Introduction
Conjoined twins are the most extreme form of twinning, occurring in about 1% of monozygotic twins with incidence of about 1 in 50,000 to 1 in 100,000 births. However 60% are still born or die shortly after, the true incidence is around 1 in 200,000 live births.1 The antenatal diagnosis is difficult clinically but extremely important. The prenatal diagnosis of conjoined twins is usually suggested at prenatal sonography, which has the advantage of offering a safe, accurate, and reliable method of detecting anomalies of foetal growth and structure.2,3 However, because of the intrinsic limitation of sonography with regard to tissue contrast, MRI has been explored as a safe alternative. We present a case of conjoined twin (Craniopagus and Thoraco-omphalopagus) diagnosed by ultrasound and MRI at 15 weeks of gestation.
Case report
A 26 years old Gravida 3, Para 2, living 2 lady at 14 weeks period of gestation, had come for booking at our tertiary level antenatal care (ANC) OPD. Besides routine antenatal investigations anomaly ultrasound scan was done. Ultrasonography performed at our foetal medicine centre revealed four extremities two cardiac structures, two stomach single foetal head with prominent orbits and a liver. Ultrasound diagnosis of conjoined twin was made [Fig. 1]. Antenatal MRI was advised to confirm ultrasound findings and for academic interest with consent of patient. MRI showed complete fusion of the cranium and the thoracic cavities. The frontal lobe of the two foetuses appeared fused with a small face oriented in the Sagittal plane to one side of the heads. Only one pair of eyes was seen. Extreme hypotelorism and micrognathia were noted. Two separate spinal canals and cardia were seen. The livers were fused with separation of twins just at the level of the single umbilical cord. MRI diagnosis of conjoined twins with Craniopagus and Thoraco-omphalopagus was made [Fig. 2]. After proper counselling patient opted for termination of pregnancy. Foetal autopsy confirmed ultrasound and MRI findings [Fig. 3]. Sex of abortus was female.
Fig. 1.
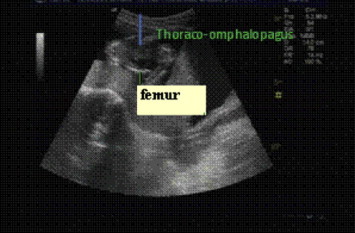
Ultrasound picture of conjoined twin.
Fig. 2.
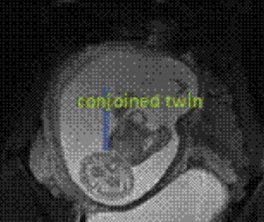
MRI picture of conjoined twin showing complete fusion of cranium and thoracic cavities. (Craniopagus and Thoraco-omphalopagus.)
Fig. 3.

Gross specimen of aborted conjoined twin.
Discussion
Conjoined twins being the most extreme form of monozygotic twinning, occur in about 1% of monozygotic twins. It is proposed that the origin of conjoined twins is at the primitive streak stage of the embryonic plate (15–17 days), and results from an error in blastogenesis due to incomplete fission of a single zygote. Most conjoined twins are female approximately 70–75%, and most are born prematurely with an extremely high mortality rate.3 The prenatal diagnosis may be suspected and confirmed if two foetuses cannot be visualized separately in a single gestational sac. Bifid appearance of the first trimester foetal pole, presence of more than three umbilical cord vessels, persistence of heads at the same level and body plane, and failure of the foetuses to change position relative to each other over time are other sonographic features that assist in making the diagnosis.4 The lack of ionizing radiation in both sonography and MRI make them ideal prenatal imaging modalities. Because of its low cost, wider availability, and real-time imaging, sonography has been the method of choice for in utero imaging and prenatal detection of foetal structural and growth anomalies. However in the presence of maternal obesity or Oligohydramnios, and because of limited sonographic ability to differentiate soft tissues, MRI provides an excellent and accurate alternative technique.
Also, MRI offers superior tissue contrast and greater clinical information during the third trimester of the pregnancy, when the foetus is larger and less mobile.5 Given its superior tissue differentiation, larger field of view and no known adverse biologic effect on the foetus, ultra fast MRI will likely gain an important role in antenatal diagnosis of foetal anomalies in the future, especially when sonographic findings of the foetus are ambiguous or uncertain.6 An early diagnosis of conjoined twins is important so that early termination can be performed after counselling couple.
Conflicts of interest
All authors have none to declare.
References
- 1.Spitz L., Kiely E.M. Experience in the management of conjoint twins. Br J Surg. 2002;89:1188–1192. doi: 10.1046/j.1365-2168.2002.02193.x. [DOI] [PubMed] [Google Scholar]
- 2.Goldberg Y., Ben Shlomo, Weiner E., Shaleu E. First trimester diagnosis of conjoined twins. Hum Reprod. 2000;5(6):1413–1415. doi: 10.1093/humrep/15.6.1413. [DOI] [PubMed] [Google Scholar]
- 3.Sherer D.M., Dalloul M., Kheyman M. Transvaginal color Doppler imaging diagnosis of thoracopagus conjoined twins at 7 weeks gestation. J Ultrasound Med. 2006;25:1485–1487. doi: 10.7863/jum.2006.25.11.1485. [DOI] [PubMed] [Google Scholar]
- 4.Sharma U.K., Dangol A., Chawala C.D., Shrestha D. Antenatal detection of conjoined twins. J Nepal Med Assoc. 2007;46(167):133–135. [PubMed] [Google Scholar]
- 5.Spielmann A.L., Freed K.S., Spritzer C.E. MRI of conjoined twins illustrating advances in fetal imaging. J Comput Assist Tomo. 2001;25:88–90. doi: 10.1097/00004728-200101000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Usta I.M., Awwad J.T. A false positive diagnosis of conjoined twins in a triplet pregnancy: pitfalls of first trimester ultrasonographic prenatal diagnosis. Prenat Diagn. 2000;20:169–170. doi: 10.1002/(sici)1097-0223(200002)20:2<169::aid-pd768>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]


