Abstract
This case reports a patient who developed central retinal artery occlusion following spinal surgery in the prone position. When placed in this position, especially as a result of malposition of the head, the patient may develop external compression of the eye which leads to central retinal artery occlusion. Therefore, a special precaution must be given for adequate eye protection during prolonged prone-positioned spine surgery.
Background
This is a case of central retinal artery occlusion (CRAO) following spinal surgery in the prone position. The CRAO can be due to embolus, thrombus or related to trauma or spasm of the artery. Its occurrence as a complication of spine surgery is very infrequent but may have severe consequences. Prevention of this condition through awareness of the risk is critical.
Case presentation
A 22-year-old Chinese man, a university student with no known medical illness, presented with sudden weakness of both his lower limbs. He underwent cervical spinal surgery in the prone position for spinal extradural haematoma under general anaesthesia for 3.5 h. There was close monitoring by the anaesthetist and there was no hypotension recorded during the procedure. Seven to eight hours postoperatively, on fully waking up from the anaesthetic, he reported of severe, central, painless blurring of vision in the right eye.
On examination at the bedside by the on-call team, his visual acuity was counting finger in the affected eye. There was a marked positive relative afferent pupillary defect. The visual field in the affected eye showed a dense central scotoma. The conjunctiva was mildly injected. Otherwise the anterior segment was normal with an intraocular pressure (IOP) of 18 mm Hg OD and 16 mm Hg OS. Hence, no IOP lowering medications were given. Right fundus examination showed a pink optic disc with patchy areas of macular and retinal oedema with a cherry-red spot (figure 1). The left eye was normal with visual acuity of 6/6, N5 and no visual field defect. He weighed 62 kg and was approximately 170 cm tall.
Figure 1.
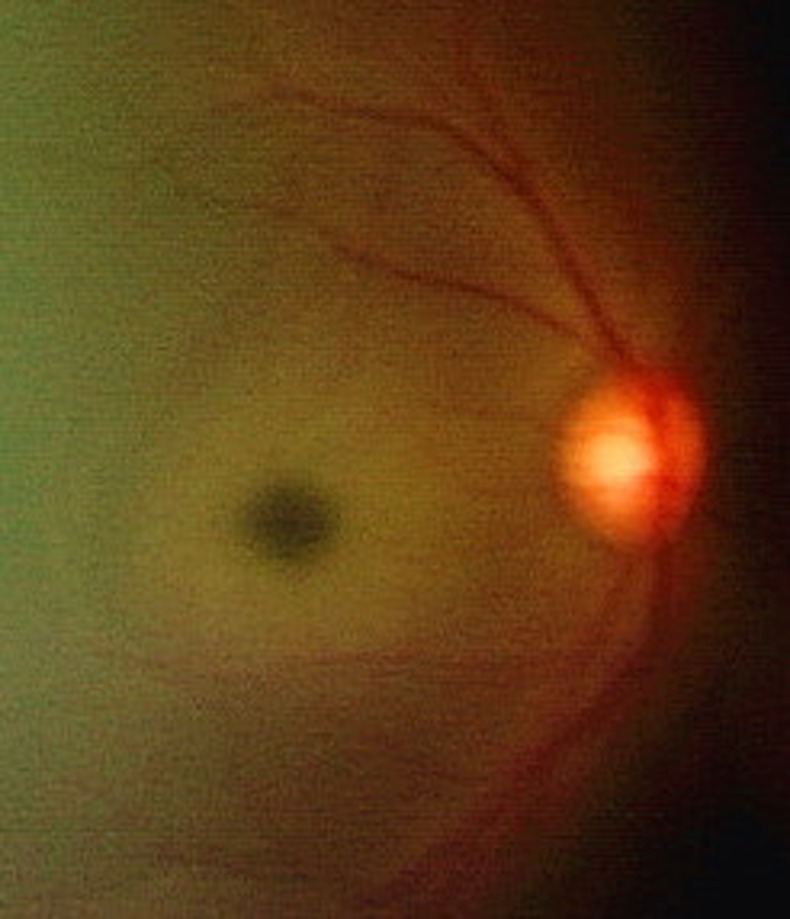
Right fundus photograph taken with a hand-held retinal camera system showed a pink optic disc with areas of macular and retinal oedema with a cherry-red spot. The patient was on complete bed rest postspinal surgery.
Investigations
Fluorescein angiography was performed 6 days later (figure 2) and showed a delay in arm-retinal perfusion time, minimal areas of capillary non-perfusion and late leakage at the macula. Microaneurysms were noted in the periphery(figure 3).
Full blood count was normal.
Blood clotting time studies were not conducted. The patient did not have any symptoms of gum bleeding or other history of hypercoagulopathy.
Serum cholesterol levels were normal.
Figure 2.
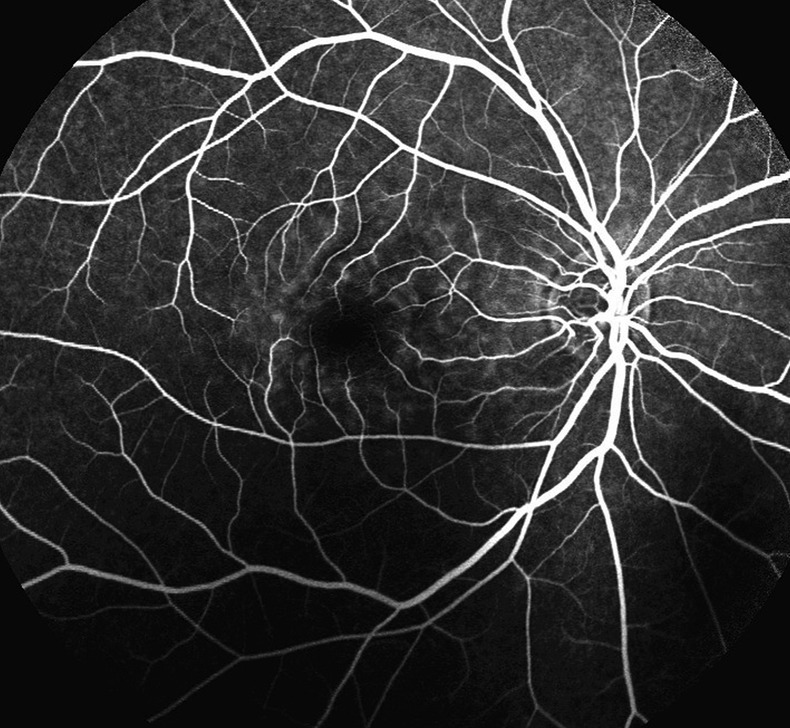
Fluorescein angiography study 6 days after presentation showed late leakage at the right macula.
Figure 3.
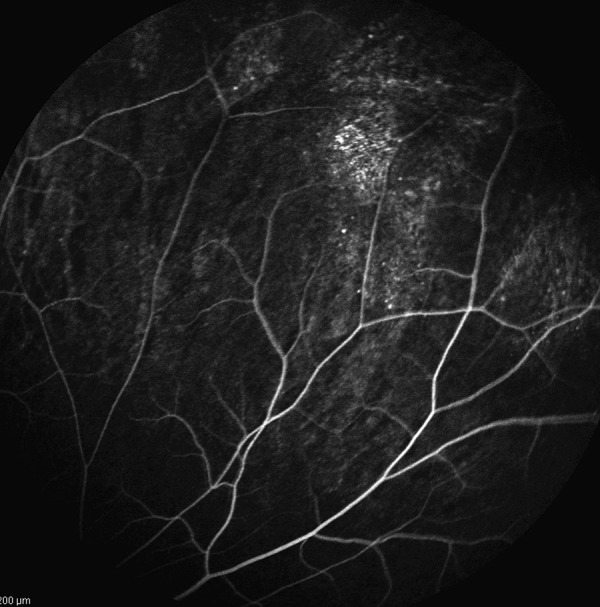
Fluorescein angiography study showed limited peripheral microaneurysms in the right superonasal quadrant.
Differential diagnosis
Ophthalmic artery occlusion
Choroidal infarct
Ischaemic optic neuropathy
Treatment
Ocular massage
Observation
Lifetime follow-up for rubeosis and neovascularisation
Outcome and follow-up
At last follow-up 1 month later, his visual acuity was still counting fingers. Right retinal examination showed a slightly pale disc with evidence of resolving occlusion (figure 4). The anterior segment findings and IOP were normal. There was no neovascularisation seen. The visual field was the same.
Figure 4.
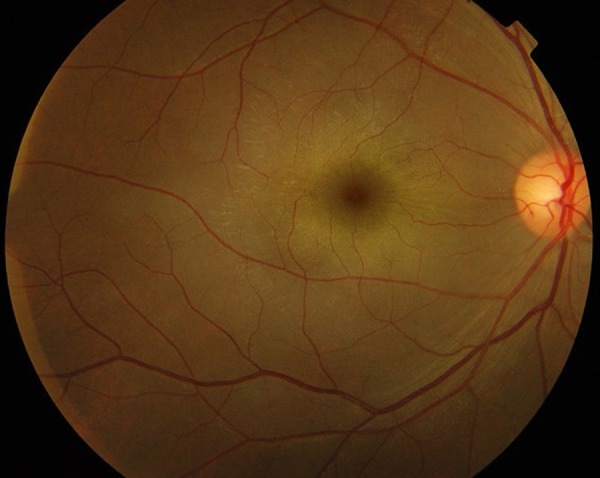
Right fundus photograph taken 1 month later showed persistent macular oedema with retinal striations at the macula and slight disc pallor.
Discussion
Postoperative visual loss occurring after surgery which does not involve the ocular structures occurs with an estimated incidence ranging from 0.001% to 1% depending on the type of surgery.1 Loss of vision after surgery on the back or spine which is usually performed under general anaesthesia in a prone position has gained increasing recognition.2–7 This prone position during general anaesthesia is an important predisposing factor.2 4 5 Prone position alone even in normal awake individuals causes the IOP to increase.2
CRAO is a rare complication of spinal operations. However, there have been several case reports of this. Slocum et al6 were the first to report this problem in a patient who underwent a neurosurgical procedure using a Bailey headrest. He emphasised that the CRAO was caused by the extraocular pressure due to the headrest or because of anaesthetic mask malposition in the presence of hypotension. Kamming and Clarke2 postulated that apart from elevated extraocular and IOP, central venous pressure could have become elevated during the procedure causing further venous compression and congestion in the orbit on the compressed side.
Hollenhorst et al7 mentioned the possibility of CRAO after neurosurgical procedures were performed with a horseshoe-shaped headrest.
In our case, the mechanism of the retinal ischaemia was probably venous congestion and arterial occlusion secondary to external compression on the eye. We also entertained the likelihood of hypotension during the surgery resulting in posterior ischaemic optic neuropathy. However, the cherry-red spot, pink disc in the acute stage and delayed perfusion on fundus fluorescein angiography support a diagnosis of CRAO. The disc pallor seen subsequently is also seen in the long-standing CRAO.
We believe that the patient's head was malpositioned during prone surgery, resulting in inadvertant excessive pressure of the headrest onto the right eye.
Learning points.
A prolonged prone position during spinal surgery under general anaesthesia, especially as a result of the patient malposition, may predispose to external compression of the eye, leading to central retinal artery occlusion.
Central retinal artery occlusion after spine surgery is a sad but avoidable complication of the surgery with significant legal implications.
Surgeons and anaesthetists performing spinal surgery in the prone position must heed every precaution for adequate eye protection during prolonged prone-positioned spine surgery.
Acknowledgments
The authors would like to thank staff of UKM specialist centre and UKM medical centre and our families.
Footnotes
Contributors: All the authors contributed to the writing of the manuscript and the management of the patient.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Warner ME, Warner MA, Garrity JA, et al. The frequency of perioperative vision loss. Anesth Analg 2001;93:1417–21 [DOI] [PubMed] [Google Scholar]
- 2.Kamming D, Clarke S. Postoperative visual loss following prone spine surgery. Br J Anaesth 2005;95:257–60 [DOI] [PubMed] [Google Scholar]
- 3.Delattre O, Thoreux P, Liverneaux P, et al. Spinal surgery and ophthalmic complications: a French survey with review of 17 cases. J Spinal Disord Tech 2007;20:302–7 [DOI] [PubMed] [Google Scholar]
- 4.Roth S, Tung A, Ksiazek S. Visual loss in a prone-positioned spine surgery patient with the head on a foam headrest and goggles covering the eyes: an old complication with a new mechanism. Anesth Analg 2007;104:1185–7 [DOI] [PubMed] [Google Scholar]
- 5.Min-Su C, Jun-Hyuk S. Visual loss in one eye after spinal surgery. Korean J Ophthalmol 2006;20:139–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Slocum HC, O'Neal KC, Allen CR. Neurovascular complications from malposition on the operating table. Surg Gynecol Obstet 1948;86:729–34 [PubMed] [Google Scholar]
- 7.Hollenhorst RW, Svien HJ, Benoit CF. Unilateral blindness occurring during anesthesia for neurosurgical opeartions. Arch Ophthalmol 1954;52:819–30 [DOI] [PubMed] [Google Scholar]


