Abstract
Background
With the trend of shortening the treatment time and reducing patient discomfort/inconveniences immediate loading of implants has emerged as an alternative approach for replacing missing natural teeth. The aim of this study is to evaluate and compare the effectiveness of immediate implant loading protocol over conventional implant loading protocol in partially edentulous mandible.
Methods
Twenty patients were selected from out patients department who needed the replacement of one of the missing mandibular first molar. They were divided into two groups. In Group A patients implants were loaded with immediate implant loading protocol, whereas in Group B they were loaded with conventional loading protocol. Periimplant bone loss and soft tissue health were measured and compared using OPG and IOPA radiographs 06 and 12 months after implant placement.
Results
One implant failed in immediate loading group (Group A), whereas all implants survived in conventional loading group (Group B). The average periimplant bone loss after 6 months and 1 year for Group A were 0.69 mm and 1.09 mm respectively, whereas it was 0.74 mm and 1.13 mm respectively for Group B. The difference in the bone loss between Group A and B was not statistically significant.
Conclusion
Immediate implant loading protocol has a highly acceptable clinical success rate in partially edentulous lower jaw although implant survival rate is slightly inferior to conventional loading protocol.
Keywords: Immediate dental implant loading, Early implant loading, Alveolar bone loss, Osseointegration, Oral hygiene, Dental plaque
Introduction
The clinical replacement of lost natural teeth by osseointegrated implants has been represented as one of the most significant advances in prosthetic dentistry. Compared to all other dental disciplines, implant dentistry has enjoyed far more innovation and progressive developments in recent years mainly in the development of new implant systems, the propagation of new and improved diagnostic procedures and the introduction of novel surgical techniques.
Formation of a direct bone-to-implant interface is the major criteria in implant dentistry. Osseointegrated dental implants have traditionally been placed in accordance with a 2 stage protocol.1 Implants were submerged and left to heal for a period of 3–4 months in mandible and 6–8 months in maxillae. Early attempts to load the implants were associated with increased failure rates.1 This meant the patients had to wait a significant time before prosthesis placement and often had to wear suboptimal provisional prosthesis. In 1990 the first investigation was published suggesting that osseointegrated implants could be loaded early or immediately in mandibles of selected patients.2 Early or immediate implant loading is now a common procedure, particularly in mandible with good bone quality.3 A Cochrane systematic review of randomized controlled clinical trials evaluating timing for the loading of dental implants suggested that immediately loaded dental implants in selected mandible can be as effective as those loaded after a conventional healing period.4
While there were no increased failure rates found for immediately loaded implants when compared to conventionally or early loaded implants in several RCTs, but many other studies also suggested that immediately loaded implants failed significantly more than conventionally loaded dental implants.1,5–8
The immediate loading of single stage implants aim at a shorter treatment period with a stable and fixed long term interim restoration on the day of surgery. This treatment option also aims at maintenance of the hard and soft tissues and reducing the waiting period.
The purpose of this study was to evaluate and compare the effectiveness of immediate implant loading protocol over conventional implant loading protocol with respect to periimplant bone loss, implant survival rate and soft tissue health around the implant in partially edentulous mandibular first molar region. This would substantiate the basis of selecting an implant loading protocol which would have reduced crestal bone loss and hence, better success rate on long term.
Material and methods
Patient selection
According to the selection criteria twenty patients were selected for this study from Out Patients Department of Army Dental Centre (R&R) who needed replacement of one of their missing first mandibular molar tooth. Patients were selected based on criteria of age group between 25 and 50 years, non-smokers, healthy remaining dentition, good oral hygiene, no retained roots or pathologic lesions, adequate inter arch clearance for implant abutment, adequate quality and quantity of bone for implant placement, no known systemic disease and availability for follow-up (Fig. 1).
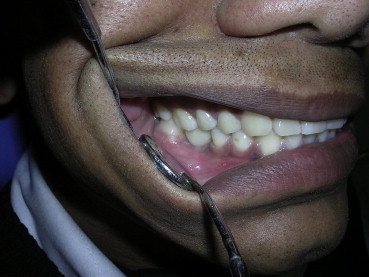
Fig. 1.

Preoperative intraoral view of the patient with teeth in occlusion.
Division of the patients
Twenty patients selected using selection criteria as mentioned above were divided into two groups (Group A and B) comprising of ten patients each. Group A comprised of patients for loading of the implant by immediate loading protocol and Group B comprised of the patients for loading of the implant by conventional loading protocol. Selection of the diameter and length of the implants were based on study casts, clinical and radiographic evaluation of available bone using an X-ray indicator (Fig. 2). Implants with widest possible diameter and maximum permissible length were selected depending on the clinical situation and preoperative radiographs. Surgical stent was fabricated in all cases for proper placement of implants. The study protocol was explained in detail to all patients and their consent for participating study was taken.
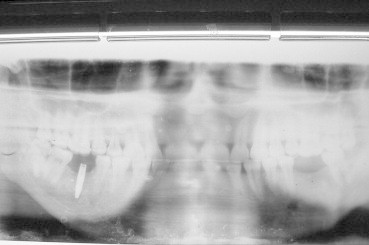
Fig. 2.

Preoperative OPG radiograph.
Surgical placement of implants
Patients were kept on oral antibiotic a day prior to implant surgery. Inferior alveolar nerve block local anesthesia was given. Under aseptic conditions an incision was made on the crest of alveolar bone using BP knife and a full thickness mucoperiosteal flap was reflected in the first molar region (Fig. 3). Using a physiodispenser and reduction gear contra-angle handpiece a channel of desired width and depth was created in the alveolar bone for the placement of implant. Nobel direct(R) single piece implants to be inserted were engaged in the channel and screwed using an implant driver (Fig. 4). Soft tissue flap was closed by using non-resorbable sutures and IOPA radiographs were taken to assess initial crestal bone level after implant placement i.e., at Time0 (T0) (Figs. 5–7).
Fig. 3.

Elevation of mucoperiosteal flap to expose the alveolar bone.
Fig. 4.

Use of pilot drill for making the channel for implant placement.
Fig. 5.
OPG radiograph after implant placement.
Fig. 6.

Post operative view of implant with teeth in occlusion.
Fig. 7.

IOPA radiograph showing alveolar bone levels on the mesial and distal side of the implant.
Patients were advised to continue the antibiotics and analgesics for three more days after the surgery. They were also instructed to maintain good oral hygiene by brushing and rinsing their mouth using 0.2% chlorhexidine gluconate mouthwash twice daily.
Prosthodontic procedures
In Group A patients implants were loaded within 48 h of implant placement using provisional crowns. Occlusion of the restoration was adjusted so that crown does not contact the opposing tooth in both intercuspal and lateral excursive movements. The finished Restorations were cemented with the eugenol free zinc oxide provisional luting cement for the easy removal of the crown for the measurements. The provisional restorations were put into light contact in Maximum Intercuspal Position after 2 months. Ceramo-metal restorations were fabricated after 6 months and were also adjusted to have light contact only in Maximum Intercuspal Position. The occlusal table of the crown was kept narrow buccolingually to reduce occlusal load on the implants (Figs. 6 and 7).
In Group B patients, after allowing 6 months of healing period for the implant to get osseointegrated, impression of the abutment and the surrounding soft tissue was made. Cast was fabricated using Type IV dental stone. Upper and lower casts were mounted on the articulator and sent to the laboratory for crown fabrication. Metal coping trial was done before porcelain application. The crowns were finished and polished. The restorations were adjusted to have light contact only in Maximum Intercuspal Position. The excursive contacts were eliminated. The occlusal table was kept narrow buccolingually to reduce occlusal load on the implants. Restorations were cemented with the eugenol free zinc oxide provisional luting cement (Fig. 8).
Fig. 8.
Intra oral view with Ceramo-metal crown in situ.
Radiographic evaluation and follow-up
The radiological evaluation was done using IOPA radiographs using paralleling (long-cone) technique to assess periimplant bone loss after 6 months [i.e., 6 months after placing the implant, at Time1 (T1)] and an year [i.e., 12 months after placing the implant, at Time2 (T2)] in both Groups A and B. A RINN framework was attached to the radiographic cone to standardize the radiographs (Fig. 9).
Fig. 9.

RINN attached to the radiographic cone for standardization.
Soft tissue evaluation
Unlike two stage implants, in single stage implants the abutment projects out of the alveolar bone after implant placement surgery. Periimplant soft tissue evaluation was done after 6 months [6 months after placement of the implant, at Soft tissue Time1 (ST1)] and 1 year after the implant placement [at Soft tissue Time2 (ST2)]. The soft tissue evaluation was done by both Principle worker and Co worker using mouth mirror and William's graduated probe. Gingival Index (GI), Plaque Index (PI) and Calculus Index (CI) were used to evaluate the soft tissues around the implant.
Results
During the study period one implant of Group A (Immediate implant loading group) failed, whereas no implant was lost in the Group B (Conventional implant loading group).
Although Group B had more periimplant bone loss than Group A, difference was statistically not significant. The average scores for soft tissue evaluation indices were not more than 01, which implies that soft tissues remained healthy around both, Groups A & B implants, even at the end of 12 months after placing the implants. One implant failed in Group A, whereas all implants survived in Group B. So 1 year implant survival rates were 90% and 100% in Group A and Group B patients respectively.
Table 1 presents the implant details with respect to their type, site and size.
Table 1.
Implant details.
| GROUP A (Patients for immediate implant loading protocol) |
GROUP B (Patients for conventional implant loading protocol) |
||||
|---|---|---|---|---|---|
| Patient Ser No. | Site | Length/Diameter (in mm) | Patient Ser No. | Site | Length/Diameter (in mm) |
| 1(I) | 46 | 4.3/10 | 1(C) | 36 | 4.3/10 |
| 2(I) | 36 | 4.3/13 | 2(C) | 36 | 4.3/13 |
| 3(I) | 36 | 3.5/13 | 3(C) | 46 | 3.5/13 |
| 4(I) | 46 | 4.3/13 | 4(C) | 46 | 4.3/13 |
| 5(I) | 36 | 4.3/10 | 5(C) | 36 | 4.3/10 |
| 6(I) | 36 | 3.5/13 | 6(C) | 36 | 3.5/13 |
| 7(I) | 36 | 4.3/13 | 7(C) | 36 | 4.3/13 |
| 8(I) | 46 | 4.3/13 | 8(C) | 46 | 4.3/13 |
| 9(I) | 46 | 3.5/13 | 9(C) | 46 | 3.5/13 |
| 10(I) | 46 | 4.3/10 | 10(C) | 46 | 4.3/10 |
Table 2 presents the mean values of crestal bone loss and soft tissue evaluation for Groups A & B implants.
Table 2.
Mean values of periimplant bone loss.
| Mean values/(±Standard deviation) | ||||
|---|---|---|---|---|
| Bone loss (in mm) and std deviation (in bracket) | ||||
| Evaluation in months | Group A |
Group B |
||
| Mesial | Distal | Mesial | Distal | |
| 06 Months (T1 − T0) | 0.71 (0.23) | 0.67 (0.22) | 0.75 (0.17) | 0.73 (0.18) |
| 12 Months (T2 − T0) | 1.11 (0.35) | 1.07 (0.37) | 1.15 (0.18) | 1.11 (0.15) |
Table 3 presents the mean values of soft tissue evaluation for Group A & B implants.
Table 3.
Mean values of soft tissue health using gingival index, periodontal index and calculus index.
| Mean values/(±Standard deviation) | ||||||
|---|---|---|---|---|---|---|
| Soft tissue evaluation and std deviation (in bracket) | ||||||
| Evaluation in months | Group A |
Group B |
||||
| GI | PI | CI | GI | PI | CI | |
| 06 Months ST1 | 0.55 (0.49) | 0.44 (0.37) | 00 (00) | 0.6 (0.64) | 0.5 (0.67) | 0.1 (0.31) |
| 12 Months ST2 | 0.88 (0.31) | 0.66 (0.47) | 00 (00) | 0.90 (0.30) | 0.70 (0.48) | 00 (00) |
Table 4 presents Paired Sample test for Group A & B implants.
Table 4.
Paired comparisons using ‘t’ values between immediately loaded and conventionally loaded implants.
| Paired differences |
t | df | Significance (2-tailed) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Std deviation | Std error mean | 95% Confidence interval of the difference |
||||||
| Lower | Upper | ||||||||
| Pair 1 | A (Mesial 06) & B (Mesial 06) | −5.5556 E-02 | 0.2963 | 9.876 E-02 | −0.2833 | 0.1722 | −0.563 | 8 | 0.589 |
| Pair 2 | A (Mesial 12) & B (Mesial 12) | −4.4444 | 0.4275 | 0.1425 | −0.3731 | 0.2842 | −0.312 | 8 | 0.763 |
| Pair 3 | A (Distal 06) & B (Distal 06) | −5.5556 E−02 | 0.3046 | 0.1015 | −0.2897 | 0.1786 | −0.547 | 8 | 0.559 |
| Pair 4 | A (Distal 12) & B (Distal 12) | −4.4444 E−02 | 0.4157 | 0.1386 | −0.3640 | 0.2751 | −0.321 | 8 | 0.757 |
Table 5 presents the statistically analyzed values. For statistical analysis, a ‘Paired t-test’ was employed to determine whether there is any statistically significant difference in bone loss between Group-A & B implants.
Table 5.
Values obtained by statistical analysis.
| Time in months | Compared pairs for bone loss | p value | Difference in bone loss (significant (S) or not significant (NS)) |
|---|---|---|---|
| 06 Months | Mesial side of Group A & Group B implants | 0.589 | NS |
| Distal side of Group A & Group B implants | 0.559 | NS | |
| 12 Months | Mesial side of Group A & Group B implants | 0.763 | NS |
| Distal side of Group A & Group B | 0.757 | NS |
Difference in bone loss is statistically significant if p value ≤ 0.05.
Discussion
It has been advocated that the surgical site should be left undisturbed for at least 3–6 months after implant placement to allow uneventful wound healing, thereby enhancing the osseointegration between implant and bone. The rationale behind this approach is that micromovement of the implant caused by the functional forces around the bone–implant interface during the wound healing may induce fibrous tissue formation between implant and bone rather than desired bone–implant contact, leading to clinical failure.9 To prevent this clinicians have attempted to reduce or minimize the concentration of forces, by avoiding the functional loading of the implant before it achieves proper osseointegration.
The amount of periimplant bone around the implant plays an important role in the success of the implant. The bone lost during the implant service reduces the total osseointegrated surface area of the implant leading to increase in the stress build up around the periimplant region which further leads to the failure of implant. Success of an implant is defined as less than 1.5 mm of marginal bone loss during first year after insertion of the prosthesis and less than 0.2 mm annual bone loss thereafter.10 Therefore it is important to minimize bone loss from the initial stage.
The duration of time gap between the implant placement and loading (functional or nonfunctional) has been investigated and reported by many authors.11–18 A consensus has yet to be reached between the authors about the ideal healing time period required between implant placement and its loading, as this period varies depending on patient specific factors (e.g., quality and quantity of available bone, loading factors, implant design and maintenance of oral hygiene etc). Implant loading protocols are generally classified according to the time period elapsed between implant placement and loading as either conventional (i.e., loaded at 3–6 months), early (i.e., loaded at approximately 6 weeks) or immediate (i.e., loaded at the time or within 48 h of implant insertion).19
The concept of immediate loading of implant is carried out to reduce the length of implant treatment, to minimize its invasiveness and complexity and also to improve its acceptance by prospective patients.11–14 This is considered to be the best option for the replacement of tooth/teeth in partially edentulous arch in esthetic zone.
A number of studies measured periimplant bone level changes in subjects with immediately loaded implants and compared them with conventional loading. Danza M et al in his randomized controlled study with 1 year follow-up showed no significant differences for marginal bone loss between immediately and conventionally loaded implants, except for slight significant difference in mandible.20 In vivo comparative study conducted by Guncu MB et al showed that immediate functional loading did not negatively affect implant stability, marginal bone levels and periimplant health when compared with conventional loading of single tooth implant.21 Schincagia et al conducted a randomized controlled trial aimed to compare single implant supported mandibular molar restorations using either an immediate or delayed loading protocol. The results of their study showed that marginal bone loss of immediate implant group was significantly lesser than delayed loaded implant.22 Sufficient data is not available to substantiate the average amount of periimplant bone loss levels of implants loaded with immediate implant loading protocol over conventional loading protocol.
Implants used in this study were TiUnite™ surface treated, tapered and threaded one piece implants (Noble Direct, Nobel Biocare, Sweden). They consist of both implant and the abutment as a single block. These single stage implants are indicated for direct insertion and direct use. Intra Oral Periapical Radiographs (IOPA) were used to measure and compare the periimplant bone loss around the implants. The periimplant bone loss is calculated by measuring distance between the top surface of the implant abutment and the first point of contact of bone with the implant surface on the radiograph immediately after the implant placement and subtracting it from the measured measurement from top surface of the implant and first point of contact of bone with the implant surface after the given time duration.
The results of study showed less amount of periimplant bone loss in Group A (Patients for immediate implant loading protocol) than Group B (Patients for delayed implant loading protocol) in 6 months after placement of the implants. The average bone loss for Group A was 0.69 mm whereas for Group B it was 0.74 mm. The difference in the bone loss between Group A and Group B was 0.05 mm. But the difference was statistically not significant. Surgical trauma and micromovement of implant caused due to the functional forces and nonfunctional forces of tongue and cheek in Group A may have caused the periimplant bone loss. Although Group B patients were not functionally loaded for 6 months, there were nonfunctional forces of tongue and cheek acting on the abutment of implant. The increased amount of bone loss seems to be as a result of disuse atrophy caused due to lack of stimulation of periimplant tissues.23
One implant of Group A failed within 6 months of insertion, whereas all implants of Group B were successful throughout the observation period. Loss of the implant may have been caused by failure of the implant to get osseointegrated because of excessive micromovement of the implant due to occlusal force or may be because of the poor quality of bone around the implant.24
Average annual crestal bone loss after 1 year of implant service with Group A implants was 1.09 mm and with Group B implants, it was 1.13 mm. Both these figures are below 1.5 mm of annual bone loss in first year of implant service and fulfill the success criteria described by Albrektsson et al.10 The immediately loaded implant group (Group A) showed less bone loss than delayed loaded group (Group B) but there was no statistically significant difference between the two groups. These results correspond to the results of other studies done by different authors.20–22,25,26
Soft tissue evaluation was done by employing Gingival Index (GI), Plaque Index (PI) and Calculus Index (CI). Since one of the etiologic factors of alveolar bone loss around implant seems to be plaque associated gingival inflammation,27–29 importance of maintaining the good oral hygiene was stressed before implant surgery as an essential requirement for successful osseointegration and maintenance of implants. Patients were also motivated for maintaining the oral hygiene. The soft tissue health was reasonably good during the entire period of evaluation as the average score for all the three indices was not more than 01, signifying mild inflammation at the most.
Conclusion and recommendations
The current study evaluated clinical outcomes of immediately loaded and delayed loaded implant protocols in partially edentulous mandibular first molar region with respect to periimplant bone levels, periodontal health and implant survival rate from the time of placement to 1 year of clinical service. Immediate implant loading protocol in partially edentulous lower jaw demonstrated a highly acceptable clinical success at the end of 1 year of implant service. But implant survival rate in immediate loading protocol was slightly inferior to conventional implant loading protocol. So this protocol can be advocated in selected patients with good bone quality and quantity. Further long term studies with larger sample sizes are necessary to evaluate periimplant bone loss, soft tissue health and success rates in order to substantiate the basis of selection of the best implant loading protocol to enhance the success rates in long term.
Intellectual contribution
Study concept: Maj Guruprasada, Maj Gen GK Thapliyal.
Drafting and manuscript revision: Maj Guruprasada.
Statistical analysis: Maj Guruprasada.
Study supervision: Maj Guruprasada, Maj Gen GK Thapliyal, Brig VR Pawar.
Conflicts of interest
This article is based AFMRC Project (No-3763/2007) and funded by the office of DGAFMS.
References
- 1.Branemark P.I., Hansson B.O., Adell R. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10 year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1–132. [PubMed] [Google Scholar]
- 2.Schnitman P.A., Wohrle P.S., Rubenstein J.E. Immediate fixed interim prosthesis supported by two-stage threaded implants: methodology and results. J Oral Implantol. 1990;16:96–105. [PubMed] [Google Scholar]
- 3.Branemark P.I., Engstrand P., Ohrnell L.O. Branemark Novum: a new treatment concept for rehabilitation of the edentulous mandible. Preliminary results from a prospective clinical follow up study. Clin Implant Dent Relat Res. 1999;1:2–16. doi: 10.1111/j.1708-8208.1999.tb00086.x. [DOI] [PubMed] [Google Scholar]
- 4.Esposito M., Grusovin M.G., Willings M., Coulthard P., Worthington H.V. Interventions for replacing missing teeth: different times for loading dental implants. Cochrane Database Syst Rev. 2007 Apr;18(2):CD003878. doi: 10.1002/14651858.CD003878.pub3. [DOI] [PubMed] [Google Scholar]
- 5.Chiapasco M., Abati S., Romeo E., Vogel G. Implant retained mandibular overdentures with Branemark system MKII implant: a prospective comparative study between delayed and immediate loading. Int J Oral Maxillofac Implants. 2001 Jul–Aug;16(4):537–546. [PubMed] [Google Scholar]
- 6.Romeo E., Chiapasco M., Lazza A. Implant-retained mandibular over dentures with ITI implants. Clin Oral Implants Res. 2002 Oct;13(5):495–501. doi: 10.1034/j.1600-0501.2002.130508.x. [DOI] [PubMed] [Google Scholar]
- 7.Cannizzaro G., Leone M. Restoration of partially edentulous patients using dental implants with a micro textured surface: a prospective comparison of delayed and immediate full occlusal loading. Int J Oral Maxillofac Implants. 2003 Jul–Aug;18(4):512–522. [PubMed] [Google Scholar]
- 8.Romanos G.E., Nentwig G.H. Immediate versus delayed functional loading of implant in posterior mandible. A 2 year prospective study. Int J Periodontics Restorative Dent. 2006 Oct;26(5):459–469. [PubMed] [Google Scholar]
- 9.Adell R., Lekholm U., Rockler B., Branemark P.I. A 15 year study of osseointegrated implants in treatment of edentulous jaw. Int J of Oral Surg. 1981 Dec;10(6):387–416. doi: 10.1016/s0300-9785(81)80077-4. [DOI] [PubMed] [Google Scholar]
- 10.Albrektsson T., Isidor F. Consensus report of session V. In: Lang N.P., Karring T., editors. Proceedings of 1st European Workshop on Periodontology. Quintessence; London: 1993. pp. 365–369. [Google Scholar]
- 11.Lazzara R.J. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989;9(5):332–343. [PubMed] [Google Scholar]
- 12.Sczwartz-Arad D., Chaushu G. Placement of implants into fresh extraction sites: 4–7 years retrospective evaluation of 95 immediate implants. J Periodontol. 1997 Nov;68(11):1110–1116. doi: 10.1902/jop.1997.68.11.1110. [DOI] [PubMed] [Google Scholar]
- 13.Wagenburg B.D., Ginsburg T.R. Immediate implant placement on removal of the natural tooth: retrospective analysis of 1081 implants. Compend Contin Educ Dent. 2001 May;22(5) 399–404, 406, 408. [PubMed] [Google Scholar]
- 14.Hahn J. Single-stage, immediate loading, and flapless surgery. J Oral Implantol. 2000;26(3):193–198. doi: 10.1563/1548-1336(2000)026<0193:SILAFS>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Salama H., Rose L.F., Salama M., Betts N.J. Immediate loading of bilaterally splinted titanium root form implants in fixed prosthodontics – a technique re-examined: two case reports. Int J Periodontics Restorative Dent. 1995 Aug;15(4):344–361. [PubMed] [Google Scholar]
- 16.Tarnow D.P., Emtiaz S., Classi A. Immediate loading of threaded implants at stage 1 surgery in edentulous arches: 10 consecutive case reports with 1–5 years data. Int J Maxillofac Implants. 1997 May–Jun;12(3):319–324. [PubMed] [Google Scholar]
- 17.Grunder U. Immediate functional loading of immediate implants in edentulous arches: two year results. Int J Periodontics Restorative Dent. 2001 Dec;21(6):545–551. [PubMed] [Google Scholar]
- 18.Degidi M., Piatelli A. Immediate functional and nonfunctional loading of dental implants: a 2–60 months follow-up study of 646 titanium implants. J Periodontol. 2003 Feb;74(2):225–241. doi: 10.1902/jop.2003.74.2.225. [DOI] [PubMed] [Google Scholar]
- 19.Cocchetto R., Vincenzi G. Delayed and immediate loading of implant in the esthetic zone: a review of treatment options. Pract Proced Aesthet Dent. 2003 Oct;15(9):691–698. [PubMed] [Google Scholar]
- 20.Danza M., Tortora P., Quaranta A., Perotti V., Vozza I., Piatelli Randomized study for the 1-year crestal bone maintenance around modified diameter implants with different loading protocols: a radiographic evaluation. Clin Oral Investig. 2010 Aug;14(4):417–426. doi: 10.1007/s00784-009-0314-0. [DOI] [PubMed] [Google Scholar]
- 21.Guncu M.B., Aslan Y., Tumer C., Guncu G.N., Uysal S. In patient comparison of immediate and conventional loaded implants in mandibular molar sites within 12 months. Clin Oral Implants Res. 2008 Apr;19(4):335–341. doi: 10.1111/j.1600-0501.2007.01471.x. [DOI] [PubMed] [Google Scholar]
- 22.Fischer K., Bäckström M., Sennerby L. Immediate and early loading of oxidized tapered implants in the partially edentulous maxilla: a 1-year prospective clinical, radiographic, and resonance frequency analysis study. Clin Implant Dent Relat Res. 2009 Jun;11(2):69–80. doi: 10.1111/j.1708-8208.2008.00096.x. Epub 2008 Apr 1. [DOI] [PubMed] [Google Scholar]
- 23.Bilhan H., Mumku E., Arat S. The role of timing of loading on later marginal bone loss around dental implants: a retrospective clinical study. J Oral Implantol. 2010;36(5):363–376. doi: 10.1563/AAID-JOI-D-09-00078. [DOI] [PubMed] [Google Scholar]
- 24.Cochran D.L. The evidence for immediate loading of implants. J Evid Based Dent Pract. 2006 Jun;6(2):155–163. doi: 10.1016/j.jebdp.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 25.Shibly O., Kutkut A., Patel N., Albandar J.M. Immediately implants with immediate loading vs. conventional loading: 1-year randomized clinical trial. Clin Implant Dent Relat Res. 2010 Oct 26 doi: 10.1111/j.1708-8208.2010.00310.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 26.Crespi R., Cappre P., Gherlone E., Romanos G.E. Immediate versus delayed loading of dental implants placed in fresh extraction sockets in the maxillary esthetic zone: a clinical comparative study. Int J Oral Maxillofac Implants. 2008 Jul–Aug;23(4):753–758. [PubMed] [Google Scholar]
- 27.Tang Z., Sha Y., Lin Y., Zhang G., Wang X., Cao C. Periimplant mucosal inflammation and bone loss: clinical and radiographic evaluation of 108 dental implants after 1-year loading. Chin J Dent Res. 2000 Aug;3(2):15–20. [PubMed] [Google Scholar]
- 28.Kracher C.M., Smith W.S. Oral health maintenance dental implants. Dent Assist. 2010 Mar–Apr;79(2):27–35. [PubMed] [Google Scholar]
- 29.Heasman P., Esmail Z., Barclay C. Peri-implant diseases. Dent Update. 2010 Oct;37(8):511–512. doi: 10.12968/denu.2010.37.8.511. 514–516. [DOI] [PubMed] [Google Scholar]


