Abstract
Background
Use of conjunctival autograft following excision of primary pterygium has reduced the recurrence rate. This study evaluates the efficiency of fibrin glue as compared to sutures in attaching the conjunctival autograft with reference to surgical time, post operative comfort and recurrence during follow up.
Methods
60 patients with primary pterygium were included and divided into two groups. In the first group autograft was secured in place with help of 10-0 polyamide monofilament suture while in second group fibrin glue was used. Both the groups were compared in terms of operative time, post op comfort and recurrence.
Results
The average surgical time taken was 50.93 ± 4.96 min with suture group and 34.43 ± 4.94 min with fibrin glue group. Pain and foreign body sensation was markedly less with fibrin glue group. At the end of final follow up at 6 months, 3 cases (10%) from suture group and 1 case (3.33%) from fibrin group had recurrence.
Conclusion
Fibrin glue is effective and safe for attaching conjunctival autograft during pterygium surgery. Although more number of recurrences were observed in suture group as compared to fibrin glue group the difference was not statistically significant (p 0.612).
Keywords: Pterygium, Conjunctival autograft, Fibrin glue
Introduction
Pterygium, a word derived from ‘pterygion’ (ancient Greek for wing) is a wing shaped, fibrovascular overgrowth arising from sub conjunctival tissue extending across the limbus onto cornea. It is a degenerative condition of the sub conjunctival tissue which proliferates as vascularized granulation tissue to invade cornea, destroying superficial layers of stroma and Bowman's membrane, the whole being covered by conjunctival epithelium.1,9
The prevalence rate of primary pterygium varies from 0.7 to 31% in various populations around the world.2 Working outdoors increases the risk 1.5 fold, whereas having darker skin complexion and using eyewear for either reading or distance substantially decreases the risk of developing pterygium.3 Though exact aetiology is not known, risk factors include genetic predisposition, chronic environmental irritations like dust, dryness, heat and ultraviolet rays.3,4
A pterygium is best left alone unless it is progressing towards pupillary area causing excessive astigmatism, restriction of ocular motility or is disfiguring.1 Various techniques have been tried in past from simple excision to use of adjunct therapies such as β radiation, thiotepa, 5-FU, and mitomycin C. The reports of recurrence rates have varied from 25 to 45% after simple excision of primary pterygium.6 The recurrence of pterygium is closely associated with corneal-limbal stem cell deficiency. Spaeth et al introduced the surgical technique of using conjunctival autograft for covering bare sclera after pterygium excision.7 Conjunctival autograft with limbal stem cell transplantation has showed promising results with low recurrence rate. A meta-analysis of various surgical techniques for pterygium excision showed that the odds for pterygium recurrence increase to six and 25 times if conjunctival autograft is not placed.6
Traditionally, during pterygium surgery the conjunctival autografts are secured in place with either absorbable or non-absorbable sutures. Presence of sutures causes discomfort to the patient and is associated with increased inflammation. Tissue adhesives have been used for closing and apposing wound edges quickly. Synthetic tissue adhesives, such as cyanoacrylate, induce sufficient fibrin cross-linking kinetics but are limited by direct tissue toxicity and barrier effect.7 Therefore, natural substances, such as fibrin, have significant advantage in terms of minimal tissue reaction. The use of fibrin glue during pterygium surgery was first described by Cohen et al in 1993.8 Since then various reports have been published regarding the safety and efficacy of fibrin glue in ophthalmic surgery.
This study has been undertaken to evaluate the efficiency of fibrin glue as compared to sutures in attaching the conjunctival autograft with special reference to surgical time, post operative comfort and recurrence during follow up.
Material and methods
60 patients reporting with primary pterygium reporting to military hospital were recruited in the study after obtaining informed consent. A comprehensive evaluation of patients was undertaken including patient's age, gender, medical and ocular history, visual acuity assessment, slit lamp examination and anterior segment photography. Patients with recurrent pterygium, associated symblepharon or history suggestive of any hypersensitivity to human blood products were excluded from the study.
Patients were divided into two groups. In both group of patients, pterygium excision with conjunctival auto grafting was done. The first group of 30 patients (n = 30) autograft was secured in place with help of 10-0 polyamide monofilament suture while in second group of 30 patients (n = 30) fibrin glue was used to secure the autograft in place.
Surgical procedure
After instillation of topical proparacaine HCL (Carecain 0.5%, Ajanta pharma, India), the involved eye underwent standard ophthalmic sterile preparation and draping. Then eye was exposed for surgery using lid speculum. The surgery was performed using operating microscope. Lidocaine–epinephrine solution (Xylocaine 2% AstraZeneca, India) was injected sub conjunctivally under pterygium to make dissection easier as well as acted as haemostatic to prevent excessive bleeding. A sharp blade was used to excise the pterygium head from the cornea. Blunt and sharp dissection was performed to separate the pterygium from underlying sclera and surrounding conjunctiva. The body of the pterygium along with underlying tenons was excised using Westcott scissors. The wound bed was scraped to clean cornea and sclera and only bleeding vessels were cauterized using wet field cautery.
The area of conjunctival defect was measured with a calliper and a free conjunctival limbal autograft measuring the same size as the defect was obtained from the superotemporal quadrant of the bulbar conjunctiva. Care was also taken to prevent buttonholes. The dissected graft was flipped over the cornea and brought near the area of bare sclera formed by excision of the pterygium. Proper orientation was maintained, with the epithelium side up and limbal edge towards limbus.
At this stage, depending on the group in which patients were allocated to, conjunctivolimbal autograft was secured in place. In first group i.e. suture group multiple interrupted 10-0 polyamide monofilament sutures (Ethicon, Johnson & Johnson, India) were used to secure autograft in place. Typically, autograft was anchored to sclera at limbus first with single superior and inferior suture. Rest of autograft margin was attached with two or three interrupted sutures.
In second group fibrin glue (Tisseel fibrin sealant Baxter AG, Vienna, Austria) was used to attach the autograft in place [Fig. 1]. The mixing of the component was done as per the manufacturer's directions. The procedure requires the addition of the fibrinolysis inhibitor, Aprotinin (small blue bottle) to the sealer protein concentrate vial (large blue bottle) followed by warming. The thrombin component is prepared by injecting the contents of calcium chloride vial (small black bottle) into the thrombin vial (large black bottle/white bottle). Large black bottle causes rapid clot formation while with white bottle rate of clot formation is slow. In our technique, the white bottle was used always so that slow clotting will give enough time to the surgeon to align the graft while attaching. The vials are then warmed for several minutes. When solutions are prepared they are drawn into two different syringes. These syringes are then placed into the duploject injector which is specially designed so that depressing the common plunger exerts simultaneous and equal pressure on both the syringes [Fig. 2]. A mixer nosecone, topped by a blunt applicator needle, is attached to the nozzle to facilitate the mixing of the two syringe components. Two to three drops of this solution were place on the scleral bed and the conjunctival autograft was immediately flipped over the area of conjunctival defect. The graft was quickly smoothed out with a non toothed forceps and edges were aligned properly while the fibrin glue clots. Operating time was noted starting from placement of lid speculum to its removal. At the end of surgery, sterile eye pad applied.
Fig. 1.
Tisseel fibrin glue kit.
Fig. 2.

Duplojet injector.
Post operatively, subjects in both groups were treated with eye drop Gatifloxacin with Prednisolone (Gatiquin P, Allergan, India) four times a day for one week which was then tapered over period of next two weeks. All patients were seen on day 1, day 3, day 7, day 14, 1 month, 3 month and 6 months post operatively. Patients were evaluated regarding presence of pain, foreign body sensation, tearing and discomfort. During each post operative visit, slit lamp bio microscopy was performed to evaluate the status of the autograft, autograft–bed integrity and development of possible complications. At the final post operative visit at 6 months, presence of recurrence if any was noted.
Results
In Group-1 i.e. suture group there were 19 males (65%) and 11 females (35%). The age of patients in suture group ranged from 36 years to 62 years with average age being 49.5 years.
In Group-2 i.e. fibrin group there were 17 males (55%) and 13 females (45%). The age of patients in fibrin group ranged from 38 years to 57 years with average age being 46.8 years [Fig. 3].
Fig. 3.
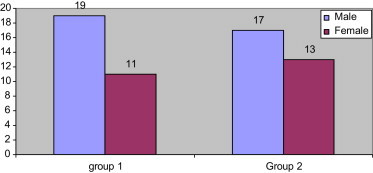
Sex distribution of patients.
The average surgical time taken for group-1 was 50.93 ± 4.96 min and group-2 was 34.43 ± 4.94 min. The mean surgical time was shorter when fibrin glue was used instead of sutures [Fig. 4]. This difference was statistically significant with p < 0.001.
Fig. 4.
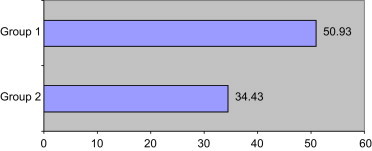
Mean surgical time.
Pain and foreign body sensation was present in all 30 cases of Group -1 on 1st post operative day. In Group -2 ie fibrin group, pain was complained by only 14 patients but foreign body sensation and lacrimation was present in 27 cases on 1st post operative day.
On subsequent visit on day 3, pain was still a major complaint in 22 patients of suture group while only 5 patients in fibrin group had pain. Foreign body sensation and lacrimation was present in 24 patients of suture group and 15 patients in fibrin group. At the end of day 7, no patient from fibrin group had pain or foreign body sensation while in suture group 8 patients had these complaints [Table 1].
Table 1.
Post operative evaluation.
| Symptoms& signs | Day 1 |
Day 3 |
Day 7 |
Day 14 |
Day 30 |
3 Month |
6 Month |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gp1 | Gp2 | Gp1 | Gp2 | Gp1 | Gp2 | Gp1 | Gp2 | Gp1 | Gp2 | Gp1 | Gp2 | Gp1 | Gp2 | |
| Pain | 30 | 14 | 22 | 5 | 8 | 0 | 5 | 0 | 2 | 0 | 0 | 0 | 0 | 0 |
| Foreign body sensation and lacrimation | 30 | 27 | 24 | 15 | 8 | 0 | 5 | 0 | 2 | 0 | 0 | 0 | 0 | 0 |
| Subconjunctival haemorrhage | 17 | 0 | 15 | 0 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Graft retraction/gaping | 3 | 3 | 3 | 3 | 5 | 3 | 5 | 3 | 5 | 3 | 5 | 3 | 5 | |
| Recurrence | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 3 | 1 |
At the end of one month, 2 patients from the suture group still had complaints of foreign body sensations.
Subconjunctival haemorrhage was a major problem noted in 17 cases of suture group while it was completely absent in fibrin group [Fig. 5].
Fig. 5.
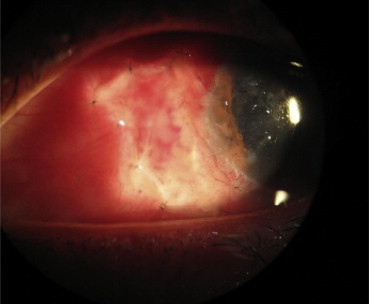
Conjunctival autograft held with sutures with haemorrhage under the graft.
Retraction of graft or gaping of edges at graft–conjunctival interface was noted in 3 cases on 1st post operative day in both groups [Fig. 6]. On 3rd post operative day and subsequent visits 5 cases of fibrin group had retraction of graft as opposes to 3 cases from suture group. Not a single case of graft loss was noted in either group.
Fig. 6.
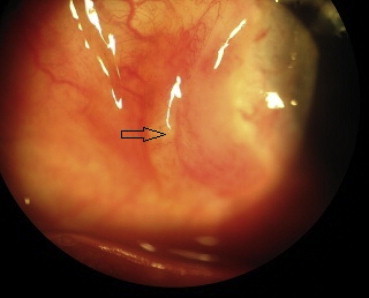
Graft retraction with fibrin glue.
All patients were evaluated for signs of recurrence of pterygium. Recurrence was noted in 2 cases at the end of 3 months post operatively in suture group. At the end of final follow up at 6 months, 3 cases from suture group and 1 case from fibrin group were noted to have recurrence. Although more number of recurrences were observed in suture group as compared to fibrin glue group the difference was not statistically significant (p 0.612).
Discussion
Pterygium is a common ophthalmic condition easy to diagnose but difficult to tackle. Various surgical techniques and their modifications have been described to manage this condition with prevention of recurrence as underlying aim. It is still an ongoing debate regarding the “ideal” pterygium surgery.
Use of a conjunctival graft to cover the bare sclera after excision of pterygium has been reported to be the most effective method of lowering recurrence rate (2–9%) and complications.5,10,12,13 The transplantation of conjunctivolimbal autograft helps to cover the limbal stem cell deficiency.11 Care should be taken to include the limbal part while harvesting the graft so that stem cells are included.13
Use of absorbable or non-absorbable sutures to secure autograft is associated with several disadvantages, including complicated surgical technique, prolonged operation time, prolonged post operative patient discomfort and suture related complications. To overcome these shortcomings tissue adhesives are being increasingly used in ophthalmology in place of sutures.14 Although the use of fibrin as a biologic adhesive was first introduced in 1909, it was not until 1944 that Tidrick et al used fibrin for skin graft fixation.15 Its use in ophthalmology was simultaneously reported by Katzin for attaching corneal transplants in rabbits.16 Tisseel fibrin sealant is a commercially available fibrin adhesive prepared from donor plasma and is as safe as other tested blood products.17
The use of fibrin glue was associated with markedly reduced surgical time. Harvey et al also showed similar statistically significant reduction in mean operative time.18 Post operative pain was less in fibrin glue than those with suture group. Also in our study pain lasted for less duration than those with suture group. Foreign body sensation present in most of the patients on 1st post operative day may be due to superficial keratectomy done during surgery. However, on subsequent days patient in fibrin group were more comfortable than those in suture group. These observations are comparable to other studies evaluating these parameters.19
Use of fibrin glue was shown to be associated with absence of haemorrhage under the graft. This can be due to activation of clotting factors with the use of glue.
Surprisingly, graft retraction was seen in more patients in fibrin glue group than suture group. The surgeon concluded that this can be due to movement of the graft due to lid movement causing displacement of the graft. Inadequate application of glue can be a causative factor. Recurrence noted was less in fibrin glue group than in suture group but not statistically significant. This is well correlated with other studies comparing sutures versus fibrin glue for conjunctival autograft.8,18–20
In summary, fibrin glue is an effective and safe method for attaching conjunctival autograft during pterygium surgery. The use of fibrin glue can ease the surgical procedure, shorten operating time and produce less post operative discomfort.
Conflicts of interest
All authors have none to declare.
References
- 1.Sihota R., Tondon R., editors. Parson's Diseases of Eye. 19th ed. Butterworth- Heinemann; 2003. Diseases of conjunctiva; pp. 193–194. [Google Scholar]
- 2.Detels R., Dhir S.P. Pterygium: a geographical survey. Arch Ophthalmol. 1967;78:485. doi: 10.1001/archopht.1967.00980030487014. [DOI] [PubMed] [Google Scholar]
- 3.Nemesure B., Wu S.Y., Hennis A., Leske M.C. Nine year incidence and risk factors for pterygium in Barbados eye studies. Ophtalmology. 2008;115:2153–2158. doi: 10.1016/j.ophtha.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 4.Allen B.D.S., Short P., Crawford G.J. Pinguecula and pterygia. Surv Ophthalmol. 1988;32:41–49. doi: 10.1016/0039-6257(88)90071-9. [DOI] [PubMed] [Google Scholar]
- 5.Spaeth E.B. Rotational island graft for pterygium. Am J Ophthalmol. 1926;9:649–655. [Google Scholar]
- 6.Sanchez-Thorian J.C., Rocha G., Yelin J.B. Meta-analysis on the recurrence rates after bare sclera resection with and without mitomycin C use and conjunctival autograft placement in surgery for primary pterygium. Br J Ophthalmol. 1998;82:661–665. doi: 10.1136/bjo.82.6.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ordman L.J., Gillman T. Studies in the healing of cutaneous wound. Arch Surg. 1996;93:857–928. doi: 10.1001/archsurg.1966.01330060001001. [DOI] [PubMed] [Google Scholar]
- 8.Cohen R.A., McDonald M.B. Fixation of conjunctival autografts with an organic tissue adhesive [letter] Arch Ophthalmol. 1993;111:1167–1168. doi: 10.1001/archopht.1993.01090090017006. [DOI] [PubMed] [Google Scholar]
- 9.Duke Elder Sir Stewart. vol VIII. Henry Kimpton; London: 1965. (System of Ophthalmology). 574. [Google Scholar]
- 10.Kenyon K.R., Wagoner M.D., Hettinger M.E. Conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology. 1985;92:1461–1470. doi: 10.1016/s0161-6420(85)33831-9. [DOI] [PubMed] [Google Scholar]
- 11.Coroneo M.T., Girolamo N.D., Wakefield D. The pathogenesis of pterygium. Curr Opin Ophthalmol. 1999;10:282–288. doi: 10.1097/00055735-199908000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Tan D.T., Chee S.P., Dear K.B., Lim A.S. Effect of pterygium morphology on pterygium recurrence in a controlled trial comparing conjunctival autografting with bare sclera excision. Arch Ophthalmol. 1997;115:1235–1240. doi: 10.1001/archopht.1997.01100160405001. [DOI] [PubMed] [Google Scholar]
- 13.Lewallen S. A randomized trial of conjunctival autografting for pterygium in the tropics. Ophthalmology. 1989;96:1612–1614. doi: 10.1016/s0161-6420(89)32667-4. [DOI] [PubMed] [Google Scholar]
- 14.Chan S.M., Boisjoly H. Advances in the use of adhesives in ophthalmology. Curr Opin Ophthalmol. 2004;15:305–310. doi: 10.1097/00055735-200408000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Tidrick R.T., Warder E.D. Fibrin fixation of skin transplant. Surgery. 1944;15:90–95. [Google Scholar]
- 16.Katzin H.M. Aqueous fibrin fixation of corneal transplants in the rabbit. Arch Ophthalmol. 1945;35:415–420. doi: 10.1001/archopht.1946.00890200422008. [DOI] [PubMed] [Google Scholar]
- 17.Gammon R.R., Avery N., Mintz P.D. Fibrin sealant: an evaluation of methods of production and the role of blood bank. J Long Term Eff Med Implants. 1998;8:103–116. [PubMed] [Google Scholar]
- 18.Harvey S.U., Reyes J.M., Flore J.D., Lim-Bon-Siong R. Comparison of fibrin glue and sutures for attaching conjunctival autografts after pterygium excision. Ophthalmology. 2005;112:667–671. doi: 10.1016/j.ophtha.2004.08.028. [DOI] [PubMed] [Google Scholar]
- 19.Sarnicola V., Vannozzi L., Motolese P.A. Recurrence rate using fibrin glue-assisted ipsilateral conjunctival autograft in pterygium surgery: 2-year follow-up. Cornea. 2010 Nov;29(11):1211–1214. doi: 10.1097/ICO.0b013e3181d5d96d. [DOI] [PubMed] [Google Scholar]
- 20.Korangy G., Seregard S., Kopp E.D. The cut and paste method for primary surgery: long- term follow- up. Acta Opthalmol Scand. 2005;83:298–301. doi: 10.1111/j.1600-0420.2005.00465.x. [DOI] [PubMed] [Google Scholar]


