Abstract
Objective
A physically active lifestyle is recommended for overall health—both physical and mental. Serious psychological distress (SPD) is associated with adverse health behaviors. We compared patterns of physical activity (PA) among adults with and without SPD using current public health guidelines for PA and examined whether adults with SPD were physically active at recommended levels.
Methods
We used data from the 2009 Behavioral Risk Factor Surveillance System (BRFSS) to assess SPD using the Kessler 6 (K6) scale of nonspecific psychological distress and PA categories based on the 2008 U.S. Department of Health and Human Services guidelines. Complete data were available for 78,886 adults in 16 states that used an optional BRFSS mental illness and stigma module containing the K6 scale. We performed multiple logistic regression analyses to estimate prevalence ratios (PRs) and 95% confidence intervals (CIs).
Results
The unadjusted prevalence of SPD was 3.9% (95% CI 3.6, 4.2), and the age-adjusted prevalence of SPD was 3.8% (95% CI 3.5, 4.1). After adjusting for age, sex, race/ethnicity, education, employment, body mass index, smoking status, and heavy drinking, adults with SPD were significantly less likely to be physically active at recommended levels than adults without SPD. PRs were attenuated but remained significant after further adjustment for limitations to PA.
Conclusion
Adults with SPD are less likely to meet current PA recommendations than adults without SPD, highlighting the need for targeted interventions.
Serious psychological distress (SPD), while not indicative of a specific mental illness, is associated with anxiety and mood disorders.1,2 In 2012, the U.S. Substance Abuse and Mental Health Services Administration (SAMHSA) compared National Survey on Drug Use and Health (NSDUH) mental health data with other data sources.3 SAMHSA reported that the estimated prevalence of past-year SPD was 10.2% using the 2009 NSDUH. The estimated prevalences of past-year serious mental illness and any mental illness (i.e., ≥1 mental disorder excluding substance abuse) were 4.8% and 19.9%, respectively, using NSDUH data, and 5.8% and 24.8%, respectively, using National Comorbidity Survey Replication data.3,4 Past 30-day estimates of SPD were 3.1% using National Health Interview Survey (NHIS) data, 4.6% using NSDUH data, and 4.8% using Medical Expenditure Panel Survey (MEPS) data.3
SPD is frequently comorbid with chronic physical conditions and disabilities, resulting in an increased risk for adverse health outcomes and premature death.5–7 In addition, SPD is highly associated with adverse health behaviors, such as smoking, physical inactivity, and substance abuse.8–11 The economic costs of mental disorders are substantial. While an estimated 6.2% of U.S. health-care spending is attributed to mental disorders,12 the true cost of these disorders is elusive, as they are mainly indirect, such as increased work absenteeism and decreased productivity, increased risk of unemployment and subsequent reliance on social services disability income, and other adverse consequences (e.g., reduced educational attainment, homelessness, and incarceration).13,14
The overall health benefits of physical activity (PA) are well known.11,15–23 In 2008, the U.S. Department of Health and Human Services (HHS) published revised PA recommendations informed by the most recent scientific evidence available. These new public health guidelines recommend a physically active lifestyle not only for physical health but also for mental health.23 Similarly, many organizations have recognized the intertwined relationship between mental and physical health, especially the role PA has in improving and maintaining mental health.11,15,17–22,24–26 For example, the American Psychiatric Association's (APA's) clinical practice guidelines include PA as an initial treatment modality in patients with mild depressive disorder, and as an adjunct therapy for patients no matter the severity of depression.17,22 Given the comprehensive health benefits of PA, further elucidation of the PA patterns among adults with SPD is needed to establish a baseline and to inform public health strategies; primary care collaborative care models; and clinical protocols designed to prevent adverse health outcomes, treat mental disorders, and improve the quality of life among this population.
Thus, this study had two goals: (1) to compare the PA patterns of adults with and without SPD and (2) to examine whether adults with SPD are physically active in accordance with the 2008 HHS PA guidelines.
METHODS
We used data from the 2009 Behavioral Risk Factor Surveillance System (BRFSS).27 The BRFSS is an ongoing landline telephone survey conducted by state health departments in collaboration with the Centers for Disease Control and Prevention that collects data on many of the behaviors and conditions that place people at risk for illness, disability, and death in the United States. In 2009, a total of 432,607 adults aged ≥18 years from all 50 states, the District of Columbia, and three territories participated in the survey.
Ascertainment of SPD status
In 2009, 16 states (California, Georgia, Hawaii, Kansas, Massachusetts, Michigan, Mississippi, Missouri, Nebraska, Nevada, South Carolina, Tennessee, Utah, Vermont, Washington, and Wyoming) administered an optional BRFSS mental illness and stigma (MIS) module that contained the Kessler 6 (K6) scale of nonspecific psychological distress. The K6 scale was developed in 1992 as a short dimensional measure of nonspecific psychological distress in the past 30 days.2 The K6 scale identifies people who are likely to meet the Diagnostic and Statistical Manual, Fourth Edition (DSM-IV)28 criteria for anxiety and mood disorders in the 30 days before the interview, as well as people with subclinical illness who may not meet the DSM-IV criteria for a specific disorder.1
K6, with optimal scaling rules, is strongly predictive of serious mental illness using the World Health Organization Composite International Diagnostic Interview Version 3.0.29,30 The K6 scale is increasingly used in population-based mental health research and has been validated in multiple settings.1,2,31 The K6 scale consists of six questions on how frequently the respondents experienced the following commonly occurring symptoms of psychological distress in the previous 30 days: nervousness, hopelessness, restlessness, worthlessness, effortfulness, and feeling so depressed that nothing could cheer them up. Possible response options and associated scores are: 4 = all of the time, 3 = most of the time, 2 = some of the time, 1 = a little of the time, and 0 = none of the time. Don't know/not sure responses, refusals to respond, and missing responses were excluded from the analysis. Scores were summed to yield a total score from 0 to 24. Total K6 scores of ≥13 are used to define SPD in the 30 days preceding the interview.32,33
Ascertainment of PA
We used six questions to assess respondents' participation in moderate and vigorous PA during a usual week. Prior to asking the six questions, each respondent was read the following statement: “We are interested in two types of physical activity—vigorous and moderate. Vigorous activities cause large increases in breathing or heart rate while moderate activities cause small increases in breathing or heart rate.” Moderate PA was assessed with the following questions: “Now, thinking about the moderate physical activities you do in a usual week, do you do moderate activities for at least 10 minutes at a time, such as brisk walking, bicycling, vacuuming, gardening, or any other activity that causes small increases in breathing or heart rate?” “How many days per week do you do these moderate activities for at least 10 minutes at a time?” and “On days when you do moderate activities for at least 10 minutes at a time, how much total time per day do you spend doing these activities?” Vigorous PA was assessed with the following questions: “Now, thinking about the vigorous physical activities you do in a usual week, do you do vigorous activities for at least 10 minutes at a time, such as running, aerobics, heavy yard work, or any other activity that causes large increases in breathing or heart rate?” “How many days per week do you do these vigorous activities for at least 10 minutes at a time?” and “On days when you do vigorous activities for at least 10 minutes at a time, how much total time per day do you spend doing these activities?”
According to the 2008 guidelines,23 to be considered physically active at recommended levels, one must accrue a minimum of 150 weekly minutes of moderate-intensity PA, a minimum of 75 weekly minutes of vigorous-intensity PA, or a combination of moderate-intensity and vigorous-intensity PA that totals ≥150 weekly minutes of PA (i.e., where 1 minute of vigorous-intensity PA = 2 minutes of moderate-intensity PA). For our analysis, and consistent with the HHS guidelines, respondents were categorized as (1) highly active (≥301 weekly minutes of PA—meets recommendations), (2) moderately active (150–300 weekly minutes of PA—meets recommendations), or (3) insufficiently active or inactive (≤149 weekly minutes of PA—does not meet recommendations). To examine the overall association between SPD and PA in accordance with current public health recommendations, respondents who were either highly active or moderately active were combined into one group (i.e., meets PA recommendations). Assessment of self-reported PA levels by the BRFSS has been shown to result in valid measurements.34
Covariates
We used sociodemographic variables and other variables known to be associated with both the independent variable (i.e., SPD) and the dependent variable (i.e., level of PA) in our analyses.35–37 The sociodemographic variables included age in years (18–24, 25–34, 35–44, 45–64, and ≥65), gender, race/ethnicity (non-Hispanic [NH] white, NH black, Hispanic, and NH other), education (<high school, high school, and >high school), employment status (employed, unemployed, retired, unable to work, and homemaker or student), and body mass index (BMI, in kilograms per square meter). Additional variables included smoking status, alcohol consumption, and limitations to PA. Smoking status was determined using two questions: (1) “Have you smoked at least 100 cigarettes in your entire life?” and (2) “Do you now smoke cigarettes every day, some days, or not at all?” Respondents who reported ever smoking 100 cigarettes and responded that they now smoke were classified as smokers. Respondents who reported smoking ≥100 cigarettes but no longer smoked, and those who had smoked <100 cigarettes in their lifetimes, were classified as nonsmokers.
Alcohol consumption was determined using two questions: (1) “During the past 30 days, how many days per week or per month did you have at least one drink of any alcoholic beverage?” and (2) “One drink is equivalent to a 12-ounce beer, a 5-ounce glass of wine, or a drink with one shot of liquor. During the past 30 days, on the days when you drank, about how many drinks did you drink on average?” Male respondents who reported consuming >2 drinks per day on average or female respondents who reported consuming >1 drink per day on average were classified as heavy drinkers. Male respondents who reported consuming ≤2 drinks per day on average or female respondents who reported consuming ≤1 drink per day on average were classified as nonheavy drinkers. Respondents with or without limitations for PA were identified with the question, “Are you limited in any way in any activities because of physical, mental, or emotional problems?”
Statistical analysis
We used SAS®38 and SAS-callable SUDAAN®39 in all analyses to account for the complex survey design of the BRFSS. Age-standardized prevalence estimates for SPD or meeting current PA guidelines by sociodemographic variables and other examined confounders were obtained using PROC DESCRIPT with the direct method based on the 2000 U.S. population aged ≥18 years. We used the conventional alpha levels of p<0.05, p<0.01, and p<0.0001 to assess significance. We used multiple logistic regression models with the predictive marginal statement and adjusted risk ratio option to obtain unadjusted and adjusted prevalence ratios (PRs) and 95% confidence intervals (CIs) for adults with SPD who were physically active at recommended levels, using adults without SPD as the reference group.39,40
RESULTS
In the 16 states that used the optional BRFSS MIS module, complete data for all study variables were obtained from 78,886 respondents. Of those, 3,102 (3.9%, 95% CI 3.6, 4.2) were estimated to have SPD. The age-standardized prevalence of SPD was 3.8% (95% CI 3.5, 4.1).
Table 1 provides the age-standardized percentages of PA patterns among adults with and without SPD who met the 2008 guidelines overall and by sociodemographic characteristics and confounders. Overall, 45.4% of adults with SPD and 67.2% of adults without SPD met current aerobic PA recommendations after age standardization (p<0.0001). Across all examined characteristics, lower proportions of adults with SPD were highly active or moderately active compared with those without SPD, with the exception of moderately active retired adults (16.2% of those with SPD vs. 14.6% of those without SPD). Among adults who were highly active, the greatest differences were found among those aged 45–64 years (24.9% of those with SPD vs. 43.4% of those without SPD, p<0.0001), nonsmokers (28.9% of those with SPD vs. 46.0% of those without SPD, p<0.0001), and those who were overweight (30.9% of those with SPD vs. 48.0% of those without SPD, p<0.0001). Among those who were moderately active, the greatest difference in proportions occurred among those of NH other race/ethnicity (8.6% of those with SPD vs. 21.7% of those without SPD, p<0.001).
Table 1.
Age-standardizeda prevalence of meeting 2008 HHS physical activity recommendations among U.S. adults with and without serious psychological distress: 16 states,b BRFSS, 2009
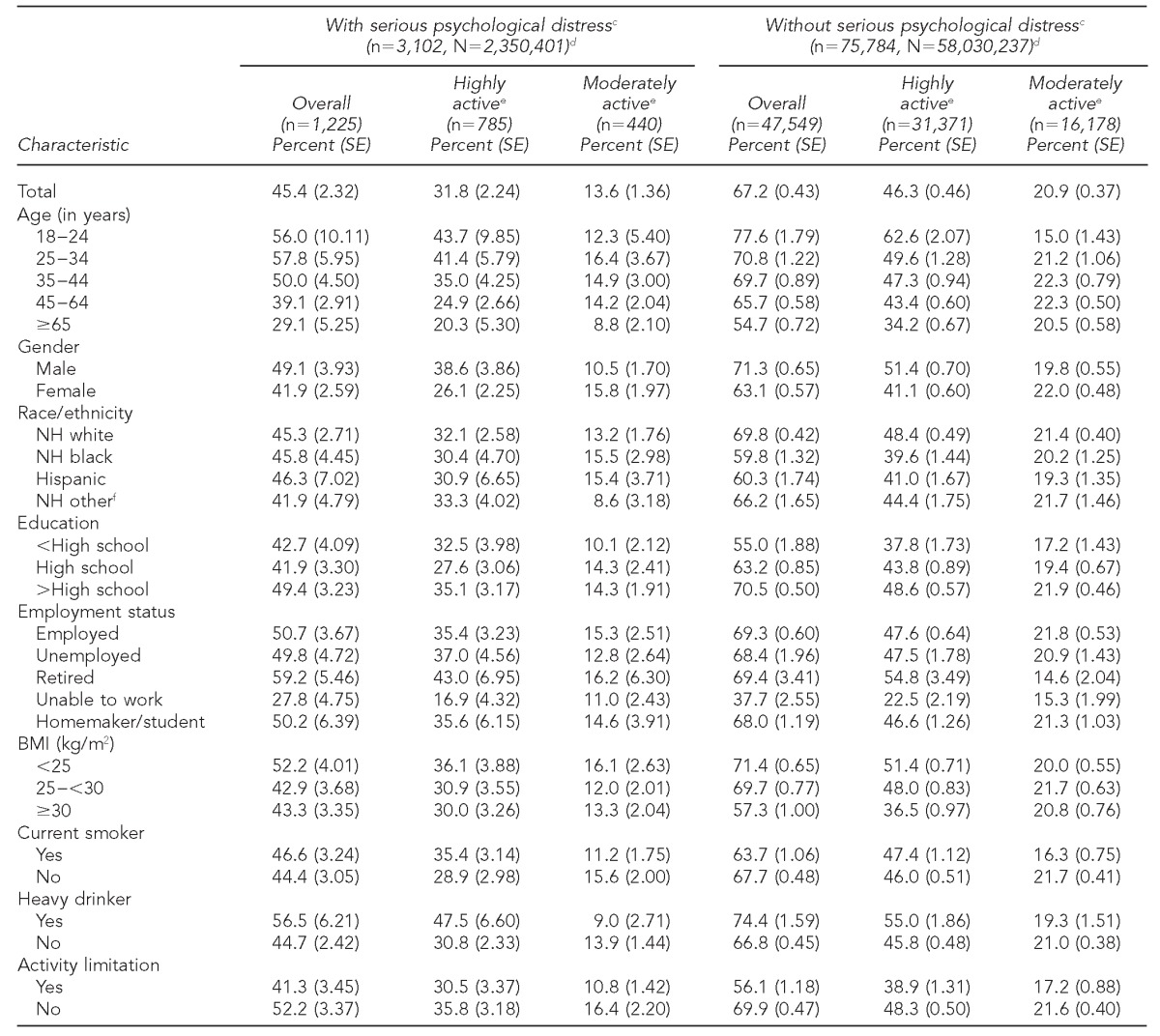
Estimates are age-standardized with the direct method based on the 2000 U.S. population aged ≥18 years.
California, Georgia, Hawaii, Kansas, Massachusetts, Michigan, Mississippi, Missouri, Nebraska, Nevada, South Carolina, Tennessee, Utah, Vermont, Washington, and Wyoming
cBased on the Kessler 6 scale, whereby 4 = all of the time, 3 = most of the time, 2 = some of the time, 1 = a little of the time, and 0 = none of the time. A total K6 score of ≥13 indicates serious psychological distress and <13 indicates no serious psychological distress.
dn = unweighted sample size, and N = weighted U.S. adult population aged ≥18 years
eHighly active = ≥301 weekly minutes of moderate-intensity and/or vigorous-intensity physical activity and moderately active = 150–300 weekly minutes of moderate-intensity and/or vigorous-intensity physical activity.
fIncludes American Indian/Alaska Native, Asian, and Native Hawaiian/other Pacific Islander
HHS = U.S. Department of Health and Human Services
BRFSS = Behavioral Risk Factor Surveillance System
SE = standard error
NH = non-Hispanic
BMI = body mass index
kg/m2 = kilograms per meter squared
As shown in Table 2, the unadjusted PR for adults with SPD who met current public health recommendations for PA compared with those without SPD was 0.68 (95% CI 0.62, 0.74). This PR decreased to 0.84 (95% CI 0.77, 0.91) after adjusting for sociodemographic variables, BMI, smoking status, and heavy drinking, and was attenuated but remained significant after further adjusting for PA limitations (0.88, 95% CI 0.81, 0.96).
Table 2.
Unadjusted and adjusted prevalence ratios for meeting 2008 HHS physical activity recommendations for U.S. adults with serious psychological distress: 16 states,a BRFSS, 2009
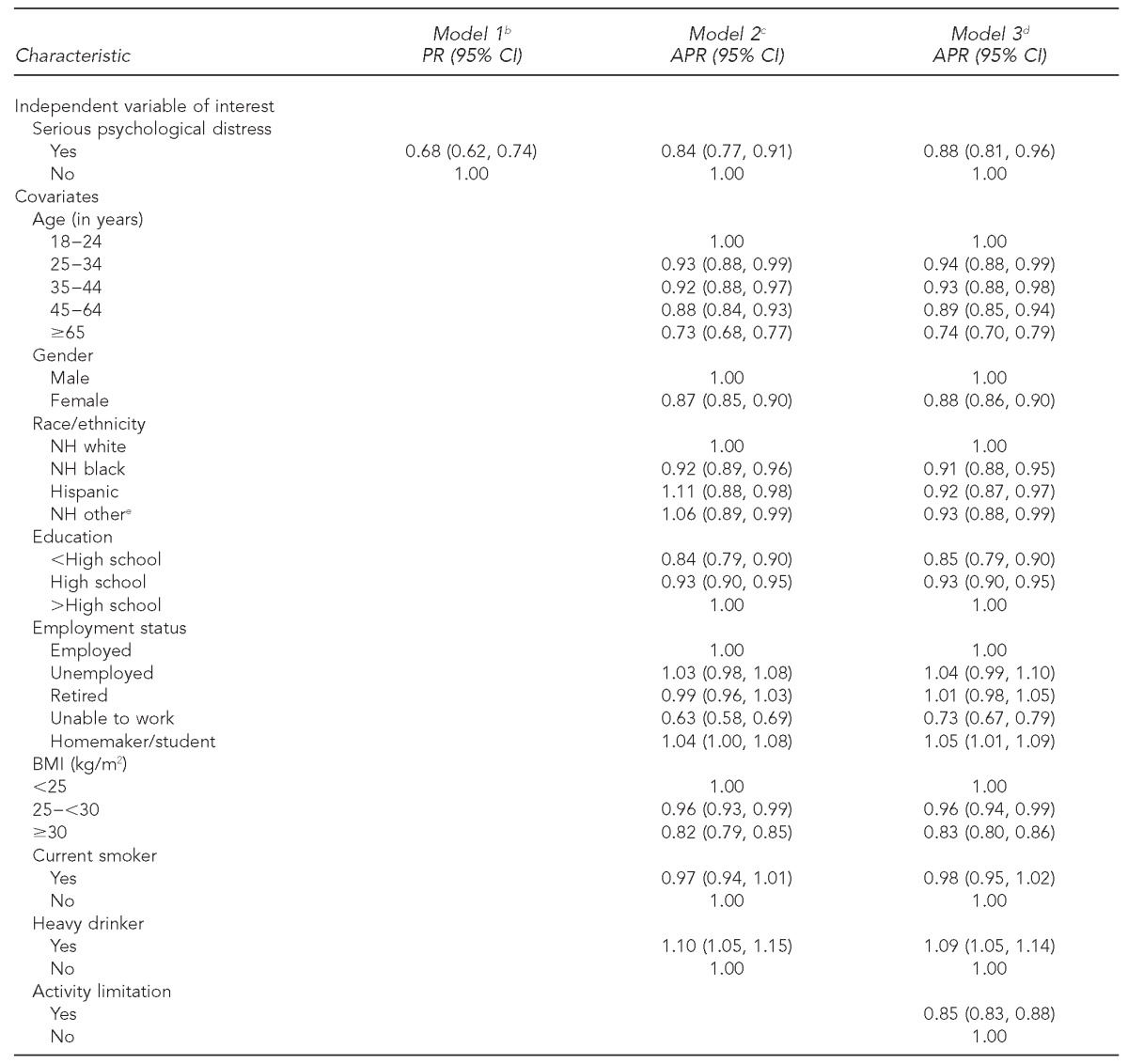
California, Georgia, Hawaii, Kansas, Massachusetts, Michigan, Mississippi, Missouri, Nebraska, Nevada, South Carolina, Tennessee, Utah, Vermont, Washington, and Wyoming
bModel 1 was unadjusted.
cModel 2 was adjusted for age, gender, race/ethnicity, education, employment status, body mass index, current smoking, and heavy drinking.
dModel 3 was adjusted for variables in model 2 and physical activity limitations.
eIncludes American Indian/Alaska Native, Asian, and Native Hawaiian/other Pacific Islander.
HHS = U.S. Department of Health and Human Services
BRFSS = Behavioral Risk Factor Surveillance System
PR = prevalence ratio
CI = confidence interval
APR = adjusted prevalence ratio
NH = non-Hispanic
BMI = body mass index
kg/m2 = kilograms per meter squared
DISCUSSION
At present, there is limited information on the PA patterns of community-dwelling adults with SPD. We found that 3.9% of adults ≥18 years of age were classified as experiencing SPD in the past 30 days. This percentage is comparable with other U.S. estimates reported by SAMHSA that ranged from 3.1% in the NHIS to 4.8% in the MEPS.3 We found that 45.4% of adults with SPD were physically active in accordance with the HHS PA guidelines23 compared with 67.2% of adults without SPD (p<0.0001).
The gap in PA at recommended levels between adults with and without SPD is substantial. Coupled with the fact that adults with SPD were also significantly more likely to be physically inactive than adults without distress (33.2% vs. 11.0%, p<0.0001), it is not surprising that people with poor mental health are at increased risk for adverse health outcomes, premature mortality, and an impaired quality of life.5,6 Our findings are also consistent with those of other researchers who have reported lower levels of PA among adults with comorbid psychological distress and chronic conditions and disabilities.10,41,42 Shih et al. reported that, among women with arthritis, those with frequent anxiety/depression had a significantly higher prevalence of physical inactivity than those without this comorbidity.42 Our findings and those of other researchers highlight the need to assess the PA status of adults at increased risk for suboptimal levels of PA, such as older adults and those with impaired mental health, chronic physical conditions, and functional limitations.
The relationship between mental health and PA is well known; however, the mechanisms of action that underlie this relationship remain poorly understood.43 Researchers have conducted several randomized controlled trials (RCTs) to further elucidate the effect that PA and its optimal prescription (i.e., frequency, intensity, and duration) may have in the treatment of depression.44–47 A recent Cochrane review summarized the findings of 30 RCTs to determine the effectiveness of exercise in the treatment of depression. For 28 RCTs, exercise had a moderate clinical effect on depression symptoms. However, when the review was limited to four methodologically robust RCTs, exercise had a much smaller clinical effect.48 Further RCTs are needed to gain a greater degree of confidence in the effect of exercise on depression, other mental disorders, and psychological distress, as well as to assist in the prescription of evidence-based PA.
While a complete understanding of these mechanisms has yet to be achieved, mental health-care professionals and other health-care professionals have incorporated PA into their clinical protocols because of its demonstrated effectiveness in improving mood disorders and overall health.17,18,22,25,26,49 For example, APA's17 clinical guidelines include prescribed and -monitored PA as an initial treatment protocol for patients with a mild depressive disorder or as an adjunct treatment for patients with depression (i.e., regardless of severity), provided there are no contraindications to PA. Notably, the percentage of U.S. adults ≥18 years of age who had received physician counseling to begin or continue to do exercise or PA increased from 22.6% in 2000 to 32.4% in 2010.50 These increases occurred for every age, race/ethnicity, and health condition group examined. However, while physical health conditions (e.g., hypertension, cardiovascular disease, and cancer) were examined, mental health conditions were not. Nevertheless, given that SPD and mental disorders are often comorbid with chronic physical conditions, the increasing trend in receipt of physician counseling for exercise may have health benefits for adults with these conditions as well, provided patients either initiate or continue PA as counseled.
The U.S. Preventive Services Task Force recommends depression screening among adults in primary care settings based upon evidence of improved health outcomes “when staff-assisted depression care supports are in place to assure accurate diagnosis, effective treatment, and follow-up.”51 To ensure optimal implementation and functioning of these depression care support systems, the Community Preventive Services Task Force recommends the use of collaborative care models, “a multicomponent, healthcare system-level intervention that uses case managers to link primary care providers, patients, and mental health specialists.”52 Adults with poor mental health may have more difficulty with the initiation or maintenance of PA due to the symptoms of their illness (e.g., feeling hopeless, like everything is an effort, and depressed) and, possibly, other factors associated with lower levels of PA (e.g., specific sociodemographic characteristics, BMI, and activity limitations).16,42,53 Thus, the incorporation of an assessment for PA followed by appropriate intervention and support to initiate, maintain, or increase PA into clinical protocols may also improve health outcomes for patients.16,23 For those identified with mental illness, it may prevent the progression of mental illness or assist with disease remission and its maintenance.17,19,22
Strengths and limitations
Our study had several strengths. First, we operationalized SPD using a standard, valid, and reliable scale developed for use in general population surveys.2,31,32 Second, we provided the first known baseline data on the PA patterns of adults with and without SPD, and whether adults with SPD were physically active at levels consistent with the 2008 guidelines.23 Third, the use of BRFSS data will facilitate the monitoring of changes in PA levels of adults with SPD. Finally, we examined variables that may confound the association between SPD and PA at levels that are consistent with current recommendations.
This study was also subject to several limitations. The 2009 BRFSS was a landline household telephone survey of the community-dwelling adult population. Thus, it is not representative of cellular-only households or of institutionalized populations, and is subject to self-reported biases. The effect of these limitations on our findings is not known, but they may have resulted in underestimates of SPD and either under- or overestimates of PA. However, researchers54 have demonstrated that the BRFSS provides reliable and valid data, particularly for our key study variables (i.e., SPD and PA).32,34
Additionally, we were unable to assess the muscle-strengthening activities component of the 2008 guidelines, and we lacked data on contraindications to PA. Furthermore, only 16 of the 50 states used the optional BRFSS MIS module; therefore, our findings are not representative of the nation's adult community-dwelling population. Finally, the BRFSS is a cross-sectional study; thus, causation cannot be inferred. For example, adults who have SPD may be more likely to stop being physically active, maintain their current level of activity, or be unable to initiate a physically active lifestyle. Conversely, adults who are physically inactive or active at levels below current public health recommendations may be more likely to develop symptoms of psychological distress or have an increased level of symptom severity.
CONCLUSIONS
A substantial disparity exists in the level of PA among adults with and without SPD. Evidence-based PA interventions that target adults with SPD, particularly those identified to be at increased risk of suboptimal levels of PA, are needed. Additional research is needed to identify and examine factors that increase the likelihood of PA among people with impaired mental health. Given the health benefits of PA, mental health-care and other health-care professionals should encourage patients to initiate, maintain, or increase PA, provided there are no contraindications to PA. Public health strategies that increase PA at a population level may improve mental health in people with subclinical levels of psychological distress, diminish the prevalence of SPD in the general population, and decrease the incidence of impaired mental health.
Footnotes
The authors thank the state Behavioral Risk Factor Surveillance System (BRFSS) coordinators for their participation in data collection for this analysis and the Division of Behavioral Surveillance staff for their assistance in developing the database.
This article was presented at the 139th American Public Health Association Annual Meeting, October 29–November 2, 2011, in Washington, D.C. The BRFSS has a surveillance exemption from Institutional Review Board (IRB) review at the Centers for Disease Control and Prevention (CDC). Participating states are subject to state-specific IRB requirements. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of CDC.
REFERENCES
- 1.Andrews G, Slade T. Interpreting scores on the Kessler Psychological Distress Scale (K10) Aust N Z J Public Health. 2001;25:494–7. doi: 10.1111/j.1467-842x.2001.tb00310.x. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32:959–76. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 3.Hedden S, Gfroerer J, Barker P, Smith S, Pemberton MR, Saavedra LM, et al. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2012. Comparison of NSDUH mental health data and methods with other data sources. CBHSQ Data Review, Center for Behavioral Health Statistics and Quality. [PubMed] [Google Scholar]
- 4.Druss BG, Hwang I, Petukhova M, Sampson NA, Wang PS, Kessler RC. Impairment in role functioning in mental and chronic medical disorders in the United States: results from the National Comorbidity Survey Replication. Mol Psychiatry. 2009;14:728–37. doi: 10.1038/mp.2008.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication [published erratum apears in Arch Gen Psychiatry 2005;62:709] Arch Gen Psychiatry. 2005;62:617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. 2006;3:A42. [PMC free article] [PubMed] [Google Scholar]
- 7.Pratt LA. Serious psychological distress, as measured by the K6, and mortality. Ann Epidemiol. 2009;19:202–9. doi: 10.1016/j.annepidem.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 8.McGuire LC, Strine TW, Vachirasudlekha S, Anderson LA, Berry JT, Mokdad AH. Modifiable characteristics of a healthy lifestyle and chronic health conditions in older adults with or without serious psychological distress, 2007 Behavioral Risk Factor Surveillance System. Int J Public Health. 2009;54(Suppl 1):84–93. doi: 10.1007/s00038-009-0011-4. [DOI] [PubMed] [Google Scholar]
- 9.Dube SR, Caraballo RS, Dhingra SS, Pearson WS, McClave AK, Strine TW, et al. The relationship between smoking status and serious psychological distress: findings from the 2007 Behavioral Risk Factor Surveillance System. Int J Public Health. 2009;54(Suppl 1):68–74. doi: 10.1007/s00038-009-0009-y. [DOI] [PubMed] [Google Scholar]
- 10.Okoro CA, Strine TW, Balluz LS, Crews JE, Dhingra S, Berry JT, et al. Serious psychological distress among adults with and without disabilities. Int J Public Health. 2009;54(Suppl 1):52–60. doi: 10.1007/s00038-009-0077-z. [DOI] [PubMed] [Google Scholar]
- 11.Substance Abuse and Mental Health Services Administration (US) Mental health, United States, 2008. HHS publication no. SMA 10-4590. Rockville (MD): Department of Health and Human Services (US); 2010. [Google Scholar]
- 12.Mark TL, Levit KR, Coffey RM, McKusick DR, Harwood HJ, King EC, et al. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2007. National expenditures for mental health services and substance abuse treatment, 1993–2003. SAMHSA publication no. SMA 07-4227. [Google Scholar]
- 13.Goetzel RZ, Hawkins K, Ozminkowski RJ, Wang S. The health and productivity cost burden of the “top 10” physical and mental health conditions affecting six large U.S. employers in 1999. J Occup Environ Med. 2003;45:5–14. doi: 10.1097/00043764-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Insel TR. Assessing the economic costs of serious mental illness. Am J Psychiatry. 2008;165:663–5. doi: 10.1176/appi.ajp.2008.08030366. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention (US) The guide to community preventive services: improving mental health and addressing mental illness [cited 2012 Jun 3] Available from: URL: http://www.thecommunityguide.org/mentalhealth/index.html.
- 16.Physical Activity Guidelines Advisory Committee report, 2008. To the Secretary of Health and Human Services. Part A: executive summary. Nutr Rev. 2009;67:114–20. doi: 10.1111/j.1753-4887.2008.00136.x. [DOI] [PubMed] [Google Scholar]
- 17.American Psychiatric Association. Compendium 2006. Arlington (VA): American Psychiatric Association; 2006. American Psychiatric Association practice guidelines for the treatment of psychiatric disorders. Also available from: URL: http://catdir.loc.gov/catdir/toc/ecip069/2006006928.html [cited 2013 Aug 27] [Google Scholar]
- 18.American College of Sports Medicine and American Medical Association. Exercise is Medicine® [cited 2012 Jun 3] Available from: URL: http://exerciseismedicine.org.
- 19.Trangle M, Dieperink B, Gabert T, Haight B, Lindvall B, Mitchell J, et al. Major depression in adults in primary care. 13th ed. Bloomington (MN): Institute for Clinical Systems Improvement; 2010. [Google Scholar]
- 20.Centers for Disease Control and Prevention (US) The guide to clinical preventive services [cited 2013 Feb 18] Available from: URL: http://www.thecommunityguide.org/about/guide.html.
- 21.World Health Organization. Global recommendations on physical activity for health. Geneva: WHO; 2010. [PubMed] [Google Scholar]
- 22.American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder. 3rd ed. Arlington (VA): American Psychiatric Association; 2010. [Google Scholar]
- 23.Department of Health and Human Services (US) 2008 physical activity guidelines for Americans: be active, healthy, and happy! Rockville (MD): HHS; 2008. [Google Scholar]
- 24.Fochtmann LJ, Gelenberg AJ. 2nd ed. Arlington (VA): American Psychiatric Publishing, Inc.; 2000. APA practice guidelines. Guideline watch: practice guideline for the treatment of patients with major depressive disorder. [Google Scholar]
- 25.Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1435–45. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- 26.National Institute for Health and Care Excellence. Depression: the treatment and management of depression in adults (update) United Kingdom: National Institute for Health and Care Excellence; 2009. Also available from: URL: http://www.nice.org.uk/guidance/CG90 [cited 2013 May 7] [Google Scholar]
- 27.Centers for Disease Control and Prevention (US) Behavioral Risk Factor Surveillance System: BRFSS 2009 Survey data and documentation [cited 2013 Nov 7] Available from: URL: http://www.cdc.gov/brfss/annual_2009.htm.
- 28.American Psychiatric Association. Arlington (VA): American Psychiatric Publishing, Inc.; 2000. Diagnostic and statistical manual of mental disorders, 4th edition, text revision (DSM-IV-TR) [Google Scholar]
- 29.Kessler RC, Ustun TB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) composite international diagnostic interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kessler RC, Green JG, Gruber MJ, Sampson NA, Bromet E, Cuitan M, et al. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res. 2010;19(Suppl 1):4–22. doi: 10.1002/mpr.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cairney J, Veldhuizen S, Wade TJ, Kurdyak P, Streiner DL. Evaluation of 2 measures of psychological distress as screeners for depression in the general population. Can J Psychiatry. 2007;52:111–20. doi: 10.1177/070674370705200209. [DOI] [PubMed] [Google Scholar]
- 32.Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60:184–9. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 33.Substance Abuse and Mental Health Services Administration (US) Results from the 2007 National Survey on Drug Use and Health (NSDUH): national findings. Rockville (MD): SAMHSA; 2008. [Google Scholar]
- 34.Strath SJ, Bassett DR, Jr, Ham SA, Swartz AM. Assessment of physical activity by telephone interview versus objective monitoring. Med Sci Sports Exerc. 2003;35:2112–8. doi: 10.1249/01.MSS.0000099091.38917.76. [DOI] [PubMed] [Google Scholar]
- 35.Goodwin RD. Association between physical activity and mental disorders among adults in the United States. Prev Med. 2003;36:698–703. doi: 10.1016/s0091-7435(03)00042-2. [DOI] [PubMed] [Google Scholar]
- 36.Harris AH, Cronkite R, Moos R. Physical activity, exercise coping, and depression in a 10-year cohort study of depressed patients. J Affect Disord. 2006;93:79–85. doi: 10.1016/j.jad.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 37.Wise LA, Adams-Campbell LL, Palmer JR, Rosenberg L. Leisure time physical activity in relation to depressive symptoms in the Black Women's Health Study. Ann Behav Med. 2006;32:68–76. doi: 10.1207/s15324796abm3201_8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.SAS Institute, Inc. SAS®: Version 9.2 for Windows. Cary (NC): SAS Institute, Inc.; 2008. [Google Scholar]
- 39.Research Triangle Institute. Research Triangle Park (NC): Research Triangle Institute; 2008. SUDAAN®: Release 10.0. [Google Scholar]
- 40.Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol. 2010;171:618–23. doi: 10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- 41.Strine TW, Kobau R, Chapman DP, Thurman DJ, Price P, Balluz LS. Psychological distress, comorbidities, and health behaviors among U.S. adults with seizures: results from the 2002 National Health Interview Survey. Epilepsia. 2005;46:1133–9. doi: 10.1111/j.1528-1167.2005.01605.x. [DOI] [PubMed] [Google Scholar]
- 42.Shih M, Hootman JM, Kruger J, Helmick CG. Physical activity in men and women with arthritis: National Health Interview Survey, 2002. Am J Prev Med. 2006;30:385–93. doi: 10.1016/j.amepre.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 43.Blake H. Physical activity and exercise in the treatment of depression. Front Psychiatry. 2012;3:106. doi: 10.3389/fpsyt.2012.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Blake H, Mo P, Malik S, Thomas S. How effective are physical activity interventions for alleviating depressive symptoms in older people? A systematic review. Clin Rehabil. 2009;23:873–87. doi: 10.1177/0269215509337449. [DOI] [PubMed] [Google Scholar]
- 45.Chalder M, Wiles NJ, Campbell J, Hollinghurst SP, Haase AM, Taylor AH, et al. Facilitated physical activity as a treatment for depressed adults: randomised controlled trial. BMJ. 2012;344:e2758. doi: 10.1136/bmj.e2758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Trivedi MH, Greer TL, Grannemann BD, Church TS, Galper DI, Sunderajan P, et al. TREAD: TReatment with Exercise Augmentation for Depression: study rationale and design. Clin Trials. 2006;3:291–305. doi: 10.1191/1740774506cn151oa. [DOI] [PubMed] [Google Scholar]
- 47.Trivedi MH, Greer TL, Church TS, Carmody TJ, Grannemann BD, Galper DI, et al. Exercise as an augmentation treatment for nonremitted major depressive disorder: a randomized, parallel dose comparison. J Clin Psychiatry. 2011;72:677–84. doi: 10.4088/JCP.10m06743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rimer J, Dwan K, Lawlor DA, Greig CA, McMurdo M, Morley W, et al. Exercise for depression. Cochrane Database Syst Rev. 2012;7:CD004366. doi: 10.1002/14651858.CD004366.pub5. [DOI] [PubMed] [Google Scholar]
- 49.Dietrich AJ, Oxman TE, Williams JW, Jr, Schulberg HC, Bruce ML, Lee PW, et al. Re-engineering systems for the treatment of depression in primary care: cluster randomised controlled trial. BMJ. 2004;329:602. doi: 10.1136/bmj.38219.481250.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barnes PM, Schoenborn CA. Trends in adults receiving a recommendation for exercise or other physical activity from a physician or other health professional. NCHS Data Brief. 2012;(86):1–8. [PubMed] [Google Scholar]
- 51.O'Connor EA, Whitlock EP, Bell TL, Gaynes BN. Screening for depression in adult patients in primary care settings: a systematic evidence review. Ann Intern Med. 2009;151:793–803. doi: 10.7326/0003-4819-151-11-200912010-00007. [DOI] [PubMed] [Google Scholar]
- 52.Thota AB, Sipe TA, Byard GJ, Zometa CS, Hahn RA, McKnight-Eily LR, et al. Collaborative care to improve the management of depressive disorders: a community guide systematic review and meta-analysis. Am J Prev Med. 2012;42:525–38. doi: 10.1016/j.amepre.2012.01.019. [DOI] [PubMed] [Google Scholar]
- 53.Strine TW, Chapman DP, Kobau R, Balluz L. Associations of self-reported anxiety symptoms with health-related quality of life and health behaviors. Soc Psychiatry Psychiatr Epidemiol. 2005;40:432–8. doi: 10.1007/s00127-005-0914-1. [DOI] [PubMed] [Google Scholar]
- 54.Li C, Balluz LS, Ford ES, Okoro CA, Zhao G, Pierannunzi C. A comparison of prevalence estimates for selected health indicators and chronic diseases or conditions from the Behavioral Risk Factor Surveillance System, the National Health Interview Survey, and the National Health and Nutrition Examination Survey, 2007–2008. Prev Med. 2012;54:381–7. doi: 10.1016/j.ypmed.2012.04.003. [DOI] [PubMed] [Google Scholar]


