Abstract
Background
Norman's procedure is a well known surgical technique for the hypermobility of temporomandibular joint. In this procedure after performing glenotemporal osteotomy the augmentation of the zygomatic root of the temporal bone is done by placing a bone graft from the iliac crest to prevent forward movement of the condyle beyond the eminence. This paper describes the clinical outcome of two modifications added to Norman's procedure. In addition to the conventional procedure inferiorly based pedicled flap from the temporal fascia was sutured to the antero-lateral aspect of the capsule. Intraorally pterygoid disjunction was carried out only in those case in which hypermobility was associated with painful temporomandibular joint disorder.
Methods
Modified Norman’s procedure was performed in 10 patients (4 females & 6 males), 7 of them were bilateral and 3 cases were unilateral under general anesthesia.
Results
After one year follow up in none of the cases graft failed or rejected though recurrence along with TMJ pain was noticed in 2 cases.
Conclusion
This technique is versatile but long-term follow up on a larger number of patients is necessary to be able to draw definitive conclusions.
Keywords: Norman's procedure, Subluxation, Dislocation, Temporofascial flap, Pterygoid disjunction
Introduction
Chronic subluxation of the temporomandibular joint (TMJ) is defined as an excessive abnormal excursion of the condyle where the condylar head moves anterior to the eminence on wide opening, while the mouth can be closed again without any assistance. Acute subluxation is associated with pain due to internal derangement of TMJ. Radiographically, the condyle is found translating anterior to articular eminence. Acute dislocation of the TMJ is a condition where the condyle moves suddenly anterior to the articular eminence and gets locked. Chronic recurrent dislocation is characterized by a condyle that slides over the articular eminence catches briefly beyond the eminence and then returns to the fossa. Most patients find that they can reduce their condyle to the normal position. Acute mandibular dislocation is a displacement of the condyle anterior to the articular eminence with complete separation of the articulating surfaces and fixation in that position. The etiology of hypermobility is unclear. The pathogenesis of hypermobility is secondary to weakness or laxity of the capsule. Patients often complain of difficulty in mastication. Management of hypermobility remains a challenge, despite a large number of conservative and surgical techniques with variable results described in literature.1,2 This paper describes the clinical outcome of two modifications added to Norman’s procedure.3,4 In addition to the conventional procedure inferiorly based pedicled flap from the temporal fascia was sutured to the antero-lateral aspect of the capsule. Intraorally pterygoid disjunction was carried out only in those case in which hypermobility was associated with painful temporomandibular joint disorder.5
Materials and method (Table 1)
Table 1.
Results following surgery.
| S.No. | Gender | Age | Side | Diagnosis | Associated TMJ pain | Preop mouth opening | Pterygoid disjunction | Mouth opening at 1 year post surgery | Transient facial nerve palsy | Follow up | Recurrence | TMJ pain post surgery |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | M | 32 | R & L | Chronic Subluxation | Yes | 49 | Yes | 40 | No | 1 year | Yes | Yes |
| 2. | M | 28 | R | Recurrent dislocation | Yes | 48 | Yes | 38 | No | 1 year | No | No |
| 3. | F | 28 | R | Recurrent dislocation | Yes | 42 | Yes | 38 | No | 1 year | Yes | Yes |
| 4. | M | 38 | R & L | Chronic Subluxation | No | 49 | No | 40 | No | 1 year | No | No |
| 5. | M | 42 | R & L | Chronic Subluxation | Yes | 44 | Yes | 39 | No | 1 year | No | No |
| 6. | M | 40 | R & L | Chronic Subluxation | Yes | 46 | Yes | 36 | Yes | 1 year | No | No |
| 7. | M | 39 | R & L | Chronic Subluxation | Yes | 48 | Yes | 38 | No | 1 year | No | No |
| 8. | F | 54 | R & L | Chronic Subluxation | No | 52 | No | 38 | No | 1 year | No | No |
| 9. | F | 48 | L | Chronic Subluxation | Yes | 48 | Yes | 38 | No | 1 year | No | No |
| 10. | F | 50 | R & L | Recurrent dislocation | No | 49 | No | 37 | No | 1 year | No | No |
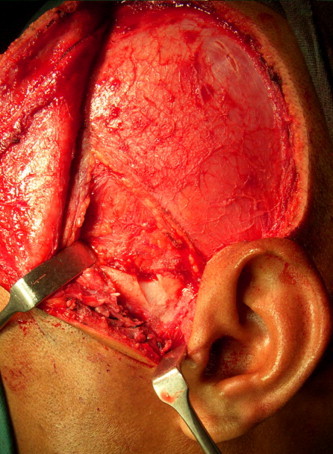
Reconstruction of the TMJ was performed in 10 patients (4 females & 6 males), 7 of them were bilateral and 3 cases were unilateral. The mean age was 40 years (range 28–54). The inclusion criteria were all cases of hypermobility of TMJ refractory to conservative management who were fit to undergo surgery under general anesthesia. True cases of Internal derangement were excluded from the study. TMJ Patient selection was based on impairment of TMJ function during speech, mastication and laughing. The clinical history pertaining to dietary habits involving wide mouth opening, betel nut chewing and trauma did not contribute to the etiology of hypermobility in any of the cases. All patients had been treated non-surgically at various centers of our organization for at least 1 year using analgesics, sedatives and anti-inflammatory medication with or without splints. Clinical examination revealed the usual signs and symptoms of TMJ dysfunction: (a) Pain in the preauricular, facial and cranial areas, (b) Joint noises during mandibular movements, (c) Disturbance of mandibular movements and excessive mouth opening while the condyle in anterior relation to the eminence. Pain was noticed in 6 patients in the preauricular region with radiation to temporal region. Joint click during mandibular movement were noticed in all the cases. All patients were edentulous with no alteration in vertical dimension. The mean mouth opening was 48 mm (range 42–52) (Fig. 1). Radiographic examination (TMJ open & closed mouth) was performed prior to surgery for each patient. No significant change in the outline of articular eminence, tubercle, glenoid fossa and mandibular condyle was noticed (Fig. 2). The diagnosis was chronic habitual subluxation in 7 patients and recurrent dislocation of the TMJ in 3 patients. The TMJ was approached through Popowich & Crane’s modification of Alkayat & Bramley’s preauricular incision to permit anterior mobilization of the tissue and exposure of the capsule of the TMJ, temporal fascia and the zygomatic root of the temporal bone without damaging the facial nerve. An osteotomy of the zygomatic root of the temporal bone was carried out by creating a gap of 0.5 cm directed at 45 towards the joint, just in front of the articular tubercle and eminence (Figs. 3 and 4). A piece of cortico-cancellous bone, taken from the iliac crest of 0.5 cm × 1.5 cm, was placed into the gap, without fixation, to prevent forward movement of the condyle beyond the eminence (Fig. 5). An inferiorly based pedicled flap from the temporal fascia was elevated and sutured to the antero-lateral wall of the capsule as an anchoring procedure (Figs. 6 and 7). The surgical procedure was performed without opening the capsule to avoid further damage to the intra articular structures. Intraorally pterygoid disjunction was carried out in 6 cases (Fig. 8). A soft diet was advised postoperatively for all patients for 4 weeks.
Fig. 1.
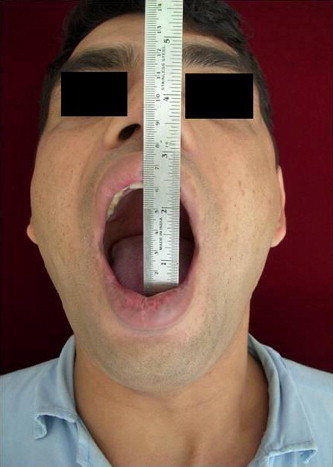
Increased preoperative mouth opening.
Fig. 2.

Hypermobility of TMJ on TMJ open mouth view.
Fig. 3.
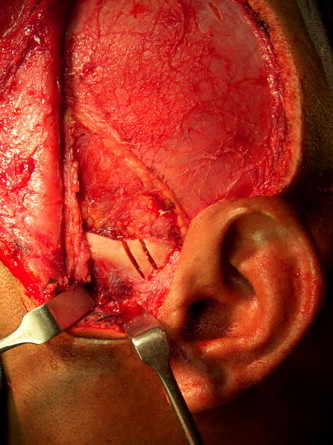
Osteotomy cuts for glenotemporal osteotomy.
Fig. 4.
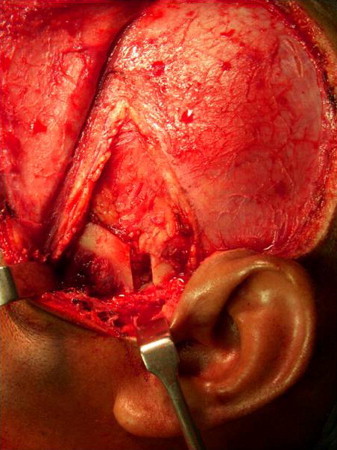
Glenotemporal osteotomy.
Fig. 5.
Interpositioning of Iliac crest graft.
Fig. 6.
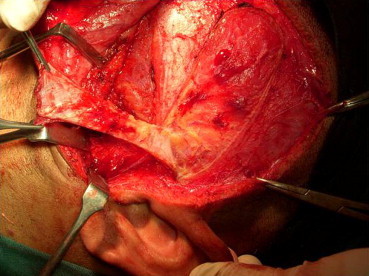
Harvesting pedicled temporofascial flap.
Fig. 7.
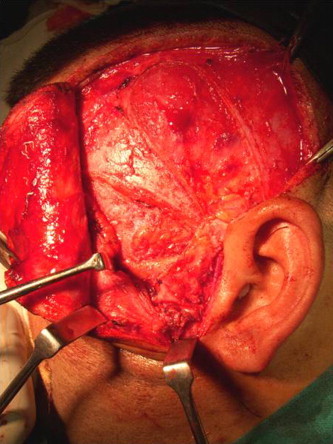
Suturing temporofascial flap over the antero-lateral aspect of TMJ capsule.
Fig. 8.
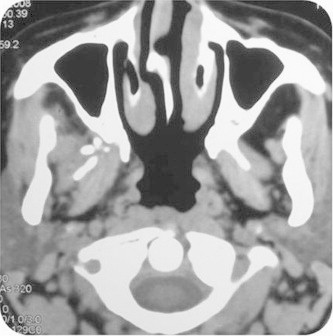
Axial section showing pterygoid disjunction.
Results
At one year follow up the average mouth opening was 38 mm (range 37–40mm). In one case transient facial nerve palsy was noticed along the distribution of temporal and zygomatic branches which subsided after 8 weeks. In none of the cases graft failed or rejected though recurrence along with TMJ pain was noticed in 2 cases. Restriction of translator movement corresponding to actual average mouth opening was evident post surgery in 8 cases (Fig. 9). Postoperative radiographs demonstrated the success of bone grafting and condylar head appeared to have normal range of movement (Fig. 10).
Fig. 9.

Postoperative mouth opening.
Fig. 10.

Restricted translation of condyle post surgery.
Discussion
Many surgical procedures have been advocated for treatment of hypermobility of the TMJ. Conservative approaches include limiting the excursion of the condyle, including physical therapy; splints, intra articular sclerosing injections cause joint fibrosis and use of Botulinum type-A toxin. These treatments are rarely successful and therefore, surgery is often indicated. The surgical options can be divided in two main techniques. The first option consists of creating a barrier to the extreme anterior slide of the condyle. It may be done through capsular plication, eminoplasty or intentional fracture of zygomatic arch or Dautrey’s procedure. Dautrey’s procedure has 3 limitations – internal derangement is possible, procedure is not possible at older age and there is a risk of the fragment relocating. The second option involves removing any barrier for spontaneous reduction which is accomplished best by eminectomy. Long term results have shown that even after performing eminectomy the condyle may continue to dislocate and further can cause articular damage leading to painful TMJ dysfunction.6 Adding two modifications to the conventional procedure we can address the laxity of the capsule, atrophied eminence and associated pain in hypermobility of TMJ in a single attempt. The temporal fascial flap is easy to rotate, prevents laxity of the capsule, reinforces the temporomandibular ligament and further induces scar formation.7 Pterygoid disjunction is an effective method to reduce pain associated with internal derangement of TMJ associated with hypermobility. It reduces the effective length/strength of lateral pterygoid muscle and thereby providing rest to the joint.8 After two years Raja Kummoona achieved 100% success in all 7 cases of hypermobility with average postoperative mouth opening of 32.5 mm.7 A.M. Medra et al observed one recurrence out of 60 cases operated. The average postoperative mouth opening after 1 year was 42 mm.8 The results of our study are quite comparable. This technique is versatile but long-term follow up on a larger group of patients is, of course necessary to be able to draw definitive conclusions.
References
- 1.Costas Lopez A., Monje Gil F., Fernandez Sanroman J., Goizueta Adame C., Castro Ruiz P.C. Glenotemporal osteotomy as a definitive treatment for recurrent dislocation of the jaw. J Craniomaxillofac Surg. 1996;24:178–183. doi: 10.1016/s1010-5182(96)80053-9. [DOI] [PubMed] [Google Scholar]
- 2.Bakardjiev Angel. Treatment of chronic mandibular dislocations by bone plates: two case reports. J Craniomaxillofac Surg. 2004;32:90–92. doi: 10.1016/j.jcms.2003.09.010. [DOI] [PubMed] [Google Scholar]
- 3.Norman JE de B. Recurrent dislocation of the temporomandibular joint. Glenotemporal osteotomy and a modified dowel graft. European Association for Maxillofacial Surgery, 7th Congress, 1984. Abstracts 97.
- 4.Norman J.E. de B.A., Bramley P. Wolfe Medical Publications; London: 1990. Textbook and Colour Atlas of the Temporomandibular Joint. [Google Scholar]
- 5.Mani Varghese. Pterygoid plate disjunction: minimally invasive treatment for internal derangement of the temporomandibular joint. Asian J Oral Maxillofac Surg. 2005;17:247–255. [Google Scholar]
- 6.Medra A.M., Mahrous A.M. Glenotemporal osteotomy and bone grafting in the management of chronic recurrent dislocation and hypermobility of the temporomandibular joint. Br J Oral Maxillofac Surg. 2008;46:119–122. doi: 10.1016/j.bjoms.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Kummoona R. Surgical reconstruction of the temporomandibular joint for chronic subluxation and dislocation. Int J Oral Maxillofac Surg. 2001;30:344–348. doi: 10.1054/ijom.2000.0090. [DOI] [PubMed] [Google Scholar]
- 8.Kannan S.V., Thangavelu A. Pterygoid plate disjunction: minimally invasive treatment of painful TMJ dysfunction. Int J Oral Maxillofac Surg. 2007;36(11):1068. [Google Scholar]


