Abstract
Every year > 600,000 sports and recreation related eye injuries occur, out of which roughly 13,500 of these result in permanent loss of sight. Up to 90% of these sports related eye injuries are preventable by using adequate eye protection equipment. Protective eyewear is made of polycarbonate, a highly impact-resistant plastic which is now easily available as prescription and non-prescription eyewear and all players should be encouraged to use them. The medical officers by educating their patients regarding the risks of eye injuries in various sports and the confirmed benefits of using protective equipment have the potential to prevent injury to over thousands of eyes every year. The medical fraternity can also play a very important role in educating the coaches, parents, and children and thus put an end to unnecessary blindness and vision loss from sports related ocular injuries, therefore ensuring a lifetime of healthy vision.
Keywords: Ocular trauma, Protective eyewear, Sports
Introduction
Every year > 600,000 sports and recreation related eye injuries occur.1 About 42,000 of these are of a severity that requires emergency room attention,2,3 with roughly 13,500 of these resulting in permanent loss of sight. Emergency rooms in the US treat a sports related ocular injury every 13 minutes. Playing games are responsible for anywhere between 10% and 20% of all ocular injuries. The incidence of ocular injuries in sports is far more commonly seen in children.3-6 In our country though no study has been carried out to assess the incidence of sports related ocular injuries, however, the available literature reveals a similar picture where playing sports was responsible for nearly 37-52% of ocular injuries mainly affecting young children in 58-70% of cases,7,8 These injuries are also seen commonly in the military personnel as games are an integral part of their daily routines. In fact playing outdoor games are highly encouraged in the forces. Football, basketball, cricket, boxing, racquet sports, and full contact martial arts, all very popular in the services, are games most commonly associated with ocular injuries. Playing with bow and arrow and gulli- danda are a unique and common cause of ocular injuries in our country (Fig. 1).8,9 The fact remains that up to 90% of these sports related eye injuries are preventable.1,10 The medical officers by educating their patients regarding the risks of eye injuries in various sports and the confirmed benefits of using protective equipment, have the potential to prevent injury to >1000 of eyes every year. They should also be able to differentiate the minor eye injuries from the major ones which require immediate referral to an ophthalmologist (Table 1). The medical fraternity also have a very important role to play in educating the coaches, parents, and children and thus put an end to unnecessary blindness and vision loss from sports related ocular injuries, ensuring a lifetime of healthy vision.1,11
Fig. 1.

Traumatic cataract—post ‘gullidanda’ injury.
Table 1.
Signs and symptoms requiring immediate ophthalmic referral.10
| 1. | Sudden decrease in or loss of vision |
| 2. | Loss of field of vision |
| 3. | Pain on movement of the eye |
| 4. | Photophobia |
| 5. | Diplopia |
| 6. | Proptosis of the eye |
| 7. | Light flashes or floaters |
| 8. | Irregularly shaped pupil |
| 9. | Foreign-body sensation/embedded foreign body |
| 10. | Hyphaema (blood in anterior chamber) |
| 11. | Halos around lights |
| 12. | Laceration of the lid margin or near medial canthus |
| 13. | Broken contact lens or shattered eyeglasses |
| 14. | Suspected globe perforations |
Most common mechanisms of eye injuries
The most common mechanisms of eye trauma involve closed globe, open globe, and radiation injuries.3 Closed globe injuries account for most sports related eye injuries. The anterior segment is the portion of the eye most frequently damaged by blunt trauma, and hyphaema is the most common mode of clinical presentation (Fig. 2).12 The extent of ocular damage depends on the size, hardness, and velocity of the blunt object, and the force imparted directly to the eye. A direct blow to the globe from a blunt object smaller than the eye’s orbital opening causes rapid anteroposterior compression and dilation of the middle of the globe, transmitting a great force to the internal ocular structures. A blunt object larger than the orbital opening (> 5 cm in diameter) exerts force on the floor of the orbit or the medial wall, resulting in fractures of the thin bones. This ‘pressure-release valve’ may prevent rupture of the globe; however, there is a high incidence of occult internal ocular in- juries.10 Another condition which may occur in cases of blunt trauma especially to the forehead is traumatic optic neuropathy (TON) which refers to an acute injury of the optic nerve secondary to trauma. The optic nerve may be damaged either directly or indirectly. An indirect injury to the optic nerve typically occurs from the transmission of forces to the optic canal from blunt head trauma. In contrast to direct TON, which results from an anatomical disruption of the optic nerve fibres from penetrating orbital trauma, bone fragments within the optic canal, or nerve sheath hematomas. Patients usually present with a variable degree of vision loss (decreased visual acuity, visual field abnormalities, or loss of colour vision). However, most cases (up to 60%) present with severe vision loss of light perception (LP) or worse. In the acute phase, the optic nerve usually appears normal on funduscopic examination, but optic nerve atrophy is often seen 3-6 weeks after the injury.
Fig. 2.

Traumatic hyphaema due to a tennis ball injury.
Examples of blunt injuries include orbital blowout fracture, orbital and lid contusions, iris injury, traumatic iritis, subconjunctival haemorrhage hyphaema, retinal haemorrhage, commotio retinae, vitreous haemorrhage, choroidal rupture, retinal tears, and retinal detachment.
Open globe injuries are relatively uncommon. Such injuries range from mild abrasions to serious lacerations. Though sometimes the diagnosis is straight forward with uveal tissue prolapsing out of an anterior scleral or corneal wound or, an identifiable foreign body in the eye; however, globe rupture is more often occult on presentation and the examination of the injured eye should proceed systematically to identify as well as protect a ruptured globe (Table 2). It is necessary to avoid putting pressure on a ruptured globe to prevent any extrusion of intraocular contents and to avoid a further damage. In any case of obvious or suspected ruptured globe rupture it very important to transfer the patient immediately to the nearest eye centre. The following first aid steps at the primary care level will go a long way in saving the patient’s eye:
-
1.
The ruptured globe should be protected from any pressure or inadvertent contact with a rigid shield during transport.
-
2.
Impaled foreign bodies should be left undisturbed.
-
3.
Eye patches are contraindicated. Instead a Fox eye shield or any other rigid device (bottom of a polystyrene foam cup) should be placed over the affected eye.
-
4.
Avoid any eye manipulation that may increase intraocular pressure with potential extrusion of intraocular contents.
-
5.
Administer antiemetics to prevent Valsalva maneuvers.
-
6.
Administer sedation and analgesics as needed.
-
7.
Avoid any topical eye solutions (e.g. fluorescein, ligno- caine, cycloplegics).
-
8.
The frequency of endophthalmitis after open globe injury has been estimated to be about 6.8%.13 Administer prophylactic broad spectrum topical antibiotics to prevent endophthalmitis.
-
9.
Administer tetanus prophylaxis.
-
10.
Ensure the patient is kept nil orally (NPO).
Table 2.
Evaluation of a case of suspected globe rupture.
| Visual acuity | Assessed in both the injured as well as the normal eye |
| Ocular movements | To rule out entrapment from an associated orbital floor fracture |
| Orbits | Orbits should be examined for bony deformity, foreign body, and globe displacement
|
| Eyelids | Eyelid and lacrimal injuries evaluated for possible deep injuries to the globe Even small lid lacerations may conceal vision-threatening globe perforations |
| Conjunctiva | Conjunctival lacerations may overlie more serious scleral injuries Severe conjunctival haemorrhage may indicate globe rupture |
| Cornea/sclera | Prolapse of the iris through a full-thickness corneal laceration may be visible Scleral buckling is indicative of rupture with extrusion of ocular contents Intraocular pressure will likely be low, but measurement is contraindicated More subtle or partially self-sealing corneal wounds may show a positive Seidel test |
| Pupils | Examined for shape, size, light reflex, and relative afferent pupillary defect (RAPD) A peaked, teardrop-shaped, or otherwise irregular pupil may indicate globe rupture |
| Anterior chamber | Slit lamp examination may reveal corneal lacerations; iris prolapse; hyphaema from ciliary body disruption; and lens injuries, including dislocation or subluxation A shallow anterior chamber may be the only sign of occult globe rupture |
| Other findings | Vitreous haemorrhage after trauma suggests retinal or choroidal tear, optic nerve avulsion, or foreign body Retinal tears, oedema, detachments, and haemorrhage may accompany globe rupture |
Canalicular lacerations usually occur because of trauma from a fellow player’s finger in the area of the medial canthus. Fishing hooks too have been known to cause penetrating globe injuries.
Radiation injuries occur as a result of exposure to ultraviolet light in snow skiing, water skiing, and other water sports.
Protective devices
Sports can be broadly classified as collision (football, rugby, hockey), contact (baseball, football, basketball, wrestling),non-contact (cross-country running, tennis, swimming), and other (bowling, golf, archery, field events). Considering the potential for eye injury, sports are further categorised as low, high, and very high-risk sports12 (Table 3). Eye protection has reduced the number and severity of eye injuries and it is strongly recommended that protective eyewear be worn by all participants in sports in which there is risk of eye injury. Sports participants using ‘street wear’ (corrective eyewear or sun wear) are at a far more severe risk of eye injury than those using no eye protection at all. Contact lenses offer absolutely no protection and a hard or gas permeable contact lens may even break upon impact causing a corneal abrasion or corneal laceration with rupture of the eye. Similarly eyeglasses offer inadequate protection and may also damage the eye by its shattering impact. Eye safety goggles specially designed for these sports should be worn while participating. There is more energy in a squash ball than a 0.22 calibre bullet because of the weight of the squash ball. A hockey puck travels at 90-100 mph. A badminton shuttlecock has been clocked at 180 mph. An effective protective device dissipates the harmful force over a larger area i.e., shifts the impact from the eyes and face to the skull without causing intracranial injury. Protective eyewear is often made of polycarbonate, a highly impact-resistant plastic, eight times stronger than other materials and even capable of absorbing ultraviolet light. Regular eyeglasses have only 4-5% of the impact resistance of polycarbonate of comparable thick- ness.10 Polycarbonate is now easily available as prescription and non-prescription eyewear for squash and badminton players, and all players should wear polycarbonate closed protectors. The American Society for Testing and Materials (ASTM) has established performance standards for selected eyewear in racquet sports, baseball, basketball, women’s lacrosse, field hockey, and skiing. It has also been ensured that these devices are acceptable to the athlete, does not change the appeal of the game, and also does not generate unacceptable liability (Table 4).10
Table 3.
Classification of sports eye-injury risk to the unprotected player.2
| High-risk | Moderate-risk | Low-risk | Eye rafe | ||
|---|---|---|---|---|---|
| Small, fast projectiles | Hard projectiles | Intentional injury, | Badminton | Swimming | Track and field |
| Air rifle, Paintball | Sticks, close contact | Boxing | Tennis | Diving | Gymnastics |
| Squash | Full-contact martial arts | Volleyball | Skiing (snow and | ||
| Cricket | Water polo | water) | |||
| Baseball, | Football | Wrestling | |||
| Lacrosse, | Fishing Golf | Bicycling | |||
| Hockey | |||||
| Racquetball | |||||
Table 4.
Recommended eye protectors for selected sports.12
| Sport | Protective eye wear |
|---|---|
|
Sports goggles with polycarbonate lenses |
|
Polycarbonate or wire face guards on the batter’s helmet and sports goggles with polycarbonate lenses on the field |
|
A full face mask for the goalie and sports goggles with polycarbonate lenses on the field |
|
A polycarbonate eye shield attached to wire face mask |
|
Helmet with full-face protection |
|
Full-face protection or sports goggles with polycarbonate lenses or wire mesh |
|
Full-face protection |
|
Sports goggles with polycarbonate lenses |
|
High-impact resistant eye protection or sports goggles with polycarbonate lenses They should also filter ultraviolet and excessive sunlight |
| Myths: Misconceived excuses for not using eye guards |
|---|
|
|
|
|
Conclusion
The incidence of ocular injuries in sports is rising and is a matter of great concern in the US, 30% of ocular injuries among children < 16 years of age are sports related.14 So much so that to educate the public on this, Prevent Blindness America—the nation’s oldest volunteer eye health and safety organisation— has made September ‘sports eye health and safety awareness’ month. Protective eyewear should be mandatory for athletes who are functionally one-eyed and for athletes who have already undergone eye surgery or suffered ocular trauma.12,14 These individuals should not participate in sports in which adequate eye protection is not available. A pre-participation eye examination is helpful in identifying persons who may be at increased risk for eye injury. Injuries are not related to the age or experience of the players and unless steps are taken, in terms of either mandatory use of eye-protectors and/or of educating the general public on the possible devastating effects of injury, these preventable injuries will continue to burden the already overworked hospital casualty departments, draining both resources and expertise.
We also recommend a national sports registry for eye injuries be maintained as a database of these injuries, similar to the one maintained in America. For this we suggest the following performa which is similar to the American eye injury registry with some suitable modifications (Appendix A and B).
Conflicts of interest
None identified.
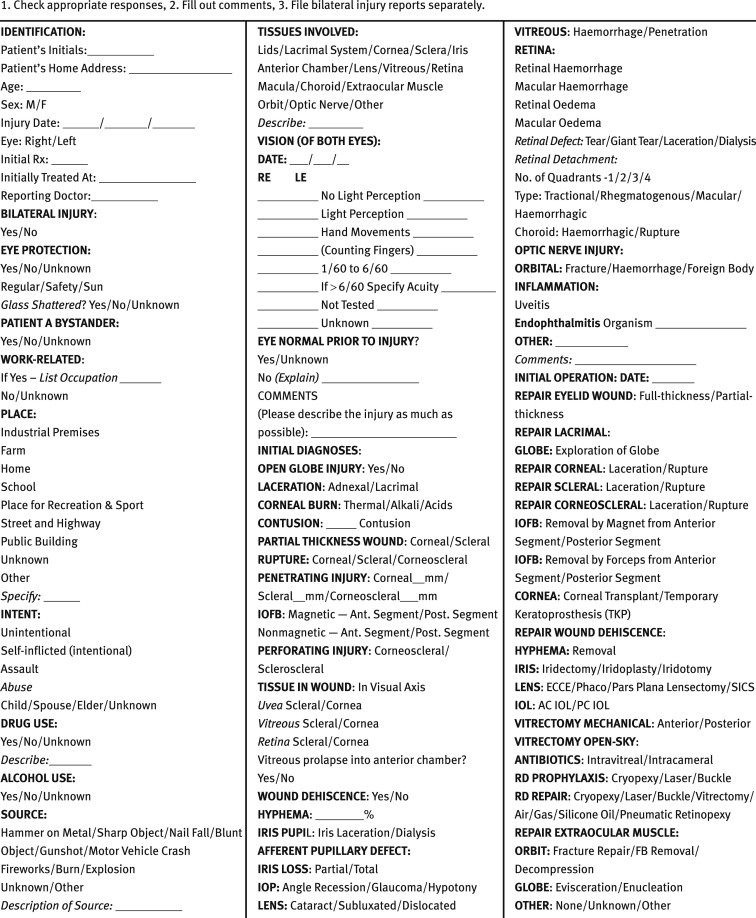
Appendix A.
Indian injury registry initial report.
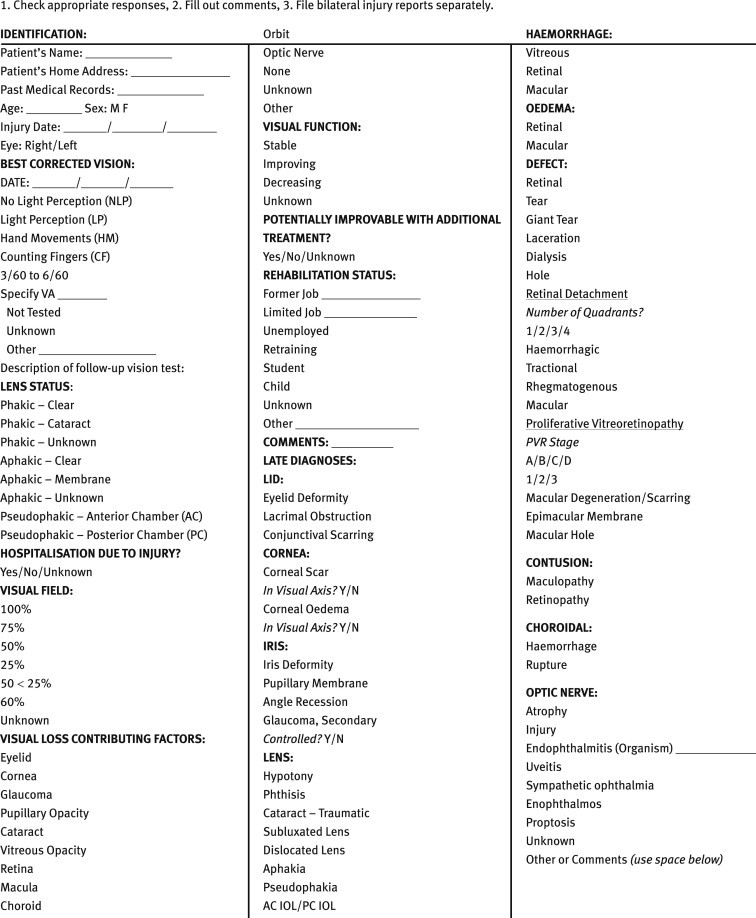
Appendix B.
Indian eye injury registry six-month follow-up report.
References
- 1.Goldstein, Michael H., Daniel W. Sports injuries: an ounce of prevention and a pound of cure. Eye & Contact Lens: Sci Clin Prac. 2011;37:160–163. doi: 10.1097/ICL.0b013e31821790db. [DOI] [PubMed] [Google Scholar]
- 2.Vinger P.F. A practical guide for sports eye protection. Phys Sportsmed. 2000;28:49–69. doi: 10.3810/psm.2000.06.961. [DOI] [PubMed] [Google Scholar]
- 3.Rodriguez J.O., Lavina A.M., Agarwal A. Prevention and treatment of common eye injuries in sports. Am Fam Physician. 2003;67:1481–1488. [PubMed] [Google Scholar]
- 4.Shoja M.R., Miratashi A.M. Pediatric ocular trauma. Acta Medica Iranica. 2006;44:125–130. [Google Scholar]
- 5.MacEwen C.J., Baines P.S., Desai P. Eye injuries in children: the current picture. Br J Ophthalmol. 1999;83:933–936. doi: 10.1136/bjo.83.8.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaur A., Agrawal A. Paediatric ocular trauma. Current Science. 2005;89:43–46. [Google Scholar]
- 7.Jaison S.G., Silas S.E., Daniel R., Chopra S.K. A review of childhood admission with perforating ocular injuries in a hospital in north-west India. Indian J Ophthalmol. 1994;42:199–201. [PubMed] [Google Scholar]
- 8.Narang S., Gupta V., Simalandhi P., Gupta A., Raj S., Dogra M.R. Paediatric open globe injuries. Visual outcome and risk factors for endophthalmitis. Indian J Ophthalmol. 2004;52:29–34. [PubMed] [Google Scholar]
- 9.Singh D.V., Sharma Y.R., Azad Rajvardhan, Talwar D., Rajpal Profile of ocular trauma at Tertiary Eye Centre. JK Sciences. 2005;7:16–21. [Google Scholar]
- 10.Vinger P.F., Duma S.M., Crandall J. Baseball hardness as a risk factor for eye injuries. Arch Ophthalmol. 1999;117:354–358. doi: 10.1001/archopht.117.3.354. [DOI] [PubMed] [Google Scholar]
- 11.Barr A., Baines P.S., Desai P., MacEwen C.J. Ocular sports injuries: the current picture. Br J Sports Med. 2000;34:456–458. doi: 10.1136/bjsm.34.6.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Academy of Pediatrics Committee on Sports Medicine and Fitness; American Academy of Ophthalmology, Eye Health and Public Information Task Force. Protective eyewear for young athletes. Ophthalmology. 2004;111:600–603. [Google Scholar]
- 13.Essex R.W., Yi Q., Charles P.G., Allen P.J. Post-traumatic endophthalmitis. Ophthalmology. 2004;111:2015–2022. doi: 10.1016/j.ophtha.2003.09.041. [DOI] [PubMed] [Google Scholar]
- 14.Youn J., Sallis R.E., Smith G., Jones K. Ocular injury rates in college sports. Med Sci Sports Exerc. 2008;40:428–432. doi: 10.1249/MSS.0b013e31815e7263. [DOI] [PubMed] [Google Scholar]


