans M., Pavan P.R., O’Donnell J.J., Sattler F., Rao N. Cytomegalovirus retinitis after initiation of highly active antiretroviral therapy. Lancet. 1997;349:1443–1445. doi: 10.1016/S0140-6736(96)11431-8. [DOI] [PubMed] [Google Scholar]
- 7.Gharai S., Venkatesh P., Garg S., Sharma S.K., Vohra R. Ophthalmic manifestations of HIV infections in India in the era of HAART: analysis of 100 consecutive patients evaluated at a tertiary eye care center in India. Ophthal Epidemiol. 2008;15:264–271. doi: 10.1080/09286580802077716. [DOI] [PubMed] [Google Scholar]
- 8.Sahu D.K., Namperumalsamy P., Walimbe P., Rajalakshmi C. Ocular manifestations of HIV infection/AIDS in South Indian patients. Indian J Ophthalmol. 1999;47:79–85. [Google Scholar]
- 9.Biswas J., Joseph A., Raizada S., Kumamsamy N., Solomon S. Ophthalmic manifestations of human immunodeficiency virus (HIV) infection in India. Indian J Ophthalmol. 1999;47:87–93. [Google Scholar]
- 10.Shah S.U., Kerkar S.P., Pazare A.R. Evaluation of ocular manifestations and blindness in HIV/AIDS patients on HAART in a tertiary care hospital in western India. Br J Ophthalmol. 2009;93:88–90. doi: 10.1136/bjo.2008.149237. [DOI] [PubMed] [Google Scholar]
- 11.Dhawan P. Tear Film in Patients on HAART Regime—a clinical evaluation intertiary health centre. Lacrimal section. In: Proceedings of the 67th Annual Conference of All India Ophthalmological Society 2009 February 5−8; Jaipur.
- 12.Teich S.A. Conjunctival vascular changes in AIDs and AIDS-related complex. Am J Ophthalmol. 1987;103:332. [PubMed] [Google Scholar]
- 13.Engstrom R.E., Holland G.N., Hardy W.D., Meiselman H.J. Haemorheologic abnormalities in patients with human immunodeficiency virus infection and ophthalmic microvasculopathy. Am J Ophthalmol. 1990;109:153–161. doi: 10.1016/s0002-9394(14)75980-x. [DOI] [PubMed] [Google Scholar]
- 14.Versura P., Frigato M., Cellini M., Mule R., Campos E.C. Diagnostic performance of tear function tests in Sjogren syndrome patients. Eye. 2007;21:229–237. doi: 10.1038/sj.eye.6702204. [DOI] [PubMed] [Google Scholar]


