Abstract
Background
To ascertain the prevalence of malocclusion and orthodontic treatment need in schoolchildren dependent on armed forces personnel. To review the overall oral health using DMFT index and to evaluate any relation between increased DMFT index to existing orthodontic problems.
Method
Five schools were randomly selected among Army/KV/AF schools and a random sample of 1200 children aged 10–15 years old attending these schools dependant on armed forces personnel were selected. A survey form was filled up after the examination of children by the principal worker and need for orthodontic treatment was assessed using index for orthodontic treatment need (IOTN) and overall oral health status by DMFT index and totaled. Frontal intra oral photograph in centric occlusion were taken. Dental Health Component (DHC) of IOTN for all the patients was marked by one set of orthodontists. The most severe occlusal trait was identified by the examiner for any particular patient and the patient was then categorized according to this most severe trait. AC of the IOTN was assessed by second orthodontist, individual and a layperson.
Results
It was observed that prevalence of malocclusion in the sample was 53.7%. 32.8% (239 males & 154 females) of samples are in need of orthodontic treatment. 55.1% of samples shown no caries risk, 38.1% had moderate caries risk and 6.8% had high caries risk.
Conclusion
Significant percentage of the samples are in need for orthodontic treatment. There is significant relation between higher DMFT index and orthodontic treatment need. It was found that IOTN is a reliable and user-friendly index, which can be used for orthodontic surveys.
Keywords: Index for orthodontic treatment need (IOTN), Dental health component (DHC), Aesthetic component (AC), Decayed-missing-filled teeth index (DMFT index)
Introduction
The goal of orthodontic treatment is to attain optimal occlusion within the framework of function, stability and esthetics. The oral-facial region is usually an area of significant concern for the individual because it draws the most attention from other people in interpersonal interactions and is the primary source of vocal, physical, and emotional communication. As a result, patients who seek orthodontic treatment are concerned with improving their appearance and social acceptance, often more than they are with improving their oral function or health. Enhancing these aspects of quality of life is an important motive for undergoing orthodontic treatment. Regardless of age, patients and their parents or caregivers expectations about improvements in oral function, esthetics, social acceptance, and body image are important for both general dentists and orthodontists to consider when advising patients about these procedures and during the treatment process.1
Orthodontic anomalies have been associated with psychosocial distress2,3 poor periodontal condition4 and impaired masticatory function5 and so should be regarded as a health problem. While there is evidence that certain features such as traumatic deep overbite, unprotected incisors and impacted teeth may adversely affect the longevity of the dentition, the relationship of dental irregularity to periodontal disease, caries and mandibular dysfunction is less certain.6
Clinicians, patients and their families may have differing views of what should be treated and what should be accepted as a modest and harmless variation. There is also likely to be variation among groups of clinicians and also between primary care referring practitioners and specialist orthodontists. A variety of social, economic, and cultural factors (esthetic judgment, income, and availability of providers) may influence personal perception of the need for orthodontic treatment.7
Although data on orthodontic awareness and treatment needs are very scanty, malocclusion is undoubtedly a public health concern in young populations. There are few studies to estimate the proportion of the population that requires orthodontic treatment in India. The schoolchildren dependent on armed forces personnel within the age group of 10–15 years of age forms the base of orthodontic treatment load in armed forces dental health setup. But no data is available on the prevalence of malocclusion and orthodontic treatment need in schoolchildren dependent on armed forces personnel. This study proposes to bring out the prevalence of malocclusion, the orthodontic treatment need and overall data regarding oral health in school going children.
This study was an effort to find out the prevalence of malocclusion and orthodontic treatment need scientifically using Index for Orthodontic Treatment Need (IOTN),8 a time tested index which is used internationally. As orthodontic care setup versus demand is not matching in armed forces dental care system, leads to long waiting periods to get the orthodontic treatment done. Frequent transfers of orthodontists and the armed forces personnel also add to the woes in this matter. This study shall help to formulate policies for the future in the training and placement of orthodontist for maximizing the benefits to the dependent clientele.
Aim of the present study was to ascertain the prevalence of malocclusion and orthodontic treatment need in schoolchildren dependent on armed forces personnel. The objective of the present study were
-
(i)
To estimate the prevalence of malocclusion
-
(ii)
To ascertain the orthodontic treatment need using Index for Orthodontic Treatment Need (IOTN)
-
(iii)
To review the overall oral health using DMFT index
-
(iv)
To evaluate any relation between increased DMFT index to existing orthodontic problems.
Material and methods
The study was conducted from Sep 2010 to Jan 2011. Five schools were randomly selected among all Army/KV/AF schools in Pune city and a random sample of 1200 children aged 10–15 years old attending these schools dependant on armed forces personnel were selected. Approval of ethical committee at Military Hospital was accorded for the project. School authorities and parents of sampled children were notified about purposes of the study.
The inclusion criteria employed for selection of samples were
-
(i)
Age group of 10–15 years
-
(ii)
Dependents of armed forces personnel
-
(iii)
No major local/systemic problems or trauma which affects the growth and development of facial structures or body
-
(iv)
No orthodontic or interceptive treatment carried out.
Any child not fulfilling the stated criteria was excluded from the study. The sampling frame comprised of approximate 2000 schoolchildren fulfilling the above criteria. Taking the prevalence of malocclusion as 50% (with alpha = 5% and chance error = 6%). The sample size worked out to be 235, i.e. say 240 in each school. Thus 240 children from each school were selected for the study giving a total sample size of 1200. The examinations were conducted at schools, by one set of orthodontists with the subject seated on a chair with adequate natural light and a total number of 20–25 children were examined per day. No radiographs were taken. Basic infection control procedures in Hand Hygiene and personal protective equipment (PPE) were adopted.9 The instruments and supplies were used were PMT sets, Cheek retractors, Enamel bowls, Kidney trays, Disposable mouth masks, Disposable gloves and Towels. PMT sets were used maximum twice and then discarded. Alcohol based antiseptic solution (3 M Hand Rub) was used for hand hygiene after washing with soap and water. After each days survey, all the reused instruments were chemically sterilized/autoclaved. Chemical sterilization was done with Unilon–SD (Cetrimide BP-15% w/v, Chlorhexidine Gluconate Soln-7.5% v/v, Isopropyl alcohol-8% v/v).
All survey forms was filled up after the examination of children by one orthodontist and need for orthodontic treatment is assessed using IOTN and overall oral health status by DMFT index and totaled.10 Other details like Angles Molar Classification,11 soft tissue condition, oral habits were recorded. To assess the attitude towards orthodontic treatment, awareness & motivation of patients were recorded. Questions like “Do you know about braces”, “where have you seen fixed type of braces”, “Have you seen braces among friends or in TV/Magazines/advertisements” were asked. Motivation was assessed by questions like “If you have to wear braces to correct your dental problem, will you agree for that”. Frontal intra oral photograph in centric occlusion were taken after applying cheek retractor with high-resolution digital camera. Immediately after the survey, health talk was given in Hindi/English and visual aids were also used in motivating children.
The DHC of the IOTN was graded in five categories for each patient. Patients were examined for Missing teeth, Overjet, Crossbites, Displacement of contact points and Overbites. The most severe occlusal trait was identified by the examiner for any particular patient and the patient was then categorized according to this most severe trait, with a score ranging therefore from 1 to 5. AC of the IOTN was assessed by second orthodontist, individual and a layperson. The soft copy of the photograph taken in digital camera were shown to individual at the time of examination and told to grade it, comparing the standard chart. A layperson, not associated with health profession was selected and told to compare the photographs with standard chart. To reduce the intra examiner bias, second orthodontist assessed the Esthetic Component of all the samples. The average of the three findings was taken as overall grade.
The data was transferred from pre-coded survey proforma to a computer. A master file was created for the purpose of data analysis. Statistical averages i.e. mean, standard deviation were employed to represent the different measurements. The inferential statistics assessing association amongst various variables were carried out using SPSS version 14. Appropriate statistical tests of significance were used wherever indicated. Prevalence of malocclusion was assessed by determining the percentage of children affected.
Results
Out of 1200, 705 (58.8%) were males and 495 (41.2%) were females with mean age of 12.70. 15.6% of the sample were dependents of Officers and 84.4% were the dependents of JCOs/ORs 36.6% had mixed dentition and 63.4% had permanent dentition. On analysis of oral hygiene, 38.8% had poor oral hygiene, 45.8% had fair oral hygiene and 15.4% had good oral hygiene. 75.2% showed Class I molar relation, 23% showed Class II molar relation and 1.8% showed Class III molar relation. 5.5% of the samples showed soft tissue abnormalities. On assessing awareness level, 78.8% were aware of orthodontic treatment and 21.2% were unaware about orthodontic treatment procedures. 7.2% of samples were motivated for orthodontic treatment, 51.3 were average on motivation and 41.5% had negative attitude about orthodontic treatment.
On analyzing DHC component of IOTN, 46.3% were Grade 1, 19.4% were Grade 2, 15.6% were Grade 3, 12.4% were Grade 4 and 6.2% were Grade 5 (Fig. 1). On excluding the Grade 1, it was observed that 53.7% samples had significant amount of deviation from the normal occlusion. On further analysis, it was found that 65.8% did not required treatment, 15.6% were borderline cases and 18.6% required definite treatment (Table 1). On analyzing five traits of DHC of IOTN, it was found that 9.5% of the sample showed missing teeth and 13.2% of the cases required orthodontic treatment. 25.1% showed increase in overjet than normal and 11.9% of the sample required treatment for correction of overjet. Crossbite tendencies were seen in 24.2% and 13.2% needed orthodontic treatment to correct crossbite. Displacement of the contact points was the largest variation seen from the normal occlusion among the all features. 49% of overall sample showed displacement of contact point and 29% required orthodontic treatment to correct it. 27.7% of the sample showed increase in overbite and 15.8% needed to correct this variation (Fig. 2). On analyzing AC of IOTN, 73.6% were grade 1–4 (No treatment required), 16.9% were graded 5–7 (Borderline) and 9.5% were graded 8–10 (Definite treatment) (Table 2). Thus combining DHC and AC of IOTN, it was concluded that 67.2% (466 males & 341 females) of sample not required orthodontic treatment and 32.8% (239 males & 154 females) of sample required orthodontic treatment (Fig. 3).
Fig. 1.
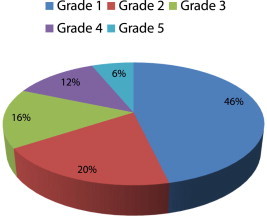
Grades of DHC.
Table 1.
Dental health component grades.
| DHC grade | Need for treatment | Male | Female | Total | % |
|---|---|---|---|---|---|
| Grade 1 & 2 | No treatment | 464 | 325 | 789 | 65.8% |
| Grade 3 | Borderline | 107 | 80 | 187 | 15.6% |
| Grade 4 & 5 | Definite treatment | 134 | 90 | 224 | 18.6% |
Chi-square = 8.767, p = 0.067.
Fig. 2.
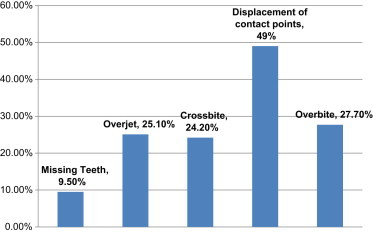
Malocclusion percentage in DHC.
Table 2.
Esthetic component grades.
| AC grade | Need for treatment | Male | Female | Total | % |
|---|---|---|---|---|---|
| Grade 1–4 | No treatment | 514 | 369 | 883 | 73.6% |
| Grade 5–7 | Borderline | 123 | 80 | 203 | 16.9% |
| Grade 8–10 | Definite treatment | 68 | 46 | 114 | 9.5% |
Chi-square = 0.428, p = 0.807.
Fig. 3.
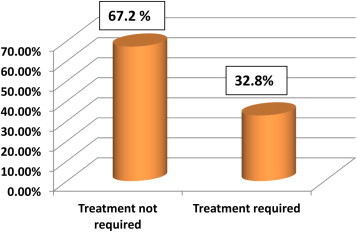
Need for orthodontic treatment.
On analyzing DMFT index, 55.1% of the sample showed no caries risk 38.1% showed moderate caries risk and 6.8% showed high caries risk. On comparing DMFT and need for orthodontic treatment it was found that moderate and high caries risk cases had significant increased requirement of orthodontic treatment (Table 3).
Table 3.
DMFT index and orthodontic treatment need comparison.
| DMFT Index | Need for orthodontic treatment |
Total | |
|---|---|---|---|
| No | Yes | ||
| No caries risk | 498 | 163 | 661 |
| Moderate caries risk | 269 | 189 | 458 |
| High caries risk | 40 | 41 | 81 |
Chi-square = 46.46, p = 0.00.
Discussion
The development of a uniform method of epidemiological assessment and grading of malocclusion has been of interest for several decades. An orthodontic index is a numerical scale that is derived by scoring specific features of a malocclusion to objectively assess some parameters such as how far a malocclusion varies from an ideal occlusion.12 Occlusal indices are useful for research, audit, practice management, and quality assurance in orthodontics.13 Over the years different occlusal indices have been employed to assess different facets of orthodontic service. However, not many of these indices have enjoyed international acceptance. In this study assessment of prevalence of malocclusion and orthodontic treatment need using IOTN, in schoolchildren dependent on armed forces personnel was carried out.
For any health setup which provides orthodontic care to dependents, data regarding the prevalence of malocclusion and need for orthodontic treatment is required. As the general awareness about esthetics is on high, demand for orthodontic treatment is on rise among the children dependent on armed forces personnel. The schoolchildren dependent on armed forces personnel within the age group of 10–15 years of age forms the base of orthodontic treatment load in armed forces dental health setup. But no data is available on the prevalence of malocclusion and orthodontic treatment need in schoolchildren dependent on armed forces personnel. One of the major hindrances to get uniform data related to prevalence of malocclusion in India is because of its variable ethnic groups. The prevalence of malocclusion among Indian children has been reported to be as low as 19.6% in Madras and high as 90% in Delhi (Table 4). As children of armed forces personnel consists of mixed population, no study done for a particular ethnic group can be attributed to them. IOTN developed by Brook & Shaw8 is widely used internationally as a method of objectively measuring the prevalence of malocclusion and treatment need in public dental health setup.14–17
Table 4.
Various studies in India for assessment of prevalence of malocclusion.
| Study by | Year | Sample age | Region | Prevalence % |
|---|---|---|---|---|
| Shourie | 1942 | 13–16 | Punjab | 50 |
| Shaikh | 1960 | 6–13 | Bombay | 68 |
| Miglani | 1963 | 15–25 | Madras | 19.6 |
| Shaik & Desai | 1966 | 07–21 | Bombay | 72.9 |
| Sidhu | 1968 | 6–30 | Delhi | 90 |
| Jacob | 1969 | 12–15 | Trivandrum | 44.97 |
| Prasad & Savadi | 1971 | 5–15 | Bangalore | 85.7 |
| Arya | 1976 | 5–28 | Nagpur | 96.5 |
| Nagraja Rao | 1980 | 5–15 | Udupi | 28.8 |
| Gardiner J H | 1989 | 10–12 | South Canara | 42 |
| Jalili | 1989 | 6–14 | Mandu district | 14.4 |
| Kharbanda | 1991 | 5–13 | Delhi | 10–18 |
| Dhar | 2007 | 8–14 | Udaipur | 30–40 |
| Shivkumar | 2009 | 12–15 | Davangere | 20 |
Dental health component are marked according to the grades given after clinical examination. The DHC has five categories classifying progressively increasing severity of malocclusions and indicating the relative need of orthodontic treatment (Grade 1: no treatment required, Grade 2: little need, Grade 3: borderline need, Grade 4: treatment required, Grade 5: great need of treatment). Within each category the different malocclusions are included (Missing teeth, Overjet, Crossbites, Displacement of contact points, Overbites, etc.) according to their severity. The most severe occlusal trait is identified by the examiner for any particular patient and the patient is then categorized according to this most severe trait, with a score ranging therefore from 1 to 5. In AC is assessed by comparing photographs for each sample with intra oral charts given by esthetic component in IOTN.
Malocclusion has a negative impact on the oral health related quality of life of adolescents. Children aged between 11 and 14 years old with malocclusion demonstrate significantly more “impacts” i.e. worse quality of life, compared with a minimal malocclusion group based on the IOTN.18 Adolescents who complete orthodontic treatment report fewer oral health impacts on their daily life activities than those who had never had treatment. Groups of children who need orthodontic treatment exhibit significantly higher impacts on their emotional and social well-being.19
Several studies have been published to describe the prevalence and types of malocclusions in different populations. Comparisons of these findings must be done cautiously, because different methods and indices were used in varying age and race of populations. On comparing distribution of rating for IOTN in school population to several studies like Brook & Shaw,8 Neslihan & Ertugay20 and Hosseinzadeh et al21 showed higher prevalence and high percentage of samples required need for orthodontic treatment than this study. The results of this study can be compared with the studies of Souames et al,22 N'agom et al,23 Dhar et al24 and Burden and Holmes.25 In present study higher DMFT significantly predicted orthodontic treatment need according to IOTN. Correlation between DMFT and orthodontic treatment need showed similar as in the study by Nobile et al.26
Comparing various studies of prevalence of malocclusion in India (Table 4), it was found that it is in not agreement with many studies which showed a rage of 14.4–96.5%. Most of the studies done were not used any internationally acceptable indices for the purpose of the study. The prevalence of 53.7% malocclusion is a significant deviation from the normal occlusion and 32.8% of the population requires orthodontic treatment. It was found that IOTN is a reliable and user-friendly index, which can be used for orthodontic surveys. Analyzing DMFT index, there was significant relation between higher DMFT index and orthodontic treatment need.
Intellectual contribution
Study concept: Col Prasanna Kumar, Brig SM Londhe.
Drafting & manuscript revision: Col Prasanna Kumar, Brig SM Londhe, Col Rajat Mitra.
Statistical analysis: Col Atul Kotwal, sm, Col Prasanna Kumar.
Study supervision: Col Prasanna Kumar, Brig SM Londhe, Col Atul Kotwal, sm, Col Rajat Mitra.
Conflicts of interest
This study has been funded by research grants from the O/o DGAFMS, New Delhi.
References
- 1.Kiyak H.A. Does orthodontic treatment affect patients' quality of life? J Dent Educ. 2008;72(8):886–894. [PubMed] [Google Scholar]
- 2.Shaw W.C. Factors influencing the desire for orthodontic treatment. Eur J Orthod. 1981;3:151–162. doi: 10.1093/ejo/3.3.151. [DOI] [PubMed] [Google Scholar]
- 3.Gray M.M., Bradnock G., Gray H.L. An analysis of the qualitative factors which influence young people's acceptance of orthodontic care. Prim Dent Care. 2000;7:157–161. doi: 10.1308/135576100322578924. [DOI] [PubMed] [Google Scholar]
- 4.N'gom P.I., Diagne F., Benoist H., Thiam F. Intraarch and interarch relationships of the anterior teeth and periodontal conditions. Angle Orthod. 2006;76:236–242. doi: 10.1043/0003-3219(2006)076[0236:IAIROT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.N'gom P.I., Diagne F., Aidara-Tamba A.W., Sene A. Relationship between orthodontic anomalies and masticatory function in adult subjects. Am J Orthod Dentofacial Orthop. 2007;131:216–222. doi: 10.1016/j.ajodo.2005.03.027. [DOI] [PubMed] [Google Scholar]
- 6.Shaw W.C., Addy M., Ray C. Dental and social effects of malocclusion and effectiveness of orthodontic treatment: a review. Community Dent Oral Epidemiol. 1980;8(1):36–45. doi: 10.1111/j.1600-0528.1980.tb01252.x. [DOI] [PubMed] [Google Scholar]
- 7.N'gom P.I., Brown R., Diagne F., Normand F., Richmond S. A cultural comparison of treatment need. Eur J Orthod. 2005;27:597–600. doi: 10.1093/ejo/cji030. [DOI] [PubMed] [Google Scholar]
- 8.Brook P.H., Shaw W.C. The development of an index of orthodontic treatment priority. Eur J Orthod. 1989;11:309–320. doi: 10.1093/oxfordjournals.ejo.a035999. [DOI] [PubMed] [Google Scholar]
- 9.Kohn W.G., Harte J.A., Malvitz D.M., Collins A.S., Cleveland J.L., Eklund K.J. Guidelines for infection control in dental health care settings—2003. J Am Dent Assoc. 2004;135(1):33–47. doi: 10.14219/jada.archive.2004.0019. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization Oral Health Surveys – Basic Methods. 4th ed. WHO; Geneva: 1997. [Google Scholar]
- 11.Angle E.H. Classification of malocclusion. Dental Cosmos. 1899;41:248–264. [Google Scholar]
- 12.Richmond S., Aylott N.A.S., Panahei M.E.S., Rolfe B., Harzer W., Tausche E. A 2-center comparison of orthodontists' perceptions of orthodontic treatment difficulty. Angle Orthod. 2001;71:404–410. doi: 10.1043/0003-3219(2001)071<0404:ACCOOP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 13.Daniels C., Richmond S. The development of the Index of Complexity, Outcome and Need (ICON) J Orthod. 2000;27:149–162. doi: 10.1093/ortho/27.2.149. [DOI] [PubMed] [Google Scholar]
- 14.Shaw W.C., Richmond S., O'Brien K.D. Indices of orthodontic treatment need and treatment standards. Br Dent J. 1991;170:107–112. doi: 10.1038/sj.bdj.4807429. [DOI] [PubMed] [Google Scholar]
- 15.Shaw W.C., O'Brien K.D., Richmond S., Brook P.H. Risk benefit appraisal in orthodontic. Br Dent J. 1991;170:33–37. doi: 10.1038/sj.bdj.4807399. [DOI] [PubMed] [Google Scholar]
- 16.Richmonds S. University of Manchester; 1990. A Critical Evaluation of Orthodontic Treatment in General Dental Service of England and Wales, PhD Thesis. [Google Scholar]
- 17.Richmond S., Shows W.C., O'Brien K.D., Buchanan I.B., Stephens C.D., Andrews M. The relationship between the index of orthodontic treatment need and consensus opinion of a panel of 74 dentists. Br Dent J. 1995;178:370–374. doi: 10.1038/sj.bdj.4808776. [DOI] [PubMed] [Google Scholar]
- 18.DeOliveira C.M., Sheiham A. The relationship between normative orthodontic treatment need and oral health-related quality of life. Community Dent Oral Epidemiol. 2003;31:426–436. doi: 10.1046/j.1600-0528.2003.00002.x. [DOI] [PubMed] [Google Scholar]
- 19.O'Brien C., Benson P.E., Marshman Z. Evaluation of a quality of life measure for children with malocclusion. J Orthod. 2007;34:185–193. doi: 10.1179/146531207225022185. [DOI] [PubMed] [Google Scholar]
- 20.Neslihan U., Ertugay E. The use of the Index of Orthodontic Treatment Need (IOTN) in a school population and referred population. J Orthod. 2001;28(1):45–52. doi: 10.1093/ortho/28.1.45. [DOI] [PubMed] [Google Scholar]
- 21.Hosseinzadeh N., Nourozi S., Fard M.J.K., Noroozi H. The relationship between patient, parent and orthodontic treatment need and demand in 17-year-old students residing in Abade/Iran. J Dent Tehran Univ Med Sci. 2007;4(3):107–114. [Google Scholar]
- 22.Souames M., Bassigny F., Zenati N., Riordan P.J., Boy-Lefevre M.L. Orthodontic treatment need in French schoolchildren: an epidemiological study using the index of orthodontic treatment need. Eur J Orthod. 2006;28:605–609. doi: 10.1093/ejo/cjl045. [DOI] [PubMed] [Google Scholar]
- 23.N'gom P.I., Diagnea F., Dieyeb F., Diop-Baa K., Thiamc F. Orthodontic treatment need and demand in Senegalese school children aged 12–13 years – an appraisal using IOTN and ICON. Angle Orthod. 2007;77(2):323–330. doi: 10.2319/0003-3219(2007)077[0323:OTNADI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Dhar V., Jain A., Van Dyke T.E., Kohli A. Prevalence of gingival diseases, malocclusion and fluorosis in school-going children of rural areas in Udaipur district. J Indian Soc Pedod Prev Dent. 2007;25:103–105. doi: 10.4103/0970-4388.33458. [DOI] [PubMed] [Google Scholar]
- 25.Burden D.J., Holmes A. The need for orthodontic treatment in child population of the United Kingdom. Eur J Orthod. 1994;16:395–399. doi: 10.1093/ejo/16.5.395. [DOI] [PubMed] [Google Scholar]
- 26.Nobile C.G.A., Pavia M., Fortunate L., Angelillo I.F. Prevalence and factors related to malocclusion and orthodontic treatment need in children and adolescents in Italy. Eur J Public Health. 2007;17(6):637–641. doi: 10.1093/eurpub/ckm016. [DOI] [PubMed] [Google Scholar]


