Introduction
The Valsalva manoeuvre is the forced exhalation against a closed glottis. First described by an Italian anatomist in 17th century Antonio Maria Valsalva, it is now a well known entity amongst medical practitioners. It is not an innocuous manoeuvre as it appears to be. It leads to increased intra thoracic and intra abdominal pressure and raised central venous pressure. There are no valves in the venous system rostral to the heart hence a rise in the reflux venous pressure occurs in the head and neck region of the body. Preretinal haemorrhage caused by this sudden rise in venous pressure was first termed as Valsalva haemorrhagic retinopathy by Duane TD in 1972.1 Valsalva retinopathy is a rather common occurrence but its recurrence is infrequent. A case of recurrent Valsalva retinopathy in a young healthy individual which occurred following a bout of vomiting after a gap of 4 years is described. Valsalva manoeuvre like stress is a part of day to day life. This case is unique because young individuals can generate sufficiently high reflux venous pressure which can lead to rupture of capillaries. It is important to be aware of this condition not only for correct diagnosis and management but also to prevent its recurrence in future.
Case report
A 30 years old male patient presented with a sudden onset painless diminution of vision in the left eye following a bout of vomiting 7 h before at 0500 hrs in the morning. There was no history of trauma, redness, flashes, floaters or transient visual loss in the past. He gave history of having a similar episode, 4 years back in the same eye following a bout of vomiting. He was diagnosed to have subhyaloid haemorrhage. All investigations including Fundus Fluorescein Angiography(FFA) were normal. He had full visual recovery with conservative management. He did not give any history of a systemic disorder. Ophthalmic evaluation revealed vision in right eye was 6/6 and left eye was 6/36. Anterior segment examination in both eyes was unremarkable. There was no afferent pupillary defect. Fundus examination in right eye was normal. Left eye showed disc was normal. Blood vessels were normal. A large circumscribed area of preretinal haemorrhage about 4 disc diameters (DD) in size was seen in the superotemporal quadrant involving upper part of macula reaching upto fovea (Fig. 1). There were no retinal holes, tears, detachment, perivascular sheathing or snow banking at parsplana. There were no microaneurysms, hard exudates, soft exudates or neovascularisation. Amslers grid showed a relative central scotoma with metamorphopsia. Colour fundus photography and FFA were performed. FFA did not reveal any leakage. All investigations including complete blood counts, clotting parameters, biochemical parameters such as urea, creatinine and glucose were within normal limits. Systemic evaluation was carried out by the physician and no abnormality was detected. He was diagnosed as Valsalva retinopathy. The patient was followed up on conservative management he showed marked improvement. The haemorrhage resolved over a period of 6 weeks and patient had a complete visual recovery.
Fig. 1.
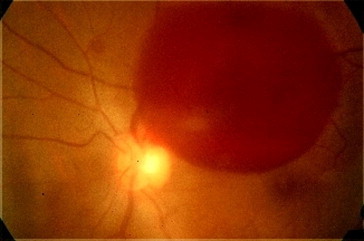
Fundus picture of left eye showing a large circumscribed area of preretinal haemorrhage about 4 DD in size in the superotemporal quadrant involving upper part of macula reaching upto fovea.
Discussion
Valsalva retinopathy was first described by Duane1 in 1972 for preretinal haemorrhages occurring as a result of sudden rise in venous pressure as seen in Valsalva manoeuvre. It is an uncommon condition and has been reported to occur with various forms of Valsalva stress such as weight lifting,2 physical exercise,3 balloon blowing,4 birth labour5 etc. The present case developed Valsalva retinopathy following a bout of emesis. Valsalva retinopathy is typically seen in young males. Ophthalmologic examination reveals either a circular or a bilobed haemorrhage6 which sometimes has a fluid level associated with it. The location can be subinternal limiting membrane (ILM) or subhyaloid. Patients with this condition are usually healthy and develop sudden visual loss when their intra thoracic or intra abdominal pressure increases suddenly such as in weight lifting, vomiting, labour etc. So a careful history taking in such cases can clinch the diagnosis. Duane1 first postulated the mechanisms for retinopathies due to distal trauma as alteration in arterial circulation (forward retinopathy), venous circulation (backward retinopathy) or to changes occurring in both systems (mixed retinopathy). Valsalva retinopathy falls in the second category. There are no valves in the venous system rostral to the heart. The sudden increase in the central venous pressure due to Valsalva stress is transmitted right upto the perifoveal capillaries which may rupture leading to preretinal haemorrhage at macula. In the present case one of the superior perifoveal capillaries appeared to have ruptured as the haemorrhage was located superior to fovea. Although Valsalva retinopathy often leads to large preretinal haemorrhages and an alarming picture the prognosis remains good and vision usually returns to normal, so the treatment usually remains conservative which was followed in the present case. However NdYAG laser has been used by some workers to puncture the posterior hyaloids and drain the blood into vitreous cavity.7 The use of NdYAG laser in such a self resolving condition with good visual prognosis is debatable as it can lead to macular hole, retinal detachment and epiretinal membrane8 (ERM).
The present case developed a recurrent episode of Valsalva retinopathy after 4 years. A case of recurrent Valsalva retinopathy has also been reported by Jung et al9 in which recurrence occurred at 3 weeks due to a similar Valsalva stress while exercising a barbell. Kim et al10 reported a case of bilateral Valsalva retinopathy in which there was bilateral recurrence after 9 months of previous episode. Literature search did not reveal any other reported instance of recurrent Valsalva retinopathy and our case appears to be only the third such case. Our case is unique because recurrence occurred after a gap of 4 years which is the longest gap after which a recurrence has occurred. Being a recurrent case a thorough evaluation was carried out to rule out an underlying cause which could not be detected. It becomes important in all cases to prevent any further recurrence by preventing any condition leading to Valsalva like stress and the patient has to be counselled accordingly.
Valsalva retinopathy occurs as a result of sudden rise in intra thoracic or intra abdominal pressure as in Valsalva manoeuvre. It has to be kept in mind in young individuals presenting with sudden diminution of vision. A careful history is the key to the diagnosis. The prognosis is good and patient needs to be counselled to avoid any such Valsalva manoeuvre like stress to prevent recurrence in future.
Conflicts of interest
All authors have none to declare.
References
- 1.Duane T.D. Valsalva haemorrhagic retinopathy. Trans Am Ophthalmol Soc. 1972;70:298–313. [PMC free article] [PubMed] [Google Scholar]
- 2.Pitta C.G., Steinert R.F., Gragoudas E.S., Regan C.D.J. Small unilateral foveal haemorrhage in young adults. Am J Ophthalmol. 1980;89:96–102. doi: 10.1016/0002-9394(80)90235-4. [DOI] [PubMed] [Google Scholar]
- 3.Roberts K.D., Mackay A.K. Microhaemorrhagic maculopathy associated with aerobic exercise. J Am Optom Assoc. 1987;58:415–418. [PubMed] [Google Scholar]
- 4.Georgiou T., Pearce I.A., Taylor R.H. Valsalva retinopathy associated with blowing balloons. Eye. 1999;13:686–687. doi: 10.1038/eye.1999.193. [DOI] [PubMed] [Google Scholar]
- 5.Ladijimi A., Zaoualis, Messaoud R. Valsalva retinopathy induced by labour. Eur J Ophthalmol. 2002;12:336–338. doi: 10.1177/112067210201200417. [DOI] [PubMed] [Google Scholar]
- 6.Pruett R.C., Carvalho A.C.A., Trempe C.L. Microhaemorrhagic maculopathy. Arch Ophthalmol. 1981;99:425–432. doi: 10.1001/archopht.1981.03930010427005. [DOI] [PubMed] [Google Scholar]
- 7.Tassignon M.J., Stempels N., Van Milders L. Retrohyaloid premacular haemorrhage treated by Q switched NdYAG laser. A case report. Graefes Arch Clin Exp Ophthalmol. 1989;227(5):440–442. doi: 10.1007/BF02172895. [DOI] [PubMed] [Google Scholar]
- 8.Kwok A.K., Lai T.Y., Chan N.R. Epiretinal membrane formation with internal limiting membrane wrinkling after NdYAG laser membranotomy in Valsalva retinopathy. Am J Ophthalmol. 2003;136(4):763–766. doi: 10.1016/s0002-9394(03)00442-2. [DOI] [PubMed] [Google Scholar]
- 9.Jung E.Y., Kion I.J., Lee E.C. A case of recurrent Valsalva retinopathy associated with exercising a barbell. J Korean Ophthalmol Soc. 2004;45(6):1040–1044. [Google Scholar]
- 10.Kim D.K., Lee W.J., Cho M.S., Kim J.S. A case of atypical Valsalva retinopathy after strenuous exercise. J Korean Ophthalmol Soc. 2005 May;46(5):915–920. [Google Scholar]


