Abstract
Background
An outbreak of food poisoning was reported from a Military establishment on 29 May 2011 when 43 cases of food poisoning reported sick in a span of few hours.
Methods
A retrospective-prospective study was conducted. Data regarding the onset of symptoms, presenting features and history of food items consumed was collected. A detailed inspection of the mess for hygiene and sanitary status, cooking and storage procedure, and rodent nuisance was also carried out.
Results
A total of 53 cases of food poisoning occurred between 29 and 31 May 2011. All cases had symptoms of diarrohea followed by fever (96.2%), headache (84.9%), abdominal pain (50.1%), nausea and vomiting (49.1%) and bodyache (39.6%) respectively. Based on the Attributable Risk (AR = 46.67%) and Relative Risk (RR = 4.5, 95% CI = 1.22–16.54) Potato-bitter gourd vegetable served during dinner on 28 May 2011 was incriminated as the food item responsible for outbreak.
Conclusion
Symptomatology, incubation period and presence of rodent nuisance suggested contamination of Potato–bitter gourd vegetable with non-typhoidal Salmonella spp.
Keywords: Food poisoning, Non-typhoidal Salmonella spp, Military establishment
Introduction
Outbreaks of food poisoning commonly occur in closed communities where food is prepared and served centrally for a sizable population like student's hostels, old age homes, prisons, hospitals and nursing homes. In Armed Forces also, due to community kitchen practice, a number of outbreaks involving varying number of personnel are reported every year.1 Besides, being a cause of concern for Unit Commanders and an added burden on health care facilities, the outbreak points to the existence of conditions which led to such an event. Hence, investigation of such an outbreak is not just a matter of elucidating the cause, but also of establishing why the causal circumstances arose.2
The authors investigated an outbreak of food poisoning which was reported from a Military establishment. On 29 May 2011, 43 cases (out of total 53 cases) reported to the Emergency Department (ED) with complaints of loose motions, fever, headache, vomiting and abdominal pain. All cases were treated at ED and one case was referred to hospital.
Material and methods
A retrospective–prospective study design was used for investigation of the outbreak.3 A probable case of food poisoning was defined as a previously well individual who suddenly developed any two of the following symptoms after eating dinner on 28 May 2011: diarrhoea (three or more loose stools in 24 h or less), fever, abdominal pain, nausea or vomiting. An epidemiological case sheet was developed for collecting the information on demographic particulars of individuals, date and time of onset of illness and time of reporting, food items eaten, presenting symptoms, and history of consumption of water or food outside the mess. A line listing of all these individuals was also done.
All cases that occurred on 29 May 2011 were traced and relevant details were obtained. Search was also made for those who had taken dinner in the mess but had not fallen ill. All such individuals were also interviewed and data on the epidemiological case sheet was recorded. All cases were followed up till recovery. Some respondents who were not available on the day of the investigation or who could not recall accurate food history were excluded from the analysis. Attack rate and Relative Risk (RR) with 95% confidence interval (95% CI) were calculated for each food item to establish an association with the illness.
An environmental survey was undertaken to assess the hygiene and sanitation of the cook house. Details of food processing, food preparation and storage of prepared food pending consumption were ascertained by interviewing food handlers. Medical examination of food handlers was carried out and stool specimens were collected for bacteriological examinations.
Stool samples were also collected from 8 patients and sent for culture. Food sample of all items of dinner on 28 May 2011, which was preserved in the mess, was also sent for culture. Water samples from three different points of water consumption were collected and analyzed for residual chlorine and bacteriological examination.
Results
Of the total 118 persons reported having dinner in the mess on 28 May 2011, 53 met the definition of food poisoning. The index case had the onset of symptoms within 6 h and reported sick in the early hours of 29 may 2011. This was followed by sudden rise in the number of cases and by midday 50% of the cases had reported. The last case was noted at 0200 h on 30 May 2011, suggesting the maximum incubation period to be approx 31 h. The sharp rise and fall of the epidemic curve, as shown in Fig. 1, confirms that the present outbreak was a point source outbreak.
Fig. 1.
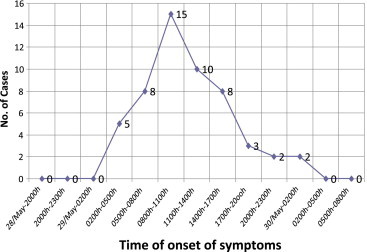
Epidemic curve.
As can be seen from Fig. 2, diarrhoea was the commonest symptom and was present in all 53 (100%) cases. Fever was of high grade, not associated with chills and rigours and was present in 51 (96.2%) cases. Headache was present in 45 (84.9%) cases, nausea and vomiting in 26 (49.1%), abdominal pain in 27 (50.1%) and body ache in 21 (39.6%) cases. There was no history of blood in stool or in vomitus.
Fig. 2.
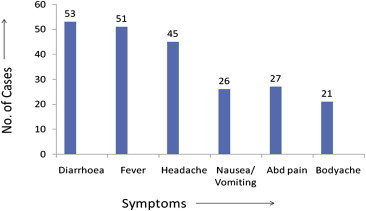
Symptom-wise distribution of cases.
The food items served during dinner on 28 May 2011 and food specific Attributable Risk (AR) and Relative Risk (RR) are shown in Table 1. The maximum Attributable Risk was noted for potato–bitter gourd vegetable, followed by rice. Relative Risk of 4.5 for potato–bitter gourd vegetable indicated that individuals who consumed potato–bitter gourd vegetable were 4.5 times more likely to have food poisoning than those who did not consume it. The probability of obtaining an RR of 4.5 or even higher was found to be 1/1250 (p = 0.0008) which is far less compared to 1/500 (p = 0.002) for rice (RR = 2.31). This is unlikely to have occurred by chance alone.
Table 1.
Food specific attack rates and relative risks of items served at dinner on 28 May 2011.
| Food items | Ate food item |
Did not eat food item |
AR (%) | RR (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Ill | Not ill | Attack rate (%) | Total | Ill | Not ill | Attack rate (%) | |||
| Rice | 74 | 46 | 28 | 62.12 | 26 | 7 | 19 | 26.92 | 35.20 | 2.31a (1.2–4.5) |
| Chapati | 86 | 46 | 40 | 53.49 | 14 | 6 | 8 | 42.86 | 10.63 | 1.25 (0.66–2.36) |
| Dal | 75 | 41 | 34 | 54.67 | 25 | 12 | 13 | 52.00 | 2.67 | 1.14 (0.72–1.80) |
| Cabbage–capsicum | 59 | 32 | 27 | 54.23 | 41 | 19 | 22 | 46.34 | 7.89 | 1.17 (0.78–1.75) |
| Potato bitter Gourd | 85 | 51 | 34 | 60.00 | 15 | 2 | 13 | 13.33 | 46.67 | 4.5b (1.22–16.54) |
| Mutton | 8 | 6 | 2 | 75 | 92 | 47 | 45 | 51.08 | 23.92 | 1.47 (0.94–2.30) |
| Milk | 32 | 22 | 10 | 68.75 | 68 | 31 | 37 | 45.56 | 23.19 | 1.51 (1.06–2.14) |
(Note: AR–Attributable Risk; RR–Relative Risk; CI–confidence interval).
X2 = 9.59 df = 1 p = 0.002.
X2 = 11.15 df = 1 p = 0.0008.
Environmental survey showed presence of rodent nuisance in the ration store and cookhouse. Dry ration stored in gunny bags were kept open, permitting contamination by faeces and urine of rodents. Investigation into food processing revealed that the raw ingredients were procured from the authorised government agencies. These items were cooked in the mess and preparation was completed by 1600 h. The cooked food was covered and kept on the platform to be served between 1900 h and 2100 h. However, there was no monitoring after the dinner was started. The individuals kept coming and serving food themselves till 2200 h. No leftover food from the previous meal was used during preparation of dinner.
All stool cultures showed growth of Escherichia coli. Samples of potato–bittergourd vegetable and cabbage–capsicum vegetable showed growth of Klebsiella spp. Milk showed growth of Serratia spp. Rice showed growth of Acinetobacter spp. Other food items did not show any growth. There was no evidence of Salmonella, Shigella or Staphylococcus. All three water samples did not grow any coliform organism.
Discussion
In the present outbreak of food poisoning, dinner served on 28 May 2011 was the common meal responsible. Potato–bitter gourd vegetable was the incriminating food item on the basis of highest statistically significant Relative Risk (RR) for this item.
Clinico-epidemiological picture of the outbreak gives a clue to its aetiology. Diarrhoea with or without abdominal cramps is a presenting feature of food poisoning due to Salmonella spp, Campylobacter jejuni, Clostridium perfringens, and diarrhoeal form of Bacillus cereus. But fever, seen in 96.2% of cases in the present outbreak, is characteristically seen only in Salmonella food poisoning.
In the present study, all cases occurred within 6–31 h with a median incubation period of 15 h. Such incubation period is seen in food poisonings due to Salmonella spp, Clostridia spp and some cases of B. cereus. Clostridia spp food poisoning commonly occurs following consumption of food which was prepared 24 h or more before consumption and presents with diarrhoea but no fever. Diarrhoeal form of B. cereus has a minimum incubation period of 12 h and do not have fever. Hence Clostridia and B. cereus are unlikely cause of the present outbreak.
With the given clinical picture and the incubation period, notwithstanding the culture reports, the possible cause of food poisoning appears to be Salmonella spp. The incriminating food item, though not typical of Salmonella food poisoning, appears to be potato–bitter gourd vegetable. In view of the unsatisfactory storage of food items and rodent nuisance in the mess, and food laid out at room temp for long time, there is a possibility of contamination of potato–bitter gourd vegetable. However, the source of contamination cannot be pinpointed.
Food poisoning has been defined as an acute gastroenteritis caused by ingestion of food or drink contaminated with either living bacteria or their toxins or inorganic chemical substances and poisons derived from plants and animals.4 Food poisoning outbreaks among humans caused by Salmonella spp are due to Salmonella typhimurium, Salmonella choleraesuis, Salmonella enteritidis and many other similar species.4 Incubation period ranges from 6 to 48 h and common presenting symptoms include fever, headache, nausea, vomiting, abdominal pain and diarrhoea. Reservoir/source of infection include poultry, rats, pigs, cattle, pets and human patients and convalescent carriers. Main route of transmission is by ingestion of the organisms in food (milk, poultry, meat, eggs) derived from infected food animals. Food can also be contaminated by infected food handlers, by cross contamination as a result of poor hygiene and from faeces of an infected animal or a person,5
Food poisonings due to Salmonella spp are usually sporadic and, in a great majority of cases, there is no identifiable link to other cases.6 The mode of transmission also may not be evident in many situations.7 In a study, conducted in New Zealand between 2000 and 2009, 204 outbreaks of non-typhoidal salmonellosis were analyzed. The results showed that non-typhoidal salmonellosis was primarily a food borne disease in New Zealand, but there was insufficient evidence to confirm important food vehicle. Evidence for the mode of transmission was weak or absent for 107 (63%) of the 169 outbreaks for which a mode of transmission was reported.8 Unusual sources like peanut butter and watermelon have also been associated with non-typhoidal salmonellosis.9,10 Pet rodents, probably, are an under-recognized source of human Salmonella infection.11
Intellectual contributions of authors
Study concept: Col Rajesh Kunwar.
Drafting and manuscript: Col Rajesh Kunwar, Maj Harpreet Singh, Maj Vipra Mangla, Maj R Hiremath.
Statistical analysis: Col Rajesh Kunwar.
Study supervision: Col Rajesh Kunwar.
Conflicts of interest
All authors have none to declare.
References
- 1.Directorate General Armed Forces Medical services . vol. 2. 2003. Food poisoning; pp. 640–647. (Manual of Health for the Armed Forces). New Delhi. [Google Scholar]
- 2.Hadden F., O'Brien S. Managing a communicable disease outbreak. In: Pencheon D., Guest C., Melzer D., Gray J.A.M., editors. Oxford Handbook of Public Health Practice. Oxford University Press; New York: 2005. pp. 244–251. [Google Scholar]
- 3.Kelsey J.L., Thompson W.D., Evans A.S. vol. 10. Oxford University Press; New York: 1986. Methods in Observational Epidemiology; pp. 212–253. (Monographs in Epidemiology and Biostatistics). [Google Scholar]
- 4.Park K. Park's Textbook of Preventive and Social Medicine. 21st ed. M/S Banarsidas Bhanot; Jabalpur: 2011. Food poisoning; pp. 216–218. [Google Scholar]
- 5.WHO . World Health Organization; Geneva: 2008. Foodborne Disease Outbreaks: Guidelines for Investigation and Control. [Google Scholar]
- 6.Painter JA, Perch M, Voetsch AC. Nontyphoidal salmonellosis. In: Wallace RB, ed. Wallace/ Maxcy – Rosenau – Last Public Health & Preventive Medicine. 15th ed. New York: The Mc Graw Hill Companies; 2008:437–440.
- 7.Jadhav S.L., Sinha A.K., Banerjee A., Chawla P.S. An outbreak of food poisoning in a military establishment. MJAFI. 2007;63(2):130–133. doi: 10.1016/S0377-1237(07)80055-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.King N., Lake R., Campbell D. Source attribution of nontyphoid salmonellosis in New Zealand using outbreak surveillance data. J Food Prot. 2011;74(3):438–445. doi: 10.4315/0362-028X.JFP-10-323. [DOI] [PubMed] [Google Scholar]
- 9.Salmonellosis outbreak caused by peanut butter. Available on: http://www.promedmail.org. Accessed on 10. 07. 11.
- 10.McCallum L., Torok M., Dufour M.T., Hall A., Cramp G. An outbreak of Salmonella typhimurium phage type 1 associated with watermelon in Gisborne, January 2009. N Z Med J. 2010, Sep 10;123(1322):39–45. [PubMed] [Google Scholar]
- 11.Swanson Stephen J., Snider Cynthia, Braden Christopher R. Multidrug-resistant Salmonella enterica Serotype typhimurium associated with pet rodents. N Eng J Med. 2007;356:21–28. doi: 10.1056/NEJMoa060465. [DOI] [PubMed] [Google Scholar]


