Abstract
Background
The mortality and morbidity rates are two to fourfold higher among Coronary Artery Disease (CAD) patients with type 2 diabetes mellitus (DM). American Diabetes Association (ADA) and World Health Organization (WHO) define different criteria for the diagnosis of glucose intolerance. This study compares the available diagnostic criteria for DM in Indian men and their importance in CAD patients.
Methods
This cross-sectional study was done on 794 male volunteers; 483 individuals from general population and 311 patients undergoing angiography for evaluation of CAD. Individuals with previous clinical history of diabetes mellitus were excluded.
Results
More than 90% of diabetics by ADA criteria could be diagnosed by Fasting plasma glucose (FPG) and HbA1c criteria while FPG and pg2h plasma glucose (WHO criteria) could detect only 74%. Impaired Fasting Glucose (IFG) or Impaired Glucose Tolerance (IGT) was present in 36.7% of individuals diagnosed to be diabetic based on HbA1c; more in CAD +ve group (53.8%) than in general population (23.6%). ROC analysis suggests >121 mg/dl of FPG or >6.2% of HbA1c as optimum cut-off for the diagnosis of DM. FPG and HbA1c criteria have higher Relative Risk for presence of coronary artery occlusion and HOMA-IR.
Conclusion
Inclusion of HbA1c in the criteria for diagnosis of DM (ADA criteria) can detect large number of cases with persistent hyperglycemia in the non-diagnostic range of DM (IFG or IGT) among general population and CAD patients. This has special relevance to epidemiological studies as the diagnosis of DM can be made on single fasting blood sample.
Keywords: Coronary artery disease (CAD), American Diabetes Association (ADA) criteria, World Health Organization (WHO) criteria, HbA1c, Diabetes mellitus (DM)
Introduction
A degree of hyperglycemia sufficient to cause pathologic and functional changes in various target tissues, but without clinical symptoms, may be present for a long period of time before Diabetes Mellitus (DM) is detected. During this asymptomatic period, it is possible to demonstrate an abnormality in carbohydrate metabolism by measurement of HbA1c, plasma glucose in the fasting state or after a challenge with an oral glucose load. The degree of hyperglycemia (if any) may change over time, depending on the extent of the underlying disease process. The disease process, in its initial stages, may cause Impaired Fasting Glucose (IFG) and/or Impaired Glucose Tolerance (IGT) without fulfilling the criteria for the diagnosis of DM. The degree of hyperglycemia reflects the severity of the underlying metabolic derangement and the propensity to develop complications. There have been reports of unsuspected glucose abnormalities in patients with coronary artery disease.1 It was observed by McGinn et al that there is substantial amount of undiagnosed dysglycemia. They observed that 10.4% of patients undergoing CABG and not to have DM were found to have HbA1c of ≥ 6.5%.2 Similarly, it has been reported that FPG alone did not identify half the patients with dysglycemia and the FPG and HbA1c measurement in combination were a useful strategy to identify coronary patients with unknown DM.3 In addition it has been reported that morbidity and mortality is higher among CAD patients with type 2 DM or IGT.4
World Health Organization (WHO) published the guidelines for the Definition, Diagnosis and Classification of Diabetes Mellitus and intermediate hyperglycemia in 2006.5 In 2009 the American Diabetes Association (ADA), International Diabetes Federation (IDF) and European Association for the Study of Diabetes (EASD) reviewed its diagnostic criteria. While the criteria for the diagnosis of diabetes and Impaired Glucose Tolerance (IGT) remained unchanged, the ADA recommended lowering the threshold for Impaired Fasting Glucose (IFG) from 6.1 mmol/l (110 mg/dL) to 5.6 mmol/l (100 mg/dL) and inclusion of HbA1c ≥ 6.5% as an additional diagnostic criteria for DM.6 In addition to IFG and IGT the ADA has included the HbA1c of 5.7–6.4% as an additional category for increased risk of diabetes (prediabetes).7 Ramachandran et al have shown high prevalence of hyperglycemia following Acute Coronary Syndrome (ACS) among Indians.8
The present study evaluates the role of HbA1c to detect the abnormalities of glucose metabolism in general population and patients undergoing investigation for CAD.
Material and methods
The study design chosen was a cross-sectional study. A total of seven hundred and ninety four male individuals volunteered for the study. It consisted of 483 individuals from general population and 311 patients who have been found to have clinical and ECG evidence of coronary artery disease and were undergoing angiography for CAD investigation. The patients had been admitted to the tertiary cardiac care hospital on referral for investigation of coronary artery disease or on presenting to the emergency room with anginal chest pain, dyspnea, diaphoresis and palpitation associated with significant ECG ST-T wave and Q wave changes.
Previous clinical history of diabetes mellitus and hypertension was taken along with the history of medication including antihypertensives, oral hypoglycemic agents, insulin injection and lipid lowering agents. Those undergoing angiography had 57 patients of DM on different therapy while general population group had 30 of such individuals. The general population group was from various army units (n = 260) locally and volunteers from local civilian population. Therefore, a total of 707 individuals from both the groups out of 794 had no previously confirmed DM. Out of 707 non-diabetics, four participants were found to have hemoglobinopathy and were not included in HbA1c related analysis.
Fasting blood was collected for blood glucose in sodium fluoride tube and for serum insulin in plain vacutainers. Patients were given 75 gm anhydrous glucose dissolved in 300 ml of water and post glucose load sample for blood glucose and insulin were taken after 2 h. Glycated hemoglobin (HbA1c) levels were determined by high performance liquid chromatography on fasting blood samples, collected in EDTA tubes. The HbA1c values were calibrated in accordance with DCCT. The kit was procured from Diamat, Germany.
DM, IFG and normal fasting glucose (NFG) were defined according to the new ADA criteria6 and IGT according to WHO criteria5 based on plasma glucose in individuals having HbA1c < 6.5%. The category of abnormal glucose was defined as IFG, IGT, or DM based on either ADA or WHO criteria.
Angiography was carried out in all of the patients suspected of CAD as investigative procedure; the findings were recorded along with the number of vessels involved. Patients were considered CAD +ve if one or more coronaries showed an occlusion of more than 50% else they were labeled CAD −ve.
Insulin assay was conducted by a solid phase two-site enzyme immunoassay kit obtained from Diasys, Germany. The Insulin resistance was determined by HOMA-IR using formula:
Fasting insulin (mIU/mL) × fasting glucose (mg/dL)/405
The statistical analysis for ROC was carried out using Medcalc, Belgium, free trial software. Other analyses were carried out using Epi Info, Database and statistics software for public health professionals, from Centers for Disease Control and Prevention (CDC), USA.
Results
The mean (SD) parameters for age, BMI, Fasting & 2 h post-glucose load plasma glucose (pg2h), and HbA1c in the study population are given in Table 1. The age, BMI, pg2h, are significantly different in CAD +ve group than in general population.
Table 1.
Mean and SD of various parameters in general population and CAD groups.
| Parameter | General population (n = 450) |
CAD +ve (n = 195) |
CAD −ve (n = 58) |
|||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Age (Yrs) | 44.37 | 6.61 | 58.62a | 7.64 | 48.66 | 13.98 |
| Height (m) | 1.70 | 0.06 | 1.66 | 0.05 | 1.67 | 0.07 |
| Weight (kg) | 69.06 | 9.21 | 69.50 | 9.20 | 66.79 | 7.93 |
| BMI (kg/m2) | 23.79 | 2.92 | 25.33a | 3.57 | 23.86 | 2.61 |
| Glucose (Fasting) (mg/dL) | 104.2 | 28.5 | 101.3 | 28.9 | 95.3 | 25.9 |
| Glucose (Pg2h) (mg/dL) | 117.0 | 54.7 | 125.4a | 40.0 | 115.8 | 45.7 |
| HbA1c (%)a | 5.44 | 1.00 | 5.44 | 1.20 | 5.22 | 1.08 |
| Insulin Fasting (IU/L) | 9.84 | 6.20 | 11.99 | 11.24 | 13.44 | 13.07 |
| Insulin pg2h (IU/L) | 30.13 | 25.02 | 35.43 | 36.31 | 21.83 | 19.50 |
| HOMA-IR | 2.56 | 1.90 | 3.18 | 3.89 | 3.27 | 3.71 |
Statistically significantly different compared to general population.
The distribution of individuals with HbA1c of <6.5% and ≥6.5% in general population and CAD group in NGT, IFG, IGT and DM are given in Table 2.
Table 2.
Distribution of study population into different categories of glucose tolerance and HbA1c.
| Glucose tolerance | General population |
CAD +ve |
CAD −ve |
|||
|---|---|---|---|---|---|---|
| <6.5% | ≥6.5% | <6.5% | ≥6.5% | <6.5% | ≥6.5% | |
| NFG | 225 | 4 | 111 | 1 | 40 | 0 |
| IFG | 134 | 3 | 32 | 4 | 8 | 0 |
| IGT | 29 | 5 | 19 | 10 | 4 | 0 |
| DM | 28 | 22 | 7 | 11 | 3 | 3 |
| Total | 416 | 34 | 169 | 26 | 55 | 3 |
IFG/IGT with HbA1c ≥ 6.5% is present in 53.8% and 23.6% of CAD +ve group and general population, respectively. IFG or IGT was present in significantly large percentage (34.9%) of individuals diagnosed to be diabetic based on HbA1c ≥ 6.5%. The patients in CAD +ve group with IGT had higher percentage (34.4%) of HbA1c ≥ 6.5% than general population (14.7%). None of the individuals in CAD −ve group with IFG or IGT had HbA1c ≥ 6.5%. Amongst patients diagnosed to be with DM by WHO criteria, HbA1c ≥ 6.5% was present in 61.1% of CAD +ve individuals compared to 44.0% in general population. The percentage of individuals in IFG group with HbA1c of ≥6.5% is also higher in CAD +ve group (12.5%) than in general population (2.2%). The overall incidence of individuals with HbA1c ≥ 6.5% with abnormal glucose tolerance is higher in CAD +ve group than in general population being 30.1% and 13.5%, respectively.
ROC analysis to find optimum cut-off values
Since the two groups are heterogeneous to the extent that all the individuals in the CAD group have undergone laboratory evaluation at certain stage of there illness, while individuals from general population have undergone laboratory evaluation only if they had clinical presentation, the ROC analyses were carried out with only general population group to find optimum cut-off for the diagnosis of DM. The results are depicted in Figs. 1 and 2. The cut-off values on ROC are found to be >121 mg/dL and >6.2%, for Fasting plasma glucose and HbA1c, respectively.
Fig. 1.
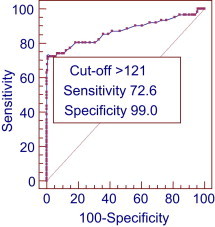
ROC curve for Fasting plasma glucose diabetes classified by ADA criteria (general population).
Fig. 2.
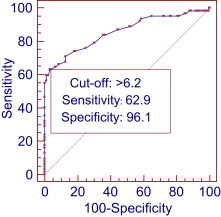
ROC curve for HbA1c diabetes classified by ADA criteria (general population).
We observed that the Fasting plasma glucose criterion is more sensitive and specific than HbA1c. We further analyzed that if we take newly determined criteria (DM_New) from ROC, i.e. fasting > 121 mg/dL or HbA1c > 6.2%, then the number of new cases that are identified and missed with respect to ADA criteria for the diagnosis of DM are given in Table 3.
Table 3.
Distribution of patients with DM diagnosed by ADA and new criteria (DM_New).
| DM by ADA criteria (DM_ADA) | DM by ROC criteria (DM_New) (Fasting plasma glucose >121 mg/dL or HbA1c >6.2%) |
Total | |
|---|---|---|---|
| +ve | –ve | ||
| +ve | 96 | 5 | 101 |
| –ve | 18 | 584 | 602 |
| Total | 114 | 589 | 703 |
If we compare the ADA criteria with conventional criteria of WHO than we find that 27 cases of DM i.e. 26.7% of cases are missed which are identified as having HbA1c of ≥6.5% (Table 4), while Fasting plasma glucose of ≥126 mg/dL alone as criteria, misses 17.5 and 39.6% of cases identified by the WHO and ADA criteria, respectively.
Table 4.
Incidence of patients diagnosed with diabetes according to different criteria among general population (n = 450), CAD (n = 253) and total population (n = 703).
| Criteria | General population n (%) | CAD n (%) | Total population n (%) |
|---|---|---|---|
| Fasting ≥ 126 mg/dL, or pg2h ≥ 200 mg/dL or HbA1c ≥ 6.5% (DM_ADA) | 62 (13.7) | 39 (15.4) | 101 (14.4) |
| Fasting ≥ 126 mg/dL or pg2h ≥ 200 mg/dL (DM_WHO) | 50 (11.1) | 24 (9.5) | 74 (10.5) |
| Fasting ≥ 126 mg/dL or HbA1c ≥ 6.5 (DM_fHb) | 56 (12.4) | 37 (14.6) | 93 (13.2) |
| Fasting ≥ 126 mg/dL | 39 (8.7) | 22 (8.7) | 61 (8.7) |
| HbA1c ≥ 6.5% | 34 (7.6) | 29 (11.5) | 63 (8.9) |
| pg2h ≥ 200 mg/dL | 27 (6.0) | 11 (4.4) | 38 (5.4) |
| pg2h ≥ 200 mg/dL or HbA1c ≥ 6.5% | 43 (9.6) | 32 (12.7) | 75 (10.5) |
Criteria for diagnosis of DM and presence of CAD
The Table 5 describes the presence of coronary artery occlusion among patients undergoing angiography for investigation of CAD and the DM diagnosed by different criteria. Relative Risk (RR) is maximum when Fasting and HbA1c is the criteria for the diagnosis of DM at ADA recommended cut-off and marginally higher at cut-off values based on this study.
Table 5.
Relative risk (RR) for presence of occlusion of coronary arteries with different criteria for diagnosis of DM in CAD group (n = 253).
| Criteria | DM |
RR | 95% CI RR | |
|---|---|---|---|---|
| +ve on angiography (n = 195) n (%) | –ve for angiography (n = 58) n (%) | |||
| Fasting ≥ 126 mg/dL or pg2h ≥ 200 mg/dL (DM_WHO) | 18 (9.2) | 6 (10.3) | 0.97 | 0.75–1.24 |
| Fasting ≥ 126 mg/dL or pg2h ≥ 200 mg/dL or HbA1c ≥ 6.5% (DM_ADA) | 33 (16.9) | 6 (10.3) | 1.12 | 0.96–1.30 |
| Fasting ≥ 126 mg/dL or HbA1c ≥ 6.5% (DM_fHb) | 32 (16.4) | 5 (8.6) | 1.15 | 0.99–1.33 |
| Fasting > 121 mg/dL or HbA1c > 6.2% (DM_New) | 37 (19.0) | 5 (8.6) | 1.18 | 1.03–1.35 |
Insulin resistance in DM
The marker used to assess the Insulin resistance is HOMA. A value higher than 75-percentile value of non-diabetics by ADA criteria is taken as an index of Insulin resistance. Occurrence of Insulin resistance's (RR) is given in Table 6. The highest RR is for DM diagnosed on the basis of Fasting plasma glucose and/or HbA1c criteria.
Table 6.
Relative Risk (RR) and 95% CI for presence of Insulin resistance (HOMA above 75th percentile (2.83) of non-diabetics) with DM diagnosed by different criteria.
| DM_ADA | ≥75th percentile | <75th percentile | Total | DM_WHO | ≥75th percentile | <75th percentile | Total |
|---|---|---|---|---|---|---|---|
| Diabetic | 62 | 39 | 101 | Diabetic | 47 | 27 | 74 |
| Non-Diabetic | 149 | 453 | 602 | Non-Diabetic | 164 | 465 | 629 |
| RR HOMA (95% CI) |
2.48 (2.01–3.05) |
2.44 (1.96–3.03) |
|||||
| DM_fHb |
≥75th Percentile |
<75th Percentile |
Total |
DM_New |
≥75th Percentile |
<75th Percentile |
Total |
| Diabetic | 59 | 34 | 93 | Diabetic | 66 | 48 | 114 |
| Non-Diabetic | 152 | 458 | 610 | Non-Diabetic | 145 | 444 | 589 |
| RR HOMA (95% CI) | 2.55 (2.07–3.13) | 2.35 (1.99–2.90) | |||||
Discussion
Out of 703 individuals (450 from general population and 253 patients undergoing angiography for CAD investigation); 101 had one or more abnormalities of glucose metabolism i.e. fasting ≥ 126 mg/dL or post-glucose load 2 h plasma glucose (pg2h) ≥ 200 mg/dL or HbA1c ≥ 6.5%. Total of these abnormalities observed were 162, among 101 individuals i.e. there was an overlap of about 62% among three diagnostic parameters. Fasting criteria of ≥126 mg/dL of plasma glucose as recommended by ADA,9 if employed alone, misses significant number of DM by WHO criteria as reported by Harris et al10 and Somani et al,11 who observed that significant number of persons who were identified to be normoglycemic by fasting glucose criteria alone were having DM, especially in CAD cases. It was therefore suggested to analyze both i.e. fasting and pg2h samples to identify IGT and DM cases. In the present study also, Fasting plasma glucose used alone, misses 17.5 and 39.6% of cases of DM diagnosed by the WHO5 and ADA-2010 criteria,6 respectively.
Out of 101 individuals found to have DM according to ADA by any of the three criteria, 74 could be detected by Fasting and pg2h plasma glucose criteria (only 8 with pg2h values ≥ 200 mg/dL). Alternatively speaking out of 63 individuals who had HbA1c of ≥6.5%; 27 of these had non-diabetic range plasma glucose levels. A similar finding has been reported by McGill et al. They reported that 10.4% of individuals not known to have DM had HbA1c of ≥ 6.5% among patients undergoing CABG, a diagnostic criteria as per ADA.2 Tekumitt et al have reported that FPG and HbA1c combination had a PPV of 97% with sensitivity and specificity of 84.4% and 94.1%, respectively.3 These 27 patients; 17 of IGT, 5 of IFG and 5 normal must have had prolonged period of intermediate hyperglycemia at these non-diagnostic plasma level of glucose, which is reflected as an increase in HbA1c. These 27 could be diagnosed as DM, only on the basis of HbA1c in fasting blood sample. Therefore, it is suggested that if only fasting sample has to be analyzed for the diagnosis of DM then one should consider analyzing the sample for Fasting plasma glucose and HbA1c both. This detects all the cases of DM by ADA criteria except 8 (8%) with isolated 2 h post-glucose load venous plasma glucose of ≥200 mg/dL.
Based on the mean and SD of HbA1c in normoglycemic individuals a value above mean (5.16%) + 2SD (0.64) can be considered as abnormal among Indians, i.e. HbA1c of 6.44%, this is close to the value recommended by ADA as one of the diagnostic criteria of DM i.e. HbA1c ≥ 6.5%. When ROC analysis is carried out with ADA criteria as classification variable to determine cut-off value for Fasting plasma glucose and HbA1c, these are found to be > 121 mg/dL and >6.2%, respectively. We also observed that the individuals diagnosed with newer cut-off criteria based on Fasting plasma glucose/HbA1c have higher odds ratio for presence of Insulin resistance in comparison to various other diagnostic criteria (Table 6).
Out of total 794 cases; 30 out of 483 in general population group (6.2%) and 57 out of 311 in CAD group (18.32%), were having pre-existing DM by WHO criteria and were on therapy for the same. Newly diagnosed cases of DM are 50 (11%) and 24 (9.4%), in the general population and CAD group, respectively. The smaller percentage in CAD group is probably because of prior exclusion of known diabetics in this well investigated hospitalized group. If we pool together these excluded patients on treatment and newly diagnosed patients than overall incidence of DM is higher in CAD group being, 16.6% and 26.0% in general population and CAD group, respectively.
When we analyze the findings of angiography in CAD group (Table 5) it is observed that RR for occlusion of coronaries are much higher when DM is diagnosed by criteria that include HbA1c viz. ADA criteria (RR 1.12); Fasting plasma glucose or HbA1c values as per ADA cut-off (RR 1.15) or ROC based cut-off of Fasting plasma glucose > 121 mg/dL or HbA1c of >6.2% (RR 1.18), compared to WHO criteria without HbA1c (RR 0.97). This increased risk of CAD forms a strong basis for inclusion of HbA1c as criterion for the diagnosis of DM especially in CAD group to pre-empt the coronary occlusion over time. However, this low RR with WHO criteria can also be explained by selective exclusion of diabetics diagnosed with WHO criteria during evaluation of CAD.
The Relative Risk (RR) for presence above 75th percentile of HOMA-IR, a surrogate marker of Insulin resistance, is highest (RR = 2.55) in case of diabetes by Fasting plasma glucose or HbA1c criteria (Table 6). Therefore, for the therapeutic purpose the DM_fHb could be better criteria for the diagnosis of DM. RR for occlusion of coronary arteries was highest when diabetes was diagnosed by DM_New (Fasting plasma glucose > 121 mg/dL or HbA1c > 6.2%). This may be useful for epidemiological/point-of-contact screening, as it requires only single fasting sample with only marginal loss of sensitivity (0.7%) and specificity (2.6%). It is also pertinent that all cases of Fasting plasma glucose of ≥100 mg/dL (IFG by ADA criteria) should be investigated with additional HbA1c estimation.
To conclude, HbA1c should form an important criterion in the diagnosis of DM as suggested by ADA. Moreover, if the test has to be performed on a single sample than based on various parameters, like total cases diagnosed with reference to ADA and WHO diagnostic criteria, as well as relationship to the surrogate markers of Insulin resistance like HOMA-IR and incidence of increased occlusion of coronary arteries, the study of Fasting plasma glucose along with HbA1c, will be the best strategy for diagnosing DM.
Conflicts of Interest
This study has been funded by research grant from O/o DGAFMS.
References
- 1.Soma P., Rheeder P. Unsuspected glucose abnormalities in patients with coronary artery disease. S Afr Med J. 2006;96:216–220. [PubMed] [Google Scholar]
- 2.McGinn J.T., Shariff M.A., Bhat T.M. Prevalence of dysglycemia among coronary artery bypass surgery patients with no previous diabetic history. J Cardiothorac Surg. 2011;6:104–109. doi: 10.1186/1749-8090-6-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tekumit H., Cenal A.R., Polat A., Uzun K., Tataroglu C., Akinci E. Diagnostic value of hemoglobin A1c and fasting plasma glucose levels in coronary artery bypass grafting patients with undiagnosed diabetes mellitus. Ann Thorac Surg. 2010;89(5):1482–1487. doi: 10.1016/j.athoracsur.2009.11.033. [DOI] [PubMed] [Google Scholar]
- 4.Seibaek M., Sloth C., Vallebo L. Glucose tolerance status and severity of coronary artery disease in men referred to coronary arteriography. Am Heart J. 1997;133:622–629. doi: 10.1016/s0002-8703(97)70163-7. [DOI] [PubMed] [Google Scholar]
- 5.Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia. Report of a WHO/IDF Consultation. 2006.
- 6.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(suppl 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Diabetes Association Position statement standards of medical care in diabetes-2011. Diabetes Care. 2011;34(suppl 1):S11–S61. doi: 10.2337/dc11-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramachandran A., Chamukuttan S., Immaneni S. High incidence of glucose intolerance in Asian-Indian subjects with acute coronary artery syndrome. Diabetes Care. 2005;28:2492–2496. doi: 10.2337/diacare.28.10.2492. [DOI] [PubMed] [Google Scholar]
- 9.The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus Report of the expert committee on the diagnosis and classification of Diabetes mellitus. Diabetes Care. 1997;20:1183–1197. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- 10.Harris M.I., Eastman R.C., Cowie C.C., Flegal K.M., Eberhardt M.S. Comparison of diabetic diagnostic categories in the US population according to the 1997 ADA and 1980–85 WHO diagnostic criteria. Diabetes Care. 1997;20:1859–1862. doi: 10.2337/diacare.20.12.1859. [DOI] [PubMed] [Google Scholar]
- 11.Somani B.L., Bangar S.S., Bhalwar R. American Diabetes Association criteria for diabetes diagnosis: another perspective. Diabetes Care. 1999;22:366. doi: 10.2337/diacare.22.2.366b. [DOI] [PubMed] [Google Scholar]


