Abstract
Hepatic tuberculosis as a part of disseminated tuberculosis is seen in 50–80% of cases. Isolated hepatic tuberculosis is very uncommon even in countries with high prevalence of tuberculosis. It can occur as a primary case or due to reactivation of an old tubercular focus. We report a case of a 59-year-old Caucasian woman who presented with persistent right upper quadrant pain and a hepatic lesion on an abdominal CT. She had a history of pulmonary tuberculosis 15 years ago with localised lung tuberculosis treated with lobectomy and antituberculous drugs.
Background
This case report is important as the most of the physicians in the world will encounter at least one patient with a space-occupying lesion of the liver in their entire life. Everyone should include the hepatic TB in the differential diagnosis.
Case presentation
Introduction
Hepatic TB particularly in the absence of miliary TB is rare and represents less than 1% of all cases of TB.1 2 Localised hepatic TB is, in the majority of cases, due to reactivation of old tuberculous foci or, on rare occasions, a result of primary tuberculous involvement of the liver. Liver tuberculoma is rare, with fewer than 100 cases reported in the literature, most of which are secondary to miliary TB.1 Hepatic TB can mimic primary hepatocellular carcinomas, hilar tumours (Klatskin tumours) that can cause biliary obstruction, cholangiocarcinoma, gallbladder carcinoma and liver abscesses. Some patients with hepatic TB present with fever of unknown origin and liver histology shows caseating granulomas (CG). Hepatic TB may also mimic other types of granulomatous liver lesions such as sarcoidosis.3 On the other hand, hepatic biochemical and imaging abnormalities may be encountered in abdominal TB in the absence of liver involvement.
Case report
We present the case of a 59-year-old Caucasian female physician, who presented with persistent right upper quadrant intermittent, non-radiating abdominal pain. She denied any fever, loss of weight, appetite changes or weakness. Clinical examination was normal, her medical history included hepatitis B infection 40 years ago and pulmonary TB 25 years ago. The pulmonary TB treated with anti-TB drugs and right apical pulmonary segmentectomy. The patient also had a cholecystectomy 15 years ago. The initial laboratory findings revealed only an elevated LDH (255 IU/L). The serum tumour markers (α-fetoprotein, carcinoembryonic antigen, CA-19.9, CA-15.3, CA-125) were within normal limits and viral serology showed that only the anti-HBcore/antiHBs were positive. Abdominal ultrasound demonstrated a mass of mixed-echogenicity in the right lobe of the liver. A plain chest radiography revealed no evidence of pulmonary TB and the Mantoux test (PPD) was negative. Subsequent CT scan showed a 2.7 cm hypodense focal lesion in segment VII of the liver (figure 1A). Following IV contrast administration there was moderate enhancement of the lesion in the arterial phase (figure 1B), with contrast wash-out and peripheral capsular enhancement in the portal-vein phase (figure 1C), findings that arose the suspicion of hepatocellular carcinoma. There were no enlarged lymph nodes and there was no evidence of malignancy elsewhere. Although a CT scan-guided biopsy might be helpful in establishing a diagnosis, the patient denied the procedure and elected to treat the mass like a potential malignant tumour and proceed with radical surgical excision. She underwent a diagnostic laparotomy and right lateral segmentomy of the liver. Histology revealed granulomatous inflammation (figures 2A,B) with Langhans giant cells (figure 2C) suggesting mycobacterial infection.
Figure 1.
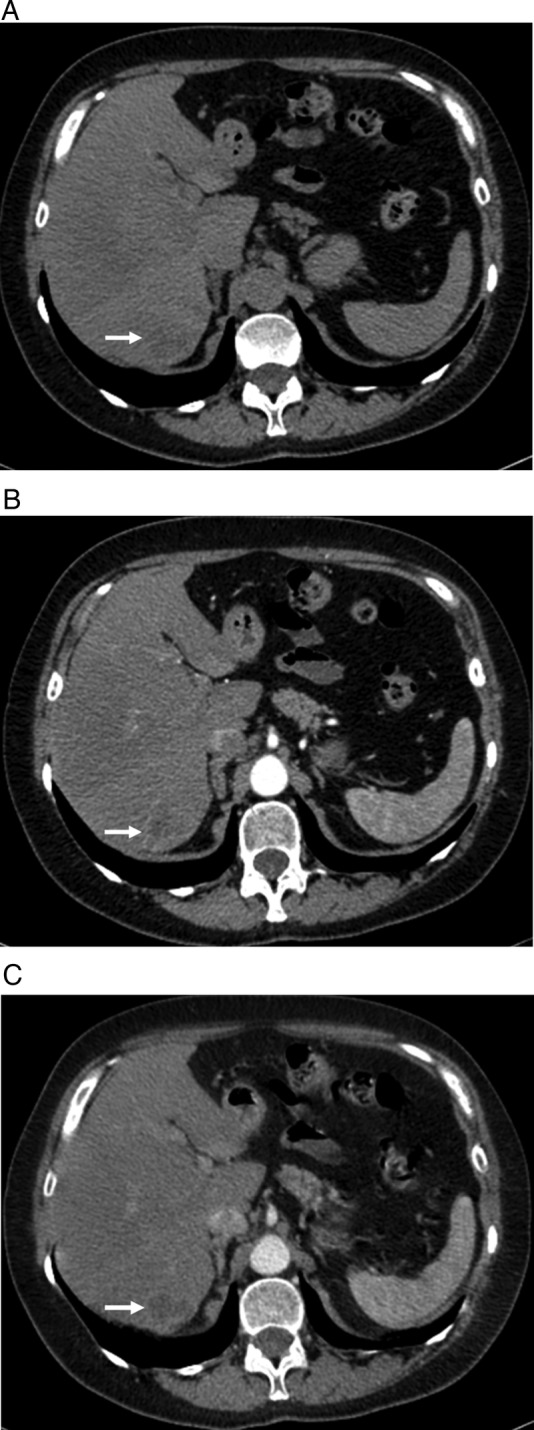
(A) Non-contrast-enhanced CT of the abdomen demonstrates a 2.7 cm hypodense focal lesion in segment VII of the liver (arrow). (B) After the intravenous administration of iodinated contrast the lesion showing moderate enhancement in the arterial phase. (C) In the portal-vein phase there is contrast wash out with peripheral capsular enhancement.
Figure 2.
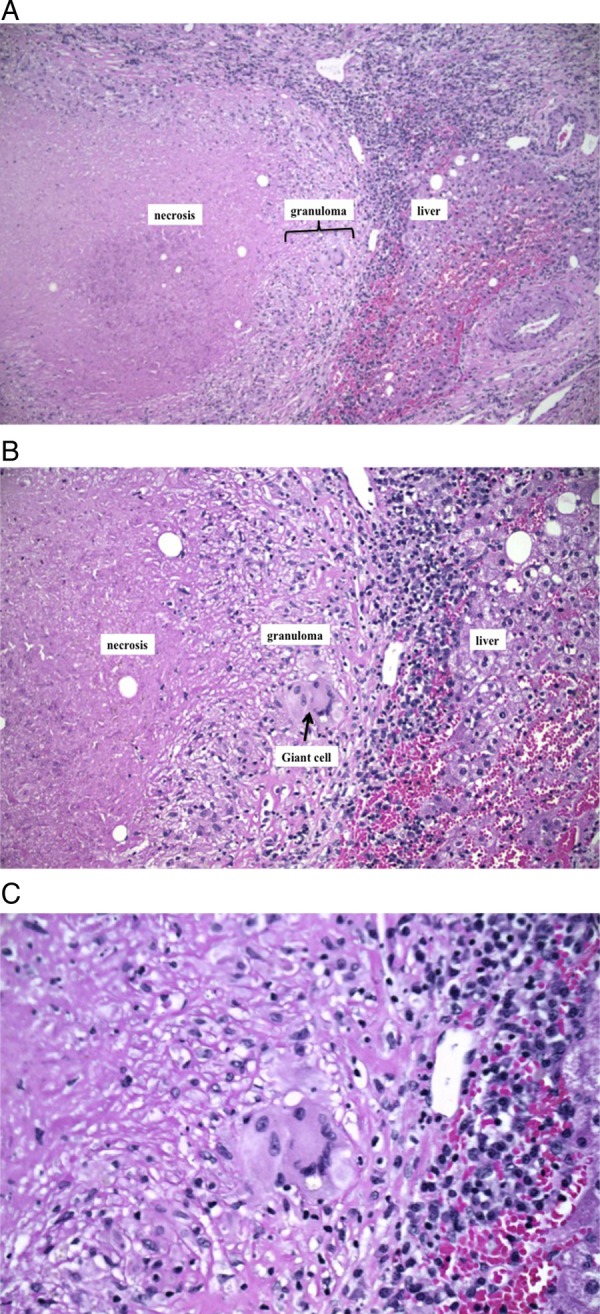
(A) The presence of centrally necrotic granuloma (caseation) in liver parenchyma (H&E, ×10). (B) The presence of centrally necrotic granuloma (caseation) in liver parenchyma (H&E, ×20). (C) Granuloma with multinucleated giant cell (H&E, ×40).
Treatment
The patient underwent a diagnostic laparotomy and right lateral segmentomy of the liver. Histology revealed granulomatous inflammation with Langhans giant cells suggesting a mycobacterial infection. Histochemical examinations (staining Ziehl-Neelsen, Grocott and PAS) for acid-fast bacilli and fungal organisms were negative. Also Mycobacterium tuberculosis DNA by PCR were negative. From the histological examination, the presence of caseating granuloma is diagnostic and a quadruple therapy (for 1 year) is recommended due to the increasing incidence of drug resistance TB.1 The patient refused to take antituberculous therapy after surgery. The postoperative period was uneventful and at 1 year follow-up she remains asymptomatic, with no sign of recurrent disease.
Discussion
The term ‘hepatic TB’ is a distinct clinical entity, with symptoms and signs related only to the hepatic involvement. Hepatic TB has been classified by Levine into: (1) miliary TB; (2) pulmonary TB with hepatic involvement; (3) primary liver TB; (4) focal tuberculoma or abscess; and (5) tuberculous cholangitis.4 The most common form of hepatic involvement is the miliary form of TB. It is believed that the route of transmission is different between the miliary TB and the primary liver TB. In the first one haematogenous dissemination of the bacteria seems to be the route of dissemination while in primary hepatic TB, the tubercle bacillus reaches the liver through the portal vein from the intestine.5 Primary liver TB was observed in about 1% of cases in two large hepatic TB series including 296 patients and in other studies.1 2 6 The prevalence of tuberculous liver abscess was just 0.34% in patients with hepatic TB.7 On the other hand, hepatic involvement can be seen in up to 80% of disseminated cases of TB.8 This disorder is referred to in the literature as atypical TB of the liver, tuberculous hepatitis, hepatic TB, hepatobiliary TB and localised or local hepatic TB.5 The most frequently encountered clinical laboratory findings of hepatic TB are hepatomegaly (90%), elevated alkaline phosphatase (80%), fever (70%), weight loss (60%), abdominal pain (50%), night sweats, anorexia and more seldom jaundice. Less specific findings are anaemia, hypoalbuminemia and hyponatremia.2 5 6 Imaging studies can pose a diagnostic challenge and the differential diagnosis includes primary hepatocellular carcinoma, cholangiocarcinoma, Klatskin tumours, amoebic liver abscess and pyogenic liver abscess.1 9 Hypoechoic nodules are usually seen during ultrasonography, though rarely do the appearances appear hyperechoic. CT findings usually reveal a round hypodense lesion with slight peripheral enhancement and, occasionally, areas of focal calcification. Non-invasive diagnosis is therefore difficult, and up to 90% of cases require a laparotomy to make the diagnosis according to Brookes et al8 and Arora et al, but it is preferably to proceed first in US-guided or CT-guided fine-needle biopsy before planning a laparotomy. 10 Although hepatic tuberculoma is a rare entity, it should be put into differential diagnosis upon facing a solitary-occupying lesion of the liver.
Regarding liver histology, in a review of 96 patients with a predominantly hepatic presentation of TB, the findings were granulomas (95.8%), caseation (83.3%), fatty changes (42%), portal fibrosis (20%) and acid-fast bacilli in association with granulomas (9%).6 Granulomas are aggregates of modified macrophages (epithelioid cells) and other inflammatory cells that accumulate after chronic exposure to antigens. The underlying trigger may be exposure to noxious agents that cannot be biochemically degraded or to immune dysfunction. The ultimate result is a release of a variety cytokines that stimulate mononuclear cells that fuse to form multinucleated giant cells with a surrounding rim of lymphocytes and fibroblasts. The extent of inflammation associated with granuloma formation is variable. In general tubercle bacilli are very rarely encountered in the hepatic TB.3 5
The presence of a caseating granuloma in histological examination is diagnostic. At the end authors recommend to treat the hepatic TB with the standard four-regimen with rifampicin, isoniazid, ethambutol and pyrazinamide. Even in occasions where the patient underwent a surgical procedure before the diagnosis or the PCR and the staining are negative, there is a rationale for antitubercular treatment, as this would help in eliminating any residual disease and also treat any undetected focus.1 7–9
Learning points.
We present a case of an atypical form of presentation of hepatic tuberculosis.
The diagnosis of isolated hepatic tuberculosis can be quite challenging in immunocompetent patients and non-endemic countries.
Combinations of antituberculosis drugs should be the treatment of choice for the hepatic tuberculosis.
In any case of a space-occupying lesion of the liver with imaging findings strongly suggestive of a malignant neoplasm, Ultrasound or CT-guided fine-needle aspiration (FNA) should be performed first.
If the FNA results are inconclusive, resection may be warranted to establish the diagnosis and treat this rare condition.
Footnotes
Contributors: KZ, VK, PFand NA contributed in designing study. KZ, VK and PF contributed in the data collection. KZ, VK and PF contributed in the manuscript drafting, and NA in the revision of manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Mert A, Ozaras R, Tabak F, et al. Localized hepatic tuberculosis. Eur J Intern Med 2003;14:511–12 [DOI] [PubMed] [Google Scholar]
- 2.Hersch C. Tuberculosis of the liver: a study of 200 cases. S Afr Med 1964;38:857–63 [PubMed] [Google Scholar]
- 3.Coash M, Forouhar F, Wu CH, et al. Granulomatous liver diseases: a review. J Formos Med Assoc 2012;111:3–13 [DOI] [PubMed] [Google Scholar]
- 4.Levine C. Primary macronodular hepatic tuberculosis: US and CT appearances. Gastrointest Radiol 1990;15:307–9 [DOI] [PubMed] [Google Scholar]
- 5.Ferrari TC, Couto CM, Vilaça TS, et al. Localized hepatic tuberculosis presenting as fever of unknown origin. Braz J Infect Dis 2006;10:364–7 [DOI] [PubMed] [Google Scholar]
- 6.Essop AR, Posen JA, Hodkinson JH, et al. Tuberculous hepatitis: a clinic review of 96 cases. Q J Med 1984;53:465–77 [PubMed] [Google Scholar]
- 7.Hassani KI, Ousadden A, Ankouz A, et al. Isolated liver tuberculosis abscess in a patient without immunodeficiency: a case report. World J Hepatol 2010;2:354–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brookes MJ, Field M, Dawkins DM, et al. Massive primary hepatic tuberculoma mimicking hepatocellular carcinoma in an immunocompetent host. Med Gen Med 2006;8:11. [PMC free article] [PubMed] [Google Scholar]
- 9.Arora R, Sharma A, Bhowate P, et al. Hepatic tuberculosis mimicking Klatskin tumor: a diagnostic dilemma. Indian J Pathol Microbiol 2008;51:382–5 [DOI] [PubMed] [Google Scholar]
- 10.Oliva A, Duarte B, Jonasson O, et al. The nodular form of local hepatic tuberculosis. A review. J Clin Gastroenterol 1990;12:166–73 [DOI] [PubMed] [Google Scholar]


