Abstract
Background
Iron deficiency anaemia (IDA) is the most common cause of anaemia in pregnancy in Indians and is associated with increased risk of low birth-weight infants. Studies from developed countries recommend iron supplementation based on serum ferritin levels. However, screening by serum ferritin is not feasible in all cases in India. This study was undertaken to document haematological profile of pregnant Indian women.
Methods
We studied the correlation between second and third trimester ferritin concentration and haemoglobin (Hb) and red cell indices in 100 consecutive ANC cases to select the best haematologic characteristic to identify women who needed iron therapy. Hb and red cell indices, RBC count, mean corpuscular volume, mean corpuscular haemoglobin, mean corpuscular haemoglobin concentration, red cell distribution width were analysed and PBS studied to subtype anaemia if present.
Results
Proportion of iron deficiency anaemia in pregnancy was 34% and significant correlation was found between serum ferritin and RDW-CV% and TRBC. No correlation was found between ferritin levels and Hb, MCV, MCH and MCHC. Serum ferritin levels were <12 ng/mL in 30 out of 52 non-anaemic cases suggesting prevalence of sub-clinical iron deficiency in 58% cases. None of the red cell indices correlated with ferritin level in this group. Only TRBC showed some correlation with ferritin (r = −0.090, p > 0.05).
Conclusion
All pregnant women in India should continue to get iron supplements unlike what is recommended in the developed countries where iron supplementation is based on serum ferritin levels.
Keywords: Serum ferritin, Iron deficiency, Antenatal cases, Red cell indices
Introduction
Anaemia in pregnancy is a major health problem in many developing countries including India, where nutritional deficiency, malaria and other parasitic infections contribute to increased maternal and perinatal mortality and morbidity.1,2 Iron deficiency is the most common cause of anaemia in pregnancy worldwide and associated with increased risk of preterm births and low birth weight infants.3,4 Furthermore, mothers given iron supplementation have decreased risk of preterm delivery.5 Recently, there have been western studies which advocate the discontinuation of iron supplementation in pregnancy due to teratogenic effects.6 A recent Cochrane Review of 2009 has found that excessive prenatal iron can have side effects and needs to be taken as per need.7 In a developing country like India with high prevalence of sub-clinical iron deficiency and the gold standard test – serum ferritin too expensive to be done in all cases, we need to know whether western study results are applicable in our settings and what are the surrogate markers for reliably predicting iron deficiency to guide prophylaxis and therapy?
Anaemia in pregnancy has been defined by criteria from the Centers for Disease Control and Prevention (CDC) as a haemoglobin level of less than 11 g per dL during the first and third trimesters and less than 10.5 g per dL during the second trimester.8 The reason for this lower cut-off value is the haemo-dilution in pregnancy due to plasma volume expansion of 30–40% exceeding the 20–25% increase in red cell mass. As a consequence there is a dilutional drop in Hb concentration creating a low viscosity state promoting oxygen transport to the tissues including placenta. As there is physiological macrocytosis with average increase of 4 fL at term, the normal cut-off of MCV <78 fL to screen cases of iron deficiency anaemia may not hold in pregnant women.3 However, in India and most of the other developing countries the lower limit is often accepted as 10 gm per dL.
Ferritin level of <12 ng/dL is considered as the gold standard for the diagnosis of iron deficiency anaemia in pregnancy.5,9 It is superior to transferrin saturation or serum iron in the diagnosis of IDA as its concentration correlates with bone marrow iron stores. Also, even with iron deficiency, serum iron can be high or normal if the pregnant female is on oral iron.10 The estimation of ferritin is expensive and cannot be routinely done in all, thus there is a need for surrogate markers to identify women who need iron supplementation. It is also necessary to determine the usefulness of red cell indices in diagnosing iron deficiency anaemia as well as sub-clinical iron deficiency longitudinally during the course of pregnancy.
Published guidelines indicate acceptable levels for Hb and red cell indices in pregnancy but they are population specific and there is no evidence confirming their applicability in Indian pregnant woman.8,11–13 This study was therefore undertaken with the intent of documenting the haematological profile of pregnant Indian women and comparing these to the established norms to determine whether the norms apply or whether there was a need to establish local norms.
Material and methods
The study was carried out in 100 consecutive pregnant women in the second and third trimester (12–40 wks) reporting to the antenatal OPD of a Medical College Hospital at Pune. Institutional ethical clearance was obtained. After informed consent, blood samples were collected 2 ml in EDTA and 3 ml in sterile vacutainer. The EDTA anticoagulated sample was used for estimation of Hb and the red cell indices on a Coulter Act 3 part automated Haematology cell counter. The red cell indices assayed were total RBC count, mean corpuscular volume (MCV), mean corpuscular haemoglobin (MCH), mean corpuscular haemoglobin concentration (MCHC), red cell distribution width coefficient of variation (RDW-CV%). A peripheral smear was seen to subtype the anaemia. If thalassaemia trait was suspected on basis of red cell indices in any of the cases, haemolysate was made from the left over sample in EDTA to estimate HbA2 and the patient's treating obstetrician was informed to ensure testing of the spouse and genetic counselling. The serum was separated from the sample in sterile tube and ferritin levels measured by ELISA test.
The data of the red cell indices and ferritin levels were analysed by SPSS 16. Scatter plots were constructed between serum ferritin and RDW-CV%, RBC count, Hb, MCV, MCH and MCHC and between MCV and Hb. Non-parametric test was done wherever required. Receiver operator characteristic (ROC) curves were drawn to look at maximum sensitivity and specificity for Hb, MCV, MCH, MCHC and RDW-CV% to look for statistically significant correlation with serum ferritin and also to see which one gave maximum area under curve (AUC).
Results
A total of 100 consecutive pregnant women in the second and third trimester were studied. The mean age was 22.34 years (SD = 2.92). Taking a cut-off of Hb of 10.5 g/dL and 11 g/dL or anaemia in 2nd and 3rd trimester respectively as per CDC recommendation and ferritin of ≤12 ng/mL for presence of iron deficiency, it was found that 48 out of 100 had anaemia and 52 were non-anaemic. 34 ladies had iron deficiency anaemia and iron deficiency without anaemia was seen in 30/52 (58%) of non-anaemic ladies. Three of the non-iron deficiency anaemia individuals had thalassaemia trait, 4 folate deficiency and rest 7 had mild anaemia due to pregnancy. Table 1 shows the distribution of these cases.
Table 1.
Description of study participants as per anaemic status.
| Iron deficiency anaemia (Hb ≤10.5 g/dL; ferritin ≤12 ng/mL) | 34 |
| Anaemia not due to iron deficiency (Hb ≤10.5 g/dL; ferritin >12 ng/mL) | 14 |
| Non-anaemic with normal ferritin (Hb >10.5 g/dL; ferritin >12 ng/mL) | 22 |
| Non-anaemic with iron deficiency (Hb >10.5 g/dL; ferritin ≤12 ng/mL) | 30 |
The mean, median mode and SD of all red cell indices, Hb and serum ferritin of all cases were calculated. Scatter plots were drawn to look for correlation of red cell indices with ferritin (Figs. 1 and 2). Significant correlation was seen between serum ferritin and RDW-CV% and RBC count (Pearsons Corr coeff (r) = −0.420, p = 0.013). No correlation was seen between ferritin levels and MCV (r = 0.058, p = 0.458), Hb (r = 0.078, p = 0.40), MCH (r = 0.052, p = 0.605) and MCHC (r = 0.035, p = 0.728) (Figs. 3–5). When MCV and Hb levels were assessed, significant correlation was found between the two (r = 0.496, p = 0.000).
Fig. 1.
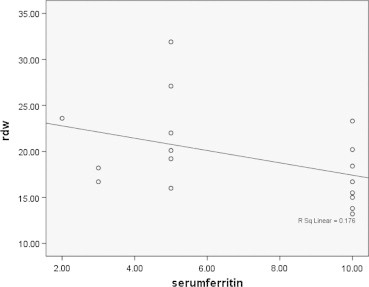
Scatter plot of RDW-CV% and serum ferritin in 34 cases with iron deficiency anaemia. Pearson Correlation coefficient = −0.420; p = 0.013.
Fig. 2.
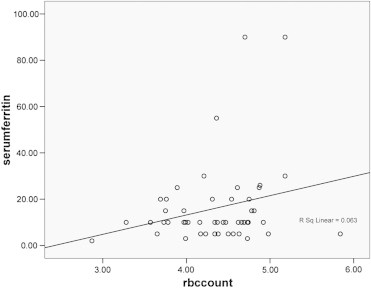
Scatter plot showing correlation between serum ferritin and RBC count. Pearson Correlation coefficient = 0.251; p = 0.012.
Fig. 3.
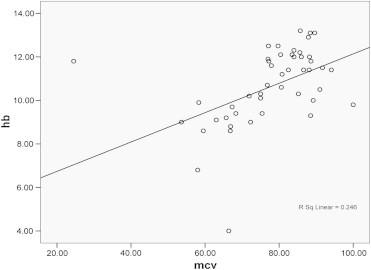
Scatter plot of haemoglobin and MCV. Pearson Correlation coefficient = 0.496; p = 0.000.
Fig. 4.
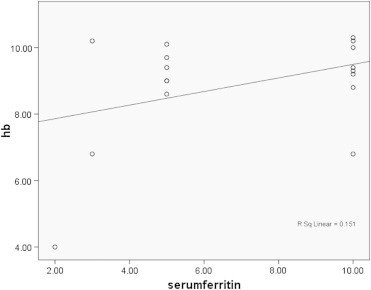
Scatter plot of haemoglobin and serum ferritin in 34 cases with iron deficiency anaemia. Pearson Correlation coefficient = −0.389; p = 0.023.
Fig. 5.
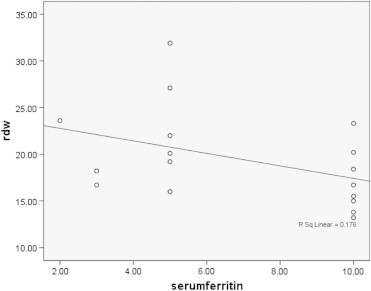
Scatter plot of RDW-CV% and serum ferritin in 34 cases with iron deficiency anaemia. Pearson Correlation coefficient = −0.420; p = 0.013.
Analysis of the difference of means of various indices showed Hb, MCV, MCH, MCHC, and total RBC to be significantly lower (p = 0.000, 0.000, 0.000, 0.000 and 0.012, respectively) and RDW-CV% to be significantly higher (p = 0.010) in the IDA cases. Serum ferritin was significantly lower in the IDA cases as compared to other pregnant women and 58% of non-anaemic had ferritin levels ≤12 ng/dL. This difference was statistically significant (p = 0.000, Mann–Whitney test).
Correlation of red cell indices and Hb with serum ferritin was assessed for 34 IDA cases using scatter plot graphs to see if they could pick up IDA. The Hb, MCV, MCH and RDW-CV% showed significant correlation with serum ferritin levels in IDA cases (p = 0.023, 0.021, 0.035, 0.013, respectively). Though MCHC and RBC count showed some correlation with serum ferritin (r = 0.337 and 0.087, respectively) but it was not statistically significant.
ROC curves were drawn to look at maximum sensitivity and specificity for indices which showed statistically significant correlation with serum ferritin and also to see which one gave maximum area under curve (AUC). Table 2 shows the area under ROC curves for various red cell indices for diagnosis of iron deficiency in ANC cases. ROC for Hb was found to give the maximum area under its curve and it was seen that Hb <9.7 g/dL can predict iron deficiency anaemia in the second and third trimester with a sensitivity of 90.9% and specificity of 79.1% (Fig. 6).
Table 2.
Area under ROC curve and the best cut-off for various red cell indices for diagnosis of iron deficiency in ANC cases.
| S. No. | Index | Area under the curve | Best cut-off | Sensitivity % | Specificity % |
|---|---|---|---|---|---|
| 1. | RBC | 0.688 | ≤4.18 million/cumm | 75.8 | 59.0 |
| 2. | Hb | 0.951 | ≤9.7 gm/dL | 90.9 | 79.1 |
| 3. | MCV | 0.790 | ≤76.1 fL | 84.8 | 78.2 |
| 4. | MCH | 0.821 | ≤25.05 pg | 81.8 | 82.4 |
| 5. | MCHC | 0.808 | ≤31.35 g/dL | 84.8 | 76.5 |
| 6. | RDW-CV% | 0.777 | ≥16.35% | 82.4 | 75.8 |
Fig. 6.
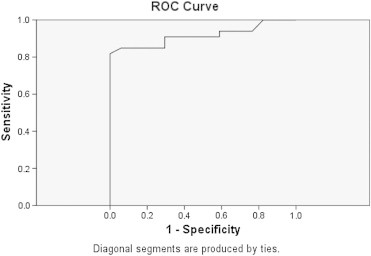
ROC curve for haemoglobin in predicting iron deficiency anaemia. Area under curve = 0.915. The best cut-off is Hb <9.7 gm/dL with a sensitivity of 90.9% and specificity of 79.1%.
The 14 non-iron deficiency anaemia comprised of 3 cases of β-thalassaemia trait, 4 folate deficiency and the rest mild anaemia due to pregnancy. The cases of β-thalassaemia trait were suspected on the basis of red cell indices i.e. low MCV, high TRBC and low/normal RDW. The diagnosis was confirmed if HbA2 >3.7%. The number of cases in this sub-group was too small for further sub-group analysis.
As there were 52 non-anaemic cases with 30 (58%) having serum ferritin levels (≤12 ng/mL), we looked at the correlation between ferritin and red cell indices in this group to see if any index can predict the presence of sub-clinical iron deficiency in this group. None of the red cell indices were found to correlate with the red cell indices in non-anaemic pregnant women.
Discussion
In the 52 non-anaemic cases we found ferritin ≤12 ng/dL in 30 ladies, thus giving a proportion of 58% iron deficiency in non-anaemic pregnant women. The total number with iron deficiency (anaemic and non-anaemic) was 64 out of 100. The present study shows that anaemia as well as iron deficiency anaemia is very common in India as compared to the developed countries.2 The other major problem in our country is sub-clinical iron deficiency without anaemia (serum ferritin ≤12 ng/dL and Hb >10.5 g/dL) which was seen in 58% non-anaemic pregnant women.
As for correlation of ferritin levels with red cell indices in all the 100 cases, we did not find any correlation between ferritin and Hb, MCV, MCH, MCHC respectively. In the whole group only RDW-CV% and RBC count correlated with the ferritin levels and these findings were similar to those of a study from USA12 on African–American population where the results showed that Hb ≤9.7 g/dL and RDW ≥15 (at gestational age <20 weeks) predicted iron deficiency with high specificity.
The present study showed that in second and third trimester pregnant women with Hb <10.5 g/dL (anaemic) the MCV, MCH, MCHC, RBC count and RDW-CV% correlate with the ferritin levels and can help in the diagnosis of iron deficiency anaemia. Our findings were different from that of a study from Malaysia which found correlation only between Hb and ferritin levels.13
Our study shows that the red cell indices available on the automated Haematology cell counters available routinely in India do not correlate with sub-clinical iron deficiency as most of these cases do not develop changes in these indices. Our findings were different from another study which concluded that in early iron deficiency and during recovery the full blood count shows the Hb near the lower limit of normal with a low MCV and a high RDW-CV%.14 The rise in MCV of 4 fL which occurs in pregnancy may have a role to play.3 Thus the normal cut-off of MCV <78 fL to screen cases of iron deficiency anaemia may not hold true in pregnant women.
By drawing ROC curves for various red cell indices for diagnosis of IDA, we found that the maximum area to be for Hb and a cut-off <9.7 g/dL had a sensitivity of 90.9% and a specificity of 79% in the diagnosis of Indian pregnant women. This was similar to the cut-off of 9.7 g/dL given in the study among African–Americans in USA.12 Though all indices had a statistically significant correlation with ferritin for IDA the next best index was MCH (area = 0.821; cut-off of <31.35 giving sensitivity of 81.8% and specificity of 82.4%). As per our study in cases with Hb <10.5 g/dL a combination of MCV <76.1 fL, MCH <25.05 pg, MCHC <31.35%, RDW-CV% >16.35% and RBC count <4.18 million/cumm can help in the diagnosis of iron deficiency anaemia in pregnant Indian women in the second and third trimester.
As for picking up iron deficiency in non-anaemic pregnant women, to help decide whom to continue giving iron therapy our study did not find any indicator to help pick up the women with ferritin <12 ng/dL. As earlier studies also did not help a recent study found that haematinic deficiency in pregnancy results in increased stimulation of erythroid progenitor cells by erythropoietin.15 However, as this is not an easily available test and not cost effective, workers from Europe have worked on newer indices which are available on the new automated cell counters like ADVIA 120 haematology system and found that percentage of hypochromic red blood cells (%HYPOm) and reticulocytes (%HYPOr), and cellular haemoglobin in reticulocytes (CHr) were in good agreement with the results based on the usage of a combination of three commonly used tests (Hb, MCV, ferritin).16 The same group in another study published in 2008 has shown that elevated %HYPOm and %HYPOr reflecting iron-deficient erythropoiesis are associated with an increase in EPO concentration in maternal blood and can help pick up sub-clinical iron deficiency as it is accompanied by a compensatory EPO response. Further studies are needed to determine the usefulness of the cell indices in diagnosing iron deficiency longitudinally during the course of pregnancy and may be similar studies should be done in India once such cell counters are cheaper and available in India.
Iron and folic acid supplementation is recommended for all antenatal cases in developing world, but some studies have highlighted the adverse effects of iron supplementation in the West where the prevalence of iron deficiency is very low.6,7 The issue is still debatable as an earlier Cochrane Review on the withdrawal of iron supplementation published in 20072 recommended the continuation of supplementation. We recommend continuation of supplementation by iron in pregnancy as has been recommended by NNACP17 as we found 58% of non-anaemic pregnant women in second and third trimester to have serum ferritin levels <12 ng/dL.
Conclusion
Thus the international norms were found to be applicable to the pregnant Indian women and to similar populations with same stage of development as India. Also, we have concluded that we have to look for newer surrogate markers for diagnosis of sub-clinical iron deficiency in Indian women. In view of this and that 58% of non-anaemic pregnant women had iron deficiency, we recommend that all pregnant women in India should get iron supplements unlike what is recommended in the developed countries where iron supplementation is based on serum ferritin levels.
Intellectual Contribution of Authors
Study concept: Col Jyoti Kotwal, Brig Sanjiv Chopra, vsm.
Data Collection and Aanalysis: Lt Manu Tiwari, Anupam Kotwal.
Drafting of Manuscript: Maj Priyanka Mishra, Col Jyoti Kotwal.
Study Supervision: Brig Vibha Dutta, sm, Col Jyoti Kotwal, Brig Sanjiv Chopra, vsm.
Conflicts of interest
All authors have none to declare.
References
- 1.http://www.nfhsindia.org/nfhs3.html
- 2.Mahomed K. Iron and folate supplementation in pregnancy. Cochrane Database Syst Rev. 2007;3:CD001135. doi: 10.1002/14651858.CD001135. [DOI] [PubMed] [Google Scholar]
- 3.Cuervo L.G., Mahomed K. vol. 80(1) John Wiley & Sons, Ltd (Level I); Chichester, UK: 2003. Treatments for iron deficiency anaemia in pregnancy (cochrane review) p. 92. (The Cochrane Library). Issue 4. [Google Scholar]
- 4.Singla P.N., Tyagi M., Kumar A., Dash D., Shankar R. Fetal growth in maternal anaemia. J Trop Pediatr. 1997;43:89–92. doi: 10.1093/tropej/43.2.89. [DOI] [PubMed] [Google Scholar]
- 5.Scholl T.O., Hediger M.L., Bendich A., Schall J.I., Smith W.K., Krueger P.M. Use of multivitamin–mineral prenatal supplement: influence on the outcome of pregnancy. Am J Epidemiol. 1997;146:134–141. doi: 10.1093/oxfordjournals.aje.a009244. [DOI] [PubMed] [Google Scholar]
- 6.Lao T.T., Tam K.F., Chan L.Y. Third trimester iron status and pregnancy outcome in non-anaemic women; pregnancy unfavourably affected by maternal iron excess. Hum Reprod. 2000;15(8):1843–1848. doi: 10.1093/humrep/15.8.1843. [DOI] [PubMed] [Google Scholar]
- 7.Peña-Rosas J.P., Viteri F.E. Effects and safety of preventive oral iron or iron + folic acid supplementation for women during pregnancy. Cochrane Database Syst Rev. 2009;(4) doi: 10.1002/14651858.CD004736.pub3. CD004736. pub3. Art. No.: CD004736. [DOI] [PubMed] [Google Scholar]
- 8.CDC criteria for anemia in children and childbearing-aged women. MMWR Morb Mortal Wkly Rep. 1989;38:400–404. [PubMed] [Google Scholar]
- 9.Crichton R.R. The biochemistry of ferritin. Br J Haematol. 1992;26:677–681. doi: 10.1111/j.1365-2141.1973.tb01695.x. [DOI] [PubMed] [Google Scholar]
- 10.Romslo I., Haram K., Sagen N., Augensen K. Iron requirement in normal pregnancy as assessed by serum ferritin, serum transferrin saturation and erythrocyte protoporphyrin determinations. Br J Obstet Gynaecol. 1984;90:101–105. doi: 10.1111/j.1471-0528.1983.tb08891.x. [DOI] [PubMed] [Google Scholar]
- 11.James T.R., Reid H.L., Mullings A.M. Are published standards of haematological indices in pregnancy applicable across populations: an evaluation of healthy pregnant Jamaican women. BMC Pregnancy Childbirth. 2008 doi: 10.1186/1471-2393-8-8. doi:0.1186/1471; ppl-7[3] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Casanova B.F., Sammel M.D., Macones G.A. Development of a clinical prediction rule for iron deficiency anemia in pregnancy. Trans R Soc Trop Med Hyg. 2003;97(3):273–276. doi: 10.1016/j.ajog.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 13.Hassan R., Abdullah W.Z., Nik Hussain N.H. Anemia and iron status of Malay women attending an antenatal clinic in Kubang Kerian, Kelantan, Malaysia. Am J Obstet Gynecol. 2005;193(2):460–466. [PubMed] [Google Scholar]
- 14.Dugdale A.E. Predicting iron and folate deficiency anaemias from standard blood testing: the mechanism and implications for clinical medicine and public health in developing countries. P N G Med J. 2003;46(3–4):143–151. doi: 10.1186/1742-4682-3-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McMullin M.F., White R., Lappin T., Reeves J., MacKenzie G. Haemoglobin during pregnancy: relationship to erythropoietin and haematinic status. Eur J Haematol. 2005;71(1):44–50. doi: 10.1034/j.1600-0609.2003.00085.x. [DOI] [PubMed] [Google Scholar]
- 16.Ervasti M., Kotisaari S., Heinonen S., Punnonen K. Use of advanced red blood cell and reticulocyte indices improves the accuracy in diagnosing iron deficiency in pregnant women at term. Eur J Haematol. 2007 Dec;79(6):539–545. doi: 10.1111/j.1600-0609.2007.00964.x. [DOI] [PubMed] [Google Scholar]
- 17.Gautam C.S., Saha L., Sekhri K., Saha P.K. Iron deficiency in pregnancy and the rationality of iron supplements prescribed during pregnancy. Medscape J Med. 2008;10(12):283. [PMC free article] [PubMed] [Google Scholar]


