Abstract
Paratesticular swellings pose a diagnostic dilemma due to concerns over malignancy. We present a case of paratesticular swelling in a 13-year-old boy as a result of Dirofilaria immitis infection. The boy presented with a 2-month history of right testicular discomfort associated with an irregular mass within the scrotum.
Background
Human subcutaneous dirofilariasis (HSD) is a zoonotic condition caused by infection by nematodes belonging to the Dirofilaria family.1 2 These worms are present in a variety of animals, with canines being the most common host.2 Although the current epidemiological studies indicate that human dirofilariasis is on the rise worldwide, its incidence is still extremely rare in the UK.1 We present a case in a child of paratesticular subcutaneous dirofilariasis that was initially suspected to be a paratesticular malignancy. We believe that this presentation in a paediatric patient is the first of its kind in the UK.
Case presentation
A 13-year-old boy presented with a 2-month history of right testicular discomfort associated with an irregular mass within the scrotum. There was no history of note and he was otherwise asymptomatic. On examination, the right testicle was hard, irregular and non-tender raising concerns of malignancy. The left testicle was normal.
Investigations, differential diagnosis and treatment
Ultrasound scan of the testicles demonstrated a generalised enlargement of the right epididymis, maximal at the tail, with a localised mass measuring 21×13×11 mm. Testicular tissue was normal. Differential diagnosis included chronic epididymitis although a malignant process could not be excluded. Tumour markers, α-fetoprotein and βHCG, were within normal range. Following discussion at the oncology multidisciplinary team (MDT) meeting, an infective process was thought to be the most likely diagnosis and the patient was started on oral co-amoxiclav (figure 1).
Figure 1.
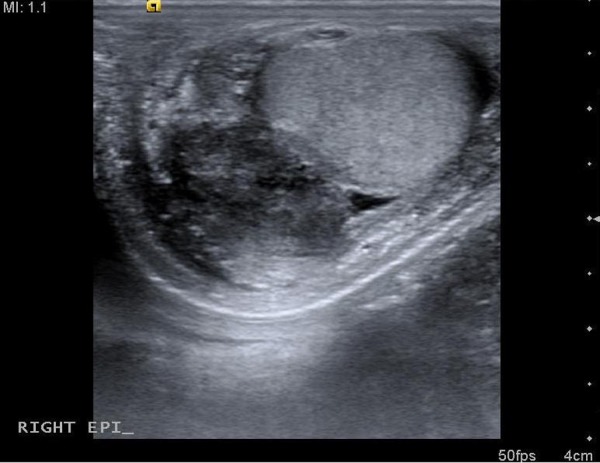
Ultrasound scan of the right testes, showing the paratesticular lesion.
On repeat scan at 2 weeks, the epididymal lesion had increased in size to 40 mm and contained cystic and solid components increasing the concern of malignancy. Further discussion at the oncology MDT resulted in the decision to proceed with right orchidectomy.
Histological examination demonstrated no evidence of malignancy; however, a worm was seen within the mass. To identify the species of worm and plan further management, specialist opinion was sought. The appearance was reported to be that of a sterile male adult worm with typical Dirofilaria features giving a diagnosis of subcutaneous dirofilariasis in the epididymis of the right testicle. The patient had a normal eosinophil count and had no other evidence of systemic infection; therefore, no further treatment was required (figure 2).
Figure 2.
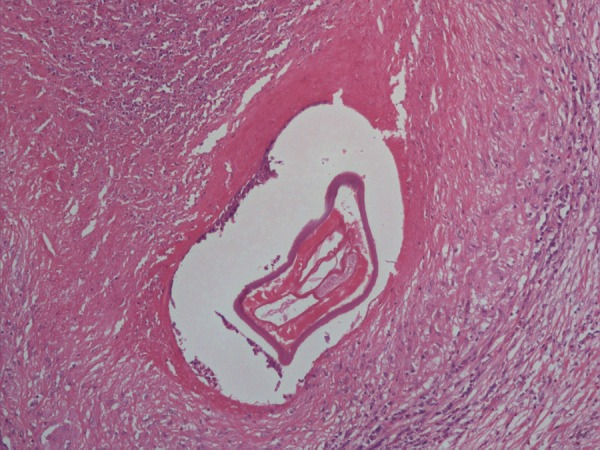
Histology demonstrating Dirofilaria immitis within the epididymis.
Outcome and follow-up
At an 18-month follow-up, the patient remained well and a testicular prosthesis was inserted.
Discussion
Dirofilariasis in humans is caused by members of the Dirofilaria family—Dirofilaria immitis and Dirofilaria repens. Also known as heartworm, D immitis is a parasitic worm responsible for causing cardiopulmonary dirofilariasis in dogs and cats, and pulmonary dirofilariasis in humans. D repens is characterised by subcutaneous nodules in canines and felines, and is associated with subcutaneous and ocular nodules when present in humans.1 While D immitis is predominantly found in America and Australia, D repens is common in Southern Europe and the Indian subcontinent.2 This is a vector-borne disease transmitted by mosquitos.3 Its incidence has increased due to transportation of Dirofilaria positive pets, evolution of new vectors and climatic changes secondary to global warming.2 Epidemiological surveys have shown the spread of both worm species to areas previously free of Dirofilaria nematodes.3
Worms of the genus Dilofilaria are elongated, thin and are identified by their thick laminated cuticle, broad lateral ends and large muscle cells. The female worms are larger than the males, with D immitis females measuring 25–31 cm compared with their male counterparts that are 12–20 cm long. D immitis can be differentiated from D repens by the absence of ridges and transverse striation.4 D immitis also causes microfilaraemia in humans, requiring anthelminthic medication.
Human dirofilariasis was first reported in 1887 when de Magalhaes discovered filarial worms in the left ventricle of a child in Rio de Janeiro.5 The transmission of D immitis most commonly causes human pulmonary dirofilariasis producing pulmonary nodules often misidentified as malignant tumours or granulomatous disease.6 Symptomatic cases commonly present with cough, fever and haemoptysis although it is most often asymptomatic. The disease is confirmed by the presence of fragments of D immitis on histological examination.
D repens manifests as subcutaneous and ocular nodules that grow over a period of weeks or months when transmitted to humans. The nodules, found in the scrotum, abdomen and cheeks, have a firm, elastic consistency and are associated with erythema. Although the highest incidence of the infection occurs in individuals aged 40–49 years, infections in patients of all ages have been described, notably in Sri Lanka where over one-third of the reported cases have occurred in children under the age of 10.2 Simple extraction of the worm or surgical excision of the dilofilarial lesion is often the treatment of choice. Dirofiliriasis is exceptionally rare in the UK; where present, D repens is more common than D immitis.
Subcutaneous dilofilariasis presenting in the testes are rare, with only a few cases being described of dirofilariasis in the scrotum, epididymis and the spermatic cord.2 7–13 These nodules can be mistaken for scrotal malignancies and can result in extensive operations that are unnecessary.10 Among the cases reported, the majority were from endemic areas with D repens commonly attributed to the occurrence of the disease.10 12 13 However, a small number of cases of subcutaneous dirofilarial nodules have been reported in the literature with D immitis as the causal organism, with one case describing a scrotal nodule.11 14 Theis et al described the case of a 28-year-old man in whom a 3 cm nodule was detected requiring orchidectomy. The patient was from Nevada, California, which is a highly enzootic area for D immitis.11 The boy in our case had a similar infection, which may be caused by the increased movement of D immitis positive pets across Europe, as reviewed by Simon et al.2
Anthelmintic drugs are not commonly used in the treatment of paratesticular dirofilariasis as the diagnosis is often made following histological examination of the excised nodule. However, if secondary nodules are detected, a trial of ivermectin and diethylcarbamazine may be carried out. However, in rare cases where additional worms or surgically inaccessible lesions are identified and pharmacological intervention is thought to be necessary, a combination of doxycycline and ivermectin may be considered.15 Pharmacological intervention should be carried out before surgery if there are risk factors suggesting the possibility of systemic dirofilariasis. The treatment for isolated disease is surgical resection, including orchidectomy in paratesticular disease as in the case described.
Learning points.
Consider nematode infection in patients presenting with gradual onset testicular swelling.
A thorough travel and pet history is essential in these patients.
Most human Dirofilarial infections can be managed definitively by surgical excision
Acknowledgments
The authors would like to thank Dr Gauri Batra, paediatric pathologist, who was involved in the institutional management of the patient at the Royal Manchester Children's Hospital. The authors would also like to thank Dr Wendi Bailey, pathologist, from the Liverpool School of Tropical Medicine who played a role in the identification of the parasite.
Footnotes
Contributors: JK wrote up the case. SJW was involved in the surgical management of the patient. TO was involved in the identification of the parasite and management of patient. RJC was involved in the surgical management of the patient.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Simón F, López-Belmonte J, Marcos-Atxutegi C, et al. What is happening outside North America regarding human dirofilariasis? Vet Parasitol 2005;133:181–9 [DOI] [PubMed] [Google Scholar]
- 2.Simon F, Siles-Lucas M, Morchon R, et al. Human and animal dirofilariasis: the emergence of a zoonotic mosaic. Clin Microbiol Rev 2012;25:507–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foissac M, Million M, Mary C, et al. Subcutaneous infection with Dirofilaria immitis nematode in human, France. Emerg Infect Dis 2013;19:171–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sathyan P, Manikandan P, Bhaskar M, et al. Subtenons infection by Dirofilaria repens. Indian J Med Microbiol 2006;24:61–2 [DOI] [PubMed] [Google Scholar]
- 5.Miyoshi T, Tsubouchi H, Iwasaki A, et al. Human pulmonary dirofilariasis: a case report and review of the recent Japanese literature. Respirology 2006;11:343–7 [DOI] [PubMed] [Google Scholar]
- 6.Bielawski BC, Harrington D, Joseph E. A solitary pulmonary nodule with zoonotic implications. Chest 2001;119:1250–2 [DOI] [PubMed] [Google Scholar]
- 7.Pampiglione S, Elek G, Palfi P, et al. Human Dirofilaria repens infection in Hungary: a case in the spermatic cord and a review of the literature. Acta Vet Hung 1999;47:77–83 [DOI] [PubMed] [Google Scholar]
- 8.Soussi A, Farah Klibi F, Zermani R, et al. [Subcutaneous dirofilariasis due to Dirofilaria repens in Tunisia: a case involving the scrotum]. Med Trop (Mars) 2004;64:375–8 [PubMed] [Google Scholar]
- 9.Singh R, Shwetha JV, Samantaray JC, et al. Dirofilariasis: a rare case report. Indian J Med Microbiol 2010;28:75–7 [DOI] [PubMed] [Google Scholar]
- 10.Fleck R, Kurz W, Quade B, et al. Human dirofilariasis due to Dirofilaria repens mimicking a scrotal tumor. Urology 2009;73:209 e1–3 [DOI] [PubMed] [Google Scholar]
- 11.Theis JH, Gilson A, Simon GE, et al. Case report: unusual location of Dirofilaria immitis in a 28-year-old man necessitates orchiectomy. Am J Trop Med Hyg 2001;64:317–22 [DOI] [PubMed] [Google Scholar]
- 12.Leccia N, Patouraux S, Carpentier X, et al. Pseudo-tumor of the scrotum, a rare clinical presentation of dirofilariasis: a report of two autochtonous cases due to Dirofilaria repens. Pathog Glob Health 2012;106:370–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.D'Amuri A, Senatore SA, Carla TG, et al. Cutaneous dirofilariasis resulting in orchiectomy. J Cutan Pathol 2012;39:304–5 [DOI] [PubMed] [Google Scholar]
- 14.Moorhouse DE. Dirofilaria immitis: a cause of human intra-ocular infection. Infection 1978;6:192–3 [DOI] [PubMed] [Google Scholar]
- 15.Jelinek T, Schulte-Hillen J, Löscher T. Human dirofilariasis. Int J Dermatol 1996;35:872–5 [DOI] [PubMed] [Google Scholar]


