Abstract
Background
Soft tissue defects in the lower limb pose a formidable challenge due to lack of reliable local flap options. Due to thin non-expendable soft tissues and predisposition to massive edema formation, even small defects become problematic. Perforator flaps represent the latest trends in soft tissue coverage. The aim of this study was to evaluate the effectiveness of perforator flaps as coverage of soft tissue defects in lower limbs.
Material and methods
A series of patients with soft tissue defects of various etiologies in the lower limb were treated using perforator flap at a tertiary care service hospital. Six were free flaps and fourteen pedicled flaps. Doppler ultrasound was used to identify recipient and donor vessels pre-operatively.
Results
Only one flap was lost due to venous congestion. In another case of carcinoma penis there was delayed healing due to persistent lymphorrhoea as a result of post-operative status following lymph node dissection and radiotherapy. Fifteen donor sites required split skin grafting, as they could not be closed directly.
Conclusion
Perforator flaps are a reliable option for closure of soft tissue defects of lower limb irrespective of size, location and depth. There is minimal donor site morbidity. It has the advantage of rapid dissection, flap elevation and reliable skin territory. As no special equipment is required it can be replicated in smaller centers also.
Keywords: Perforator flaps, Lower limb reconstruction, Soft tissue coverage, Wounds and injuries
Introduction
Soft tissue defects in the lower extremity, especially distal third of leg, present a formidable challenge due to lack of reliable local flaps. Conventional reconstructive options include split skin grafting, local random fasciocutaneous flaps, Ponten's super flap, cross leg fasciocutaneous flap, pedicled muscular or musculocutaneous flaps or microvascular free tissue transfer. All these procedures have their limitations and associated morbidity at donor site. Limb salvage rates have greatly improved in last 20–30 years.1 Reconstruction now addresses not only soft tissue coverage but also takes into consideration functional recovery, infection control and cosmetic outcome.
Evolution of perforator flaps started when survival of free flaps had already reached 98%.2 Quest for refinements and reduction in donor site morbidity resulted in the development of the perforator flap. Perforator vessels are those where the source artery is deep and the branch that carries blood to the fasciocutaneous tissues passes through the overlying deep fascia.3 There are three types of perforators-direct cutaneous, septocutaneous and musculocutaneous.4 Musculocutaneous perforators are named according to the muscle perforated. Other perforators are named according to name of proximal artery.5 Perforator flaps have the advantage of less donor site morbidity, replacement with like tissue, alleviation from concern of anatomic variation in different individuals. Post-operative recovery is less painful as no muscle is divided; main source vessel is not divided. Fat can be added for bulk. It has been shown to provide adequate coverage for Gustillo III fracture with respect to consolidation and infection.6
Material and methods
From July 2007 to June 2009, twenty patients with soft tissue defects in lower limbs were managed with perforator flaps. 4 MHz and 8 MHz hand held Doppler was used to mark potential recipient vessels and trace perforators of the flap. Particulars of the patients, dimensions and location of defects with presence of infection was noted. Success of the flap to provide skin cover was assessed by flap survival and healing of the margins of the flap. If following the removal of sutures, there was no gaping of the edges, the flap was considered effective. Wound debridement and bone fixation was done before soft tissue coverage. All perforators in the vicinity of the defect were marked using Doppler. The flap was designed around the major perforator close to the defect. The width of the defect equaled the width of the flap. The length of the proximal limb equaled the longitudinal length of the defect and distance from proximal wound edge to the perforator for propeller type of flaps. For transposition or interpositional movement of the flap, conventional method of flap marking was carried out. Dissection was carried out after inflation of pneumatic tourniquet and under loupe magnification. Once an adequate caliber artery with venae comitantes was identified the flap design was re-evaluated. We considered greater than 1 mm caliber for the artery as adequate if it showed visible pulsations under magnification. If superficial nerves or saphenous vein were encountered they were preserved. If undue tension was encountered after insetting, the perforator was further dissected into muscle or septum to gain additional length. Multiple perforated drains are placed under the flap.
A light dressing with dorsal splint and limb elevation for 5 days was done. No disprin or heparin was given routinely. A two-team approach was used for microvascular free tissue transfer. The first team started exploring the limb for the recipient vessel. This was done under loupe magnification at a location marked by pre-operative hand held Doppler and the knowledge of regional anatomy. The second team simultaneously began elevating the perforator flap and its vascular pedicle. For the free flaps, flap was measured as the exact replica of the likely defect. Microvascular anastomosis was carried out under operating microscope for one artery and one or two accompanying veins measuring 1–3 mm in diameter. After anastomosis, brisk bleeding from the margin was confirmed and flap inset over defect.
Results
There were eighteen males and only two female patients. Age ranged between 14 and 58 years. Majority was between 20 and 40 years. Patients were placed in two groups based on etiology. Fourteen had trauma as primary etiology, four had defects due to carcinoma excision, one each due to soft tissue infection and burn contracture release (Fig. 1). Region wise distribution of soft tissue defects is tabulated in Fig. 2. In six cases free perforator flaps were used. Free anterolateral thigh (ALT) flap was used in all six cases (Fig. 3). These were used to cover amputation stump in three cases (Figs. 4 and 5), one defect over dorsum of foot and one each for defect in popliteal fossa and middle third of leg. Of the 14 pedicled or islanded flaps, three were ALT flaps. One was used to cover contra lateral groin defect in a case of carcinoma penis who had undergone lymph node dissection, radiotherapy and attempted tensor fascia lata repair of the defect. The islanded flap was raised with some bulk of vastus lateralis to obliterate contour deformity. Distally based islanded ALT flap was used to cover defect after post burn contracture release of popliteal fossa. However, it was lost due to venous congestion. Another pedicled perforater plus ALT flap was used to cover a groin defect. Three cases of superior lateral geniculate artery perforator flaps were used for defects around knee and popliteal fossa (Fig. 6). In two cases the secondary defect was closed directly. Posterior tibial artery perforator flap was used in five cases: two cases of defect in mid third leg, two cases in lower third leg and one over the medial malleolus (Fig. 6). Peroneal perforator flap was used for defect on lateral malleolus with exposed hardware (Fig. 7). An islanded anterior tibial artery perforator flap was used for ankle defect (Fig. 7). For a post-traumatic soft tissue defect overlying patellar tendon medial sural artery perforator flap was used.
Fig. 1.
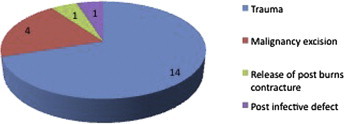
Etiology wise distribution of soft tissue defects.
Fig. 2.
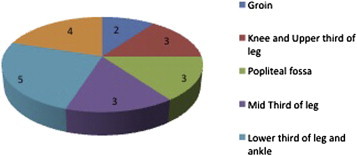
Region wise distribution of soft tissue defects.
Fig. 3.
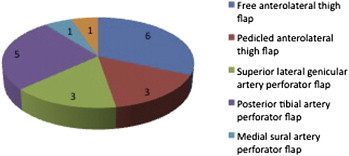
Types of perforator flaps used.
Fig. 4.

Free anterolateral thigh flap for stump closure.
Fig. 5.
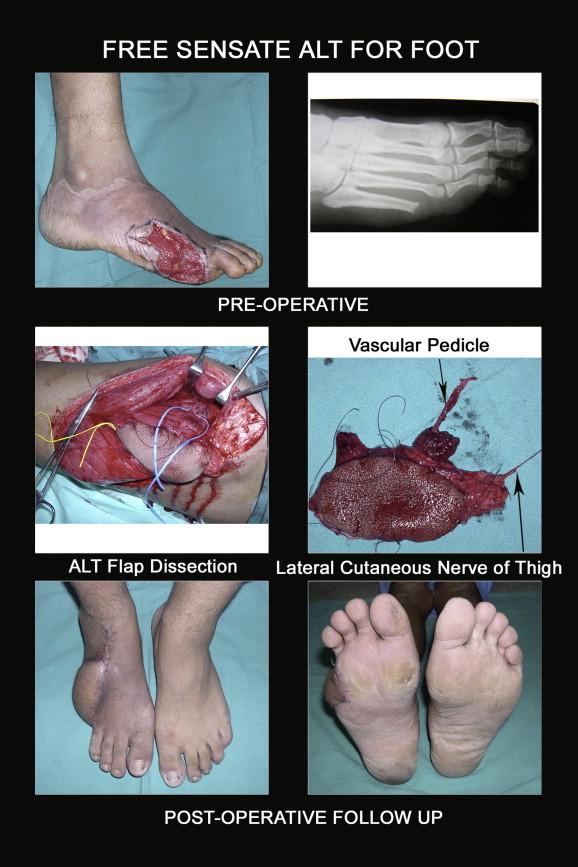
Free sensate anterolateral thigh flap for the foot.
Fig. 6.

More perforator flaps.
Fig. 7.
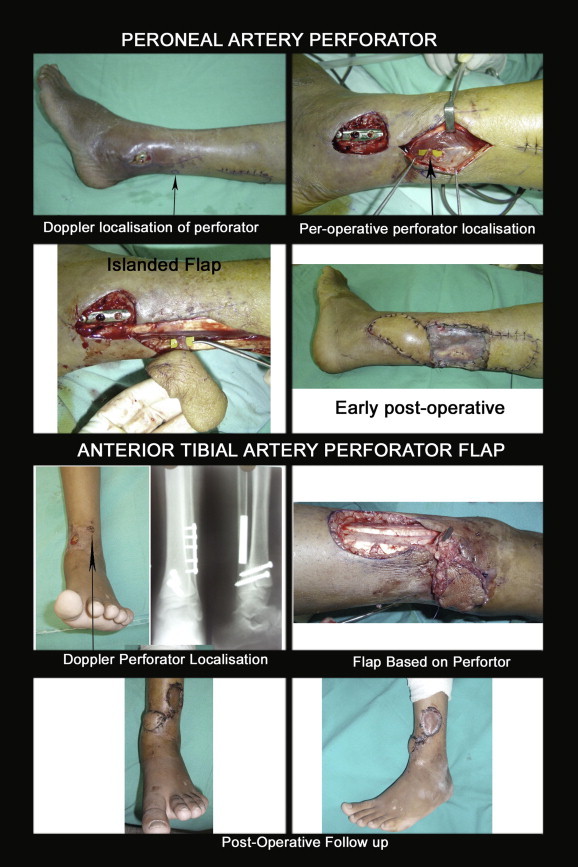
Yet more perforator flaps.
Size of free perforator flaps ranged from 7 × 8 cm (56 cm2) to 25 × 16 cm (400 cm2) with average of 175 sqcm. Size of pedicled flaps ranged from 4 × 3 cm (12 cm2) to 25 × 16 cm (176 cm2). Distribution of flaps according to movement is shown in Fig. 8. Nine pedicled flaps were moved as propeller flaps with rotation between 100° and 180°. In three cases flaps were moved as interposition flaps after complete islanding. One was moved as V–Y advancement and another as transposition flap. Fifteen donor sites required grafting. Even small secondary defects after harvesting of the flaps in ankle and lower third leg required skin grafting, as they could not be closed directly. All flaps healed well except the groin defect following lymph node dissection and radiotherapy, which continued to have lymphorrhoea leading to delay in healing.
Fig. 8.
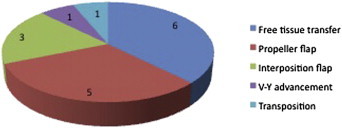
Movement of flaps.
Duration of surgery for free flaps was from 5 to 15 h, with median of 6 h. Fourteen hours in one case was due to only one surgical team and need for revision of microvascular anastomosis.
Total hospital stay after surgery ranged from 10 to 21 days with an average of 16 days. Longer stay seen in few cases was commonly due to partial loss of skin graft at donor site. Persisting lymphorrhoea from under the flap in groin resulted in prolonged hospitalization in one case.
Discussion
Perforator flaps represent the latest descendant in a line of evolution that began with the random pattern flap. Soft tissue defects of distal lower limb are a common problem in defense personnel due to activity and high mobility. This presents a formidable challenge due to lack of reliable local flaps. Due to thin non-expendable soft tissues and predisposition for massive edema even small defects can become problematic.7
For large defects with deep cavities muscle flaps provide superior obliteration of the cavity. For moderate sized defects, a deepithelialized part of skin flap can provide obliteration as well.1 For bony fractures, there is no significant difference as far as consolidation and infection are concerned between the coverage provided by muscular or fasciocutaneous flaps, provided wound debridement was adequate.6
Pedicled perforator flaps for lower limb soft tissue defects are an interesting option as several constant perforators are available.7 The thin consistency allows patient to wear normal shoes. Ease of harvest and inset makes this a quick procedure.
As no special instruments are required for pedicled perforator flaps they can be performed in smaller centers also. Flap can be based on any type of perforator. This free style principle allows different flap designs in presence of a Doppler signal in close proximity to the defect.7
One of the disadvantages of local perforator flaps is that they are raised within the zone of injury, which may leave part of the flap with a potentially impaired perfusion. It is important to limit the length of the flap to two vascular territories, if more than two are verified by Doppler study then the flap may be inadequate without a prior delay procedure.
For the distal third of tibia, local islanded fasciocutaneous perforator flap allow adequate coverage, but the donor area often requires skin grafting. When a local perforator flap is designed as a propeller flap an excellent esthetic result and direct closure of donor site can be achieved. In this study nine patients underwent propeller movement with good results. In another study eight patients underwent similar repair with good results and patients returned to full ambulation in 8 weeks.7
Peroneal perforator based propeller flap in ankle region are a good option, provide good form and function with excellent surface area and mobility for dynamic areas without sacrificing any major vessel or nerve. We used one such flap to cover a defect over lateral malleolus. There is another single case report of fasciocutaneous propeller flap based on peroneal artery perforator, rotated 180° for digital papillary carcinoma of posterolateral ankle and Achilles tendon, providing a gliding surface for Achilles tendon.8
In our study we did not lose any anterolateral thigh free flap, whereas in another larger study of seventy cases, there was total flap failure in three patients and partial failure in five patients. The free anterolateral thigh flap has become the workhorse in many centers. It is a reliable flap with consistent anatomy and a long constant pedicle diameter. Its versatility in which thickness and volume can be adjusted, leads to a perfect match of customized reconstruction.9
We used an islanded anterolateral thigh flap with some bulk of vastus lateralis to cover a deep defect in the groin following lymph node dissection and radiotherapy. It has been shown that with anterolateral thigh flap varying sizes of vastus lateralis can be harvested. The skin islands of these flaps have great range when dissected on their perforator. Indication for adding a muscular component is exposed bone, skull base or osteosynthesis, open sinuses and lack of muscle bulk.10
Conclusion
Perforator flaps have emerged as a reliable option for the soft tissue defects of lower limb irrespective of its size, location and depth. The biggest advantage of perforator flap is limited donor site morbidity. These flaps also offer the advantage of relatively rapid dissection and flap elevation, and reliable skin territory. As with any other new surgical technique, there is a learning curve associated with perforator flaps. As no special equipment is required it can be replicated in smaller centers also.
Intellectual contribution of authors
Study concept: Maj Gen M K Mukherjee, ysm.
Drafting and manuscript revision: Col M A Parwaz.
Statistical analysis: Col Vijay Langer.
Study supervision: Col Vijay Langer, Brig B Chakravarty.
Conflicts of interest
All authors have none to declare.
References
- 1.Hong J.P. The use of supermicrosurgery in lower extremity reconstruction: the next step in evolution. Plast Reconstr Surg. 2009;123:230–235. doi: 10.1097/PRS.0b013e3181904dc4. [DOI] [PubMed] [Google Scholar]
- 2.Wei F.C., Celik N. Perforator flap entity. Clin Plastic Surg. 2003;30:325–329. doi: 10.1016/s0094-1298(03)00033-6. [DOI] [PubMed] [Google Scholar]
- 3.Geddes C.R., Morris S.F., Neligan P.C. Perforator flaps: evolution, classification and applications. Ann Plast Surg. 2003;50:90–99. doi: 10.1097/00000637-200301000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Blondeel P.N., Van Landuyt K., Hamdi M., Monstrey S.J. Perforator flap terminology: update 2002. Clin Plast Surg. 2003;30:343–346. doi: 10.1016/s0094-1298(03)00035-x. [DOI] [PubMed] [Google Scholar]
- 5.Kim J.T. New nomenclature concept of flap. Br J Plast Surg. 2005;58:431–440. doi: 10.1016/j.bjps.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 6.Danino A.M., Gras M., Coeugniet E., Jebrane A., Harris P.G. Is muscle the best coverage for leg Gustillo IIIb fractures? A retrospective comparative study. Ann Chir Plast Esthet. 2008;53:473–479. doi: 10.1016/j.anplas.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 7.Jakubietz R.G., Jakubietz M.G., Gruenert J.G., Jakubietz M.G. The 180-degree perforator-based propeller flap for soft tissue coverage of the distal, lower extremity: a new method to achieve reliable coverage of the distal lower extremity with a local, fasciocutaneous perforator flap. Ann Plast Surg. 2007;59:667–671. doi: 10.1097/SAP.0b013e31803c9b66. [DOI] [PubMed] [Google Scholar]
- 8.Rad A.N., Singh N.K., Rosson G.D. Peroneal artery perforator based propeller flap of the lateral distal lower extremity after tumour extirpation: case report and literature review. Microsurgery. 2008;28:663–670. doi: 10.1002/micr.20557. [DOI] [PubMed] [Google Scholar]
- 9.Engel H., Gazyakan E., Cheng M.H., Piel D., Germann G., Giessler G. Customized reconstruction with the free anterolateral thigh perforator flap. Microsurgery. 2008;28:489–494. doi: 10.1002/micr.20538. [DOI] [PubMed] [Google Scholar]
- 10.Posch N.A., Mureau M.A., Flood S.J., Hofer S.O. The combined free partial vastus lateralis with anterolateral thigh flap reconstruction of extensive composite defects. Br J Plast Surg. 2005;58:1095–1103. doi: 10.1016/j.bjps.2005.04.022. [DOI] [PubMed] [Google Scholar]


