Abstract
Alcohol-exposed pregnancy (AEP) is a significant public health problem in the United States. Sexually transmitted disease (STD) clinics serve female clients with a high prevalence of heavy alcohol consumption coupled with ineffective contraceptive use. Project CHOICES (Changing High-Risk AlcOhol Use and Increasing Contraception Effectiveness) is an evidence-based, brief intervention to lower risk of AEP by targeting alcohol and contraceptive behaviors through motivational interviewing and individualized feedback. We describe our experience integrating and implementing CHOICES in STD clinics. This endeavor aligns with CDC's National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention's program collaboration and service integration strategic priority to strengthen collaborative work across disease areas and integrate services provided by related programs at the client level.
This article describes the adaptation, implementation, and effectiveness of an evidence-based intervention to reduce alcohol-exposed pregnancy (AEP) in sexually transmitted disease (STD) clinics, using program collaboration and service integration (PCSI) principles from the Centers for Disease Control and Prevention (CDC) National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention 2009 white paper.1 The five key principles of PCSI are:
Appropriateness: The integration of prevention services must make epidemiologic and programmatic sense and should be contextually appropriate.
Effectiveness: Prevention resources are far too limited to be wasted on ineffective or unproven interventions or settings.
Flexibility: Health organizations need the ability to respond to changes in disease epidemiology, demographics, advances in technology, and policy/political imperatives.
Accountability: Prevention partners need the ability to monitor key aspects of their prevention services and gain insight into how they can optimize operations to maximize opportunities for prevention.
Acceptability: To be effective, PCSI must be accepted by program staff members and service providers, as well as by the people they serve.
PCSI PRINCIPLES AND STD CLINICS
Appropriateness—why STD clinics should be involved in efforts to reduce the risk of AEP
Alcohol use by pregnant women is a major public health problem in the United States. Prenatal alcohol use is estimated to affect 1% of births annually and can result in a range of consequences: alcohol-related birth defects, alcohol-related neurodevelopmental disorders, fetal alcohol syndrome, and death.2–5 Fetal alcohol spectrum disorders (FASDs) are among the leading, preventable causes of developmental disorders in the U.S.
Nearly 2% of pregnant women and about 13% of nonpregnant women of reproductive age in the U.S. are estimated to engage in binge drinking (defined at the time as ≥5 standard alcoholic drinks per occasion).6 Heavy alcohol use for women is currently defined by the National Institute on Alcohol Abuse and Alcoholism as ≥4 standard alcoholic drinks in one day (binge drinking) and/or ≥8 alcoholic drinks in one week.7
At STD clinics, there is a high prevalence of women presenting for care who are at risk for AEP because of high rates of heavy alcohol use, no/ineffective contraceptive use, and pregnancy among alcohol users.8,9 High rates of heavy alcohol use by women have been reported in STD clinics, with 30% of women reporting binge drinking in the prior month.8 Approximately 50% of women attending STD clinics are not using effective contraception, even if not intending to get pregnant.10 In a six-year study of Baltimore, Maryland, STD clinics, alcohol use was reported by 33% of women who knew they were pregnant before their visit and by 38% of women who were diagnosed as pregnant at their STD clinic visit.9 Approximately 10%–20% of women attending STD clinics are pregnant.11,12
The higher rates of alcohol use with pregnancy seen in STD clinics are not surprising. The highest levels of heavy alcohol use, and the highest incidences of Chlamydia trachomatis and Neisseria gonorrhoeae infections, have been found in 15- to 24-year-olds.13,14 Multiple studies have suggested a correlation between alcohol use and acquisition of STDs, associated with increases in risky behavior such as number of sex partners, less condom use, and receptive anal sex.8,12,15,16–18 Unplanned pregnancy is also associated with heavy alcohol use in women attending STD clinics.12
Effectiveness—what STD clinics can do to reduce the risk of AEP in women
Effective interventions for women at risk for AEP are possible. Information and education alone have not been shown to affect STD risk behavior, contraceptive use, or alcohol consumption.19 However, brief interventions, in conjunction with screening for risk behaviors, have been shown to be efficacious in a variety of settings.5,20–27
Project CHOICES (Changing High-Risk AlcOhol Use and Increasing Contraception Effectiveness) is an integrated behavioral intervention for the prevention of prenatal alcohol exposure in women at high-risk for AEP. It was initiated by CDC in 1997 and developed in collaboration with experts in alcohol treatment, fetal alcohol syndrome, screening and brief intervention for behavior change, and service delivery. The intervention was based on motivational interviewing (MI) and included personalized feedback about drinking levels, a decisional balance exercise to weigh the pros and cons of changing drinking and contraceptive behavior, the importance/readiness/confidence rulers to assess ability to change, goal-setting for drinking limits, and a review of barriers and facilitators to change.28 Treatment included four manual-guided sessions delivered by mental health clinicians and one contraceptive counseling session delivered by a family planning (FP) clinician. In a randomized controlled trial (RCT) in three cities and six community settings (jails, drug/alcohol treatment centers, suburban primary care practices, a hospital-based gynecology clinic, and a Medicaid health maintenance organization), Project CHOICES was compared with usual care among 830 women at risk of AEP. At the nine-month follow-up evaluation, 69% of women in the CHOICES intervention reported reducing their risk of AEP compared with 54% of women in the information-only group.21 Project CHOICES had demonstrated efficacy in a variety of diverse settings; the next phase was to determine its effectiveness in STD clinics, where there were high rates of heavy alcohol use and ineffective contraception. “Effectiveness” was defined as a reduction in risk of AEP (reduction in alcohol use below heavy levels and/or increase in effective contraceptive use) when delivering CHOICES as part of integrated care in the STD clinic. Acceptance of CHOICES by providers, clinic staff, and clients was a secondary criterion of effectiveness.
Flexibility—making interventions shown to be efficacious in an RCT effective in STD clinics
In 2009, the Baltimore City Health Department and the Colorado Department of Public Health and Environment were funded by CDC to implement CHOICES in STD clinics. The Baltimore and Denver sites had high rates of heavy alcohol use (exceeding the national average for women of reproductive age) and ineffective contraceptive use. Ineffective contraceptive use was defined as failure to use condoms, or a hormonal or intrauterine device as directed, for every episode of vaginal sex. Both also had contraceptive services through Title X FP clinics, either co-located in the same building (Baltimore) or integrated into the STD clinic (Denver). Finally, both clinics had appropriate infrastructures and experience to support this behavioral intervention with long-term follow-up of clients.
The challenge for both sites was to introduce an alcohol risk-reduction program to clients, providers, and staff in STD clinics. In Baltimore, there was an additional challenge of introducing contraceptive care, because FP services were delivered in a separate clinic site.
CDC and the original developers of CHOICES provided training on MI and CHOICES to project staff from both sites. The sites then pilot tested the CHOICES curriculum with STD clinic patients to ensure acceptability. Adaptations were made using feedback from the pilot activities and in consultation with CDC and CHOICES experts. For STD clinics that typically treat clients in a single visit, a two-session counseling model and two booster phone calls were determined to be more feasible than the original four-session CHOICES. As the second session was expected to show some loss of participation, the essential elements were placed into the first session, while the second session reviewed successes or barriers to goals and plans for change. The two sites independently adapted the curriculum to be more culturally appropriate and to match population literacy levels. At both sites, project staff supervised CHOICES counselors and patient navigators. The patient navigators guided clients through each step of the intervention.
As this project represented a new direction for both STD clinics, numerous steps were completed before enrolling participants into the program. Both sites hired and trained an MI counselor to deliver CHOICES and a patient navigator for recruitment and the three- and six-month follow-up evaluations. Physical space was identified in each clinic to serve as a counseling room to deliver CHOICES. Acceptability of STD CHOICES to health department staff was critical to successful project integration and is a key PSCI principle as well. The sites provided information and ongoing project updates to STD clinic staff about AEP to improve awareness of the problem and increase investment in STD CHOICES. (We formally and informally solicited feedback about the project, as we discuss later.) Sites also presented continuing education lectures in the health department on AEP, FASDs, and detection/treatment of alcohol misuse in women. These sessions were open to all providers and staff. Both sites partnered with substance abuse treatment programs, which served as referral resources if more intensive alcohol treatment was deemed necessary. Information was placed on the health departments' websites. All participants were given a resource guide containing information on local health centers, drug/alcohol treatment centers, and other services.
FP services are not offered as usual care in Baltimore STD clinics; therefore, add-on services were required. We offered QuickStart, a service that allows the STD clinic provider to start a woman on oral contraceptives or medroxyprogesterone injectable immediately after a CHOICES session. Women also had the option to attend the FP clinic for a separate visit if they wanted other types of birth control or for follow-up. The patient navigator assisted with this transition. QuickStart had the unintended but positive consequence of facilitating service integration between STD and FP clinics. Women who initiated birth control in the STD clinic or the FP clinic were included in the outcomes evaluation. In Denver, STD treatment and FP services were already integrated.
Accountability—determining and measuring the efficacy of STD CHOICES
We monitored both program logistics (screening, recruitment, and retention statistics) and project effectiveness in reducing AEP. Where monitoring revealed problems with the program logistics, we made adaptations to address the identified barriers. We also found it helpful to compare statistics and client outcomes both across and within each clinic to identify where improvements were needed.
Monitoring screening, recruitment, and retention.
Although Baltimore and Denver demonstrated considerable similarity in the planning activities needed to start CHOICES, systems and population differences led to different methods of approaching screening and recruitment. In Baltimore, because the electronic medical record (EMR) was not modifiable, we prescreened at clinic registration with a single, piloted question: “How often in the last year have you had 3 or more drinks of alcohol?” Women with positive prescreens were called from the waiting room prior to their STD appointment for more complete screening and recruitment. In Denver, screening for heavy alcohol use was conducted by the clinician using their EMR, which was modified prior to implementation of CHOICES. Initially, clinicians conducted the screening and referred positive screens to CHOICES staff; however, this methodology resulted in lower recruitment rates, likely because of the additional clinical burden placed on providers. Instead, providers were asked only to screen and introduce at-risk women to CHOICES staff as the next step in their clinical care. That single change significantly improved recruitment.
Table 1 summarizes the screening, recruitment, and retention of women for STD CHOICES by site. Women 18–44 years of age were ineligible if they were drinking moderately or not at all, not able to become pregnant, did not complete the prescreen (Baltimore), and/or declined to participate.
Table 1.
Screening, recruitment, and retention of women for STD CHOICES, by sitea
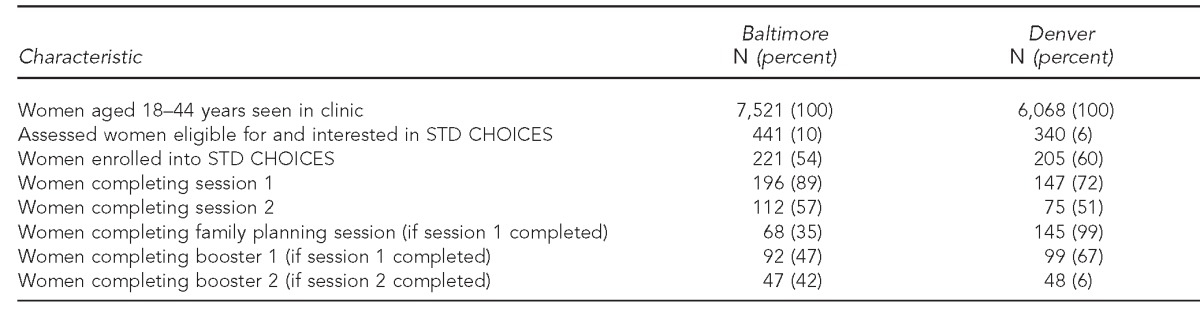
Women were enrolled from October 1, 2010, through March 30, 2012 (for six-month follow-up) and through June 30, 2012 (for three-month follow-up).
STD = sexually transmitted disease
CHOICES = Changing High-Risk AlcOhol Use and Increasing Contraception Effectiveness
More than half of eligible and interested women approached by project staff at both sites chose to enroll (54% in Baltimore and 60% in Denver) and the majority of enrollees completed the first session (89% in Baltimore and 72% in Denver). No incentives were provided for participation or travel to the clinic. Participants returned for the second session (57% in Baltimore and 51% in Denver) at a lower rate, underscoring the importance of concentrating key intervention elements in the first session for the STD clinic setting. Baltimore was more successful in delivering session two because it added the option to complete session two counseling by phone; Denver has followed suit.
Retention at both sites required multimedia, intensive efforts. The population was largely young and frequently changed addresses and phone numbers. As a result, both sites missed women for the booster phone calls (Baltimore completed 45%, while Denver completed 66%). Similarly, rates of lost-to-follow-up were approximately 35% in Baltimore and 43% in Denver as a result of women failing to return to the clinic for follow-up assessment and/or inaccessibility by phone or mail (data not shown). Both sites have made adaptations to follow-up procedures by conducting the second counseling session and the follow-up evaluations by phone. Text message reminders, e-mails, and letters rescheduling missed appointments have helped address this issue. Throughout the year, we sent holiday and birthday cards to participants to maintain contact with them.
Several methods to meet retention goals were initiated. Reminder text messages were very effective. Both sites also used clinic staff to assist with retention. In Baltimore, disease intervention specialists (DISs) helped find and refer women. The EMR was flagged so that staff could notify CHOICES staff when a client returned to the STD clinic. In Denver, the EMR could not be flagged, but clinic and CHOICES staff reviewed the daily clinic schedule to identify women returning for visits. Denver used CHOICES staff to go out into the field. Follow-up assessment rates were initially low at both sites. Both sites improved follow-up rates by conducting assessments by phone if needed. Incentives were initially used to encourage participation in the follow-up assessments, but both sites found that they were unnecessary and discontinued them, thereby replicating real-world service delivery.
Project effectiveness—client outcomes.
All enrolled clients received baseline assessments. Both sites collected basic demographics and brief information about alcohol quantity and frequency and contraceptive use at baseline and at the three- and six-month follow-up assessments. Women were considered at reduced risk for AEP if they used contraception effectively, reduced alcohol consumption to <4 drinks on one occasion and <8 drinks/week, or used contraception effectively and reduced alcohol consumption.
The sites differed in basic demographics as well as in alcohol consumption. In Baltimore, 55% of the women were ≥25 years of age and largely African American (87%); in Denver, 51% of the women were 18–24 years of age and primarily white (62%), with 41% identifying Hispanic ethnicity. On average, Baltimore women binged on more days than did Denver women (6.9 days vs. 5.5 days/month). Denver women consumed more alcoholic drinks/day (7.2 vs. 4.7) and had a higher number of average drinks/week (25.1 vs. 14.6) than Baltimore women. All participants had ineffective contraceptive use at baseline (data not shown).
At the three-month follow-up, 81% of Baltimore women who returned reduced their risk for AEP: 15% reduced alcohol consumption only, 36% chose effective contraception only, and 30% both reduced alcohol consumption and used effective contraception. In Denver, 74% of women reduced their risk for AEP: 26% reduced alcohol consumption only, 33% chose effective contraception only, and 15% both reduced alcohol consumption and used effective contraception (Table 2). At both sites, sexual abstinence was a significant contraceptive choice: 18% of women in Baltimore and 10% of women in Denver reported choosing sexual abstinence (data not shown).
Table 2.
Outcomes for women participating in STD CHOICES, by site and follow-up montha
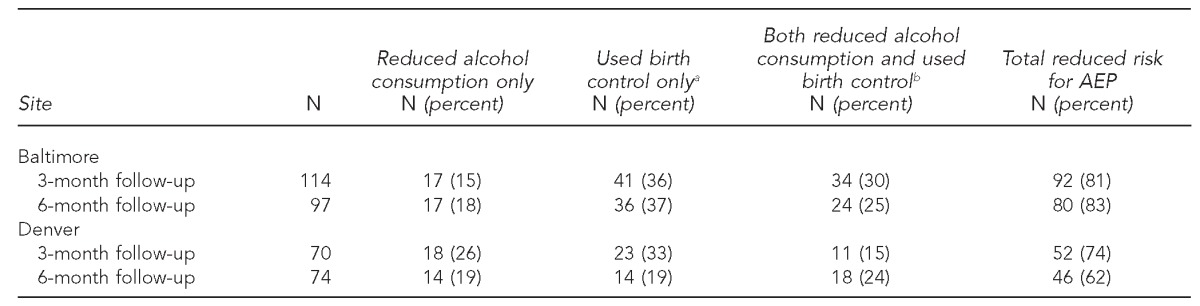
Women were enrolled from October 1, 2010, through March 30, 2012 (for six-month follow-up) and through June 30, 2012 (for three-month follow-up).
bIncludes hormonal method/intrauterine device, abstinence from vaginal sex, and 100% condom use
AEP = alcohol-exposed pregnancy
Of the women who participated in the six-month follow-up, 83% of Baltimore women reduced their risk for AEP: 18% reduced alcohol consumption only, 37% chose effective contraception only, and 25% both reduced alcohol consumption and used effective contraception. In Denver, 62% of women reduced their risk for AEP: 19% reduced alcohol consumption only, 19% chose effective contraception only, and 24% both reduced alcohol consumption and used effective contraception (Table 2). Denver women were more likely than Baltimore women to choose hormonal/intrauterine device methods of birth control, while 18% of Baltimore women chose 100% condom use but no other birth-control method. More women in Baltimore than Denver opted for sexual abstinence (data not shown).
Site differences in outcomes were likely attributable to differences in age, baseline alcohol consumption, and location of the STD/FP clinics. Contraception rates in both clinics were maintained from the three- to six-month evaluation, and rates of alcohol consumption continued to decrease. The percentages of those receiving at least one session who provided follow-up data at three and six months, respectively, were 58% and 49% in Baltimore and 48% and 50% in Denver (data not shown).
Acceptability—acceptance of STD CHOICES by clinicians, other STD staff members, and women eligible for the intervention
Anonymous client satisfaction surveys were completed at both clinics after each session, as well as client assessment of information gained and expected behavior change. On average, one-third of women completed these surveys, with both sites scoring 4.9–5.0 on a scale of 1–5 (5 = very satisfied).
Anonymous surveys were also conducted biannually with medical and administrative staff to measure their perception of goals, utility for clients, and integration into clinic flow. To encourage completion of the survey, respondents could enter a raffle for a gift certificate to a local store. Our survey response rate was 100%; 95%–100% of staff demonstrated an understanding of CHOICES and its effectiveness for women's health, and endorsed the view that CHOICES was well integrated into clinic flow.
CONCLUSIONS
Project CHOICES was effectively implemented in both STD clinics and satisfied the five principles of PCSI.1 Prevention of AEP was appropriate in STD clinics, as women who present to these clinics have high rates of heavy alcohol use coupled with ineffective contraception. The previous CHOICES RCTs showed that the intervention was efficacious; outcome data from this demonstration project show that it can successfully be translated into the STD clinic setting and is effective. The adaptations undertaken by each STD CHOICES site demonstrate the program's flexibility. For accountability, STD clinics can set measurable process standards (e.g., screening and referral rates and intervention completion rates) and outcome standards for reduced AEP risk. If resources allow, self-report could be supplemented using registry data.
Both sites showed that STD CHOICES was acceptable to clinic providers and staff by early engagement, effective communication, and integration into clinic flow. Screening that was quick, universal, easily incorporated into usual clinic procedures, and non-stigmatizing was found to be acceptable for both staff and clients. Two face-to-face sessions were feasible, although we recommend that session 1 contain the essential elements that are reinforced in session 2 in case session 2 is not completed. Session 2 was possible to conduct by phone if needed. Retention was increased by the use of text messages, client flags in EMRs to alert about clinic entry, use of DISs, and engagement of clinic staff. Integrated STD and FP services (i.e., in Denver) increased uptake of effective contraception; although, at six months, the frequency of birth-control use was similar at both sites. Identifying eligible and interested women and retaining them for follow-up evaluations will always be a challenge in a busy STD clinic where one visit is the norm for care. However, both sites were successful in working with their particular challenges, suggesting that other STD clinics can also integrate this program by addressing factors particular to their populations, staff, and medical records.
A dedicated interventionist position may not be feasible in STD clinics; therefore, to sustain CHOICES, Baltimore and Denver are training other health department staff. In Baltimore, social workers are adding CHOICES/MI to their clinical toolkit, whereas in Denver, paraprofessional staffers are adding MI/CHOICES to their other duties.
To support dissemination, CDC has a website that provides open access to CHOICES curriculum materials for clients, counselors, and training of counselors.29 CDC also provides background materials on MI, CHOICES, and FASD and is currently training trainers who may assist other clinics interested in implementing CHOICES.
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The Johns Hopkins Medicine Institutional Review Board (IRB) determined that the study did not involve human subjects and, therefore, was exempt from IRB review.
REFERENCES
- 1.Centers for Disease Control and Prevention (US) Atlanta: Department of Health and Human Services (US), CDC; 2009. Program collaboration and service integration: enhancing the prevention and control of HIV/AIDS, viral hepatitis, sexually transmitted diseases, and tuberculosis in the United States. Also available from: URL: http://www.cdc.gov/nchhstp/programintegration/docs/207181-C_NCHHSTP_PCSI%20WhitePaper-508c.pdf [cited 2012 May 31] [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration (US) Fetal alcohol spectrum disorders by the numbers. 2007. [cited 2012 Jun 27]. Available from: URL: http://store.samhsa.gov/shin/content//SMA06-4236/SMA06-4236.pdf. [PubMed]
- 3.National Institutes of Health (US) Fetal alcohol spectrum disorders fact sheet. 2010. [cited 2012 May 31]. Available from: URL: http://report.nih.gov/nihfactsheets/Pdfs/FetalAlcoholSpectrum Disorders(NIAAA).pdf.
- 4.Ingersoll K, Floyd L, Sobell M The Project CHOICES Intervention Research Group. Reducing the risk of alcohol-exposed pregnancies: a study of a motivational intervention in community settings. Pediatrics. 2003;111(5 Pt 2):1131–5. [PubMed] [Google Scholar]
- 5.Ingersoll KS, Ceperich SD, Nettleman MD, Karanda K, Brocksen S, Johnson BA. Reducing alcohol-exposed pregnancy risk in college women: initial outcomes of a clinical trial of a motivational intervention. J Subst Abuse Treat. 2005;29:173–80. doi: 10.1016/j.jsat.2005.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tsai J, Floyd RL, Green PP, Boyle CA. Patterns and average volume of alcohol use among women of childbearing age. Matern Child Health J. 2007;11:437–45. doi: 10.1007/s10995-007-0185-4. [DOI] [PubMed] [Google Scholar]
- 7.National Institute on Alcohol Abuse and Alcoholism (US) Moderate and binge drinking [cited 2012 May 22] Available from: URL: http://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking.
- 8.Hutton HE, McCaul ME, Santora PB, Erbelding EJ. The relationship between recent alcohol use and sexual behaviors: gender differences among sexually transmitted disease clinic patients. Alcohol Clin Exp Res. 2008;32:2008–15. doi: 10.1111/j.1530-0277.2008.00788.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson HL, Erbelding EJ, Zenilman JM, Ghanem KG. Sexually transmitted diseases and risk behaviors among pregnant women attending inner city public sexually transmitted diseases clinics in Baltimore, MD, 1996–2002. Sex Transm Dis. 2007;34:991–4. doi: 10.1097/olq.0b013e31812e6b9a. [DOI] [PubMed] [Google Scholar]
- 10.Godfrey EM, Wheat SG, Cyrier R, Wong W, Trussell J, Schwarz EB. Contraceptive needs of women seeking care from a publicly funded sexually transmitted infection clinic. Contraception. 2010;82:543–8. doi: 10.1016/j.contraception.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shlay JC, Zolot L, Bell D, Maravi ME, Urbina C. Association between provision of initial family planning services and unintended pregnancy among women attending an STD clinic. J Womens Health (Larchmt) 2009;18:1693–9. doi: 10.1089/jwh.2008.0966. [DOI] [PubMed] [Google Scholar]
- 12.Thomas AG, Brodine SK, Shaffer R, Shafer MA, Boyer CB, Putnam S, et al. Chlamydial infection and unplanned pregnancy in women with ready access to health care. Obstet Gynecol. 2001;98:1117–23. [PubMed] [Google Scholar]
- 13.Department of Health and Human Services (US), Substance Abuse and Mental Health Services Administration. Rockville (MD): SAMHSA; 2011. Results from the 2010 National Survey on Drug Use and Health: summary of national findings. NSDUH Series H-41. Also available from: URL: http://oas.samhsa.gov/NSDUH/2k10NSDUH/2k10Results.htm#3.1.3 [cited 2012 May 15] [Google Scholar]
- 14.Centers for Disease Control and Prevention (US) 2010 sexually transmitted diseases surveillance [cited 2012 May 16] Available from: URL: http://www.cdc.gov/std/stats10/toc.htm.
- 15.Cook RL, Comer DM, Wiesenfeld HC, Chang CH, Tarter R, Lave JR, et al. Alcohol and drug use and related disorders: an underrecognized health issue among adolescents and young adults attending sexually transmitted disease clinics. Sex Transm Dis. 2006;33:565–70. doi: 10.1097/01.olq.0000206422.40319.54. [DOI] [PubMed] [Google Scholar]
- 16.Seth P, Sales JM, DiClemente RJ, Wingood GM, Rose E, Patel SN. Longitudinal examination of alcohol use: a predictor of risky sexual behavior and Trichomonas vaginalis among African-American female adolescents. Sex Transm Dis. 2011;38:96–101. doi: 10.1097/OLQ.0b013e3181f07abe. [DOI] [PubMed] [Google Scholar]
- 17.Staras SA, Tobler AL, Maldonado-Molina MM, Cook RL. Riskier sexual partners contribute to the increased rate of sexually transmitted diseases among youth with substance use disorders. Sex Transm Dis. 2011;38:413–8. doi: 10.1097/OLQ.0b013e31820279a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suss AL, Homel P, Hammerschlag M, Bromberg K. Risk factors for pelvic inflammatory disease in inner-city adolescents. Sex Transm Dis. 2000;27:289–91. doi: 10.1097/00007435-200005000-00010. [DOI] [PubMed] [Google Scholar]
- 19.DiClemente RJ, Wingood GM, Sionean C, Crosby R, Harrington K, Davies S, et al. Association of adolescents' history of sexually transmitted disease (STD) and their current high-risk behavior and STD status: a case for intensifying clinic-based prevention efforts. Sex Transm Dis. 2002;29:503–9. doi: 10.1097/00007435-200209000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Floyd RL, Weber MK, Denny C, O'Connor MJ. Prevention of fetal alcohol spectrum disorders. Dev Disabil Res Rev. 2009;15:193–9. doi: 10.1002/ddrr.75. [DOI] [PubMed] [Google Scholar]
- 21.Floyd RL, Sobell M, Velasquez MM, Ingersoll K, Nettleman M, Sobell L, et al. Project CHOICES Efficacy Study Group. Preventing alcohol-exposed pregnancies: a randomized controlled trial. Am J Prev Med. 2007;32:1–10. doi: 10.1016/j.amepre.2006.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Floyd RL, Ebrahim S, Tsai J, O'Connor M, Sokol R. Strategies to reduce alcohol-exposed pregnancies. Matern Child Health J. 2006;10(5 Suppl):S149–51. doi: 10.1007/s10995-006-0116-9. [DOI] [PubMed] [Google Scholar]
- 23.Manwell LB, Fleming MF, Mundt MP, Stauffacher EA, Barry KL. Treatment of problem alcohol use in women of childbearing age: results of a brief intervention trial. Alcohol Clin Exp Res. 2000;24:1517–24. [PubMed] [Google Scholar]
- 24.Substance Abuse and Mental Health Services Administration (US) Screening, brief intervention, and referral to treatment (SBIRT) [cited 2012 May 22] Available from: URL: http://www.samhsa.gov/prevention/SBIRT/SBIRTwhitepaper.pdf.
- 25.Department of Health and Human Services (US), Substance Abuse and Mental Health Services Administration. Rockville (MD): SAMHSA; 2011. Screening, brief intervention and referral to treatment (SBIRT) in behavioral healthcare. Also available from: URL: http://www.samhsa.gov/prevention/SBIRT/SBIRTwhitepaper.pdf [cited 2012 May 22] [Google Scholar]
- 26.Kamb ML, Fishbein M, Douglas JM, Jr, Rhodes F, Bolan G, Zenilman J, et al. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: a randomized controlled trial. Project RESPECT Study Group. JAMA. 1998;280:1161–7. doi: 10.1001/jama.280.13.1161. [DOI] [PubMed] [Google Scholar]
- 27.Jemmott LS, Jemmott JB, III, O'Leary A. Effects on sexual risk behavior and STD rate of brief HIV/STD prevention interventions for African American women in primary settings. Am J Public Health. 2007;97:1034–40. doi: 10.2105/AJPH.2003.020271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Velasquez MM, Ingersoll KS, Sobell MB, Floyd RL, Sobell LC, von Sternberg K. A dual-focus motivational intervention to reduce the risk of alcohol-exposed pregnancy. Cogn Behav Pract. 2010;17:203–12. doi: 10.1016/j.cbpra.2009.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention (US) National Center on Birth Defects and Developmental Disabilities [cited 2013 Feb 5] Available from: URL: http://www.cdc.gov/ncbddd/index.html.


