Abstract
An 85-year-old woman with failure to thrive due to poor oral intake was admitted owing to dehydration. A nasogastric (NG) tube was inserted for the initiation of enteral feedings. The tube position was confirmed by gastric auscultation after insufflating air through the tube. A chest X-ray revealed that the NG tube traversed the right main stem bronchus with its tip ending in the right costophrenic angle adjacent to the pleura. No pneumothorax was identified. The tube was removed and a short while later the patient developed mild chest discomfort. A repeat chest X-ray revealed significant pneumothorax on the right side. She was treated conservatively with 100% oxygen with successful resolution of the pneumothorax.
Background
Nasogastric tube insertion is a commonly performed procedure for hospitalised patients. Traditional bedside confirmatory signs of gastric placement are often unreliable. Tracheobronchial complications can occur with nasogastric tube insertion. We present a case of a right-sided malpositioned NG tube which caused a pneumothorax only on its removal. A chest X-ray after the removal of a malpositioned NG tube is necessary for the recognition of this rare complication.
Case presentation
An 85-year-old woman with a history of advanced dementia was admitted to the hospital with failure to thrive. Her attendant stated that she had not ingested any substantive food or fluids for 2 weeks prior to admission. She had decreased skin turgor and dry mucous membranes. Her lab reports revealed a blood urea nitrogen (BUN) of 82 mg/dL, creatinine of 2.2 mg/dL and sodium of 156 mEq/L, consistent with severe dehydration and intravascular volume depletion. She was treated with intravenous fluids with normalisation of the renal indices and sodium. A nasogastric tube was placed to initiate enteral feedings. The tube was inserted to 50 cm, its intended length, without any resistance or cough. The operator heard epigastric gurgling after air insufflation. A chest X-ray was obtained to confirm the NG tube position; it revealed that the tube was traversing the right main stem bronchus and its tip was located in the right costophrenic angle adjacent to the pleura. There was no pneumothorax present at this time (figure 1). The NG tube was removed, and several hours later the patient developed mild chest discomfort. Repeat chest X-ray revealed significant pneumothorax (figure 2). The patient was treated with 100% oxygen with complete resolution of the pneumothorax over a 2-day period.
Figure 1.

Nasogastric tube in a right costophrenic angle abutting the pleura.
Figure 2.
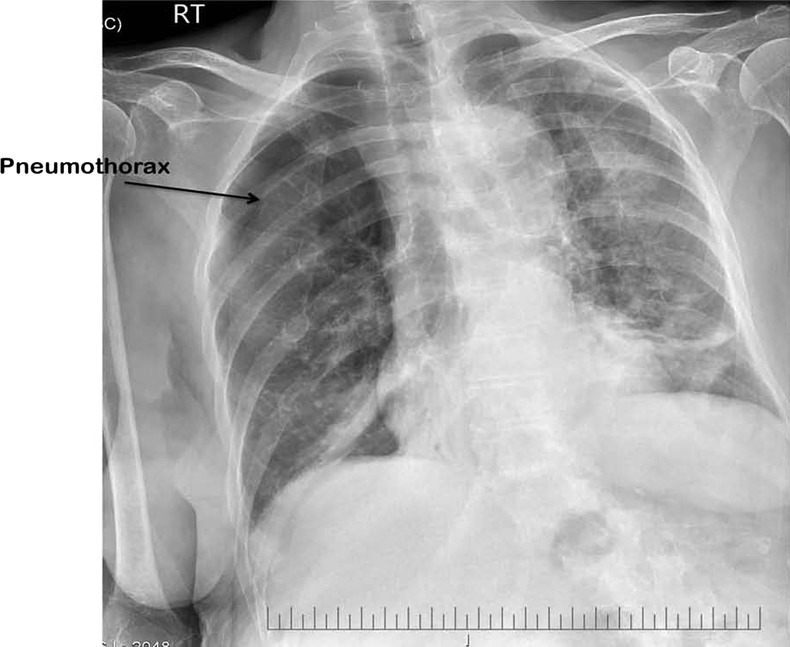
Right-sided pneumothorax after removal of the nasogastric tube.
Discussion
Nasogastric tube insertion is a commonly performed procedure. It is generally blindly inserted with confirmation based on clinical findings, including auscultation of gastric gurgling on insufflation of air.1 This finding is associated, however, with a 20% rate of tube malposition and therefore cannot be relied on.2 A chest X-ray is often obtained after NG tube placement to confirm the tube position.
Inadvertent malposition into the tracheobronchial tree has been reported up to 2% of the time and is associated with a mortality of 0.3%.3 4 Patients may cough as an indication of a foreign body in the tracheobronchial tree; however, a majority of malpositioned tubes are not associated with any sensation of resistance or malposition.1
A number of patient characteristics have been identified that are associated with an increased risk of bronchopulmonary complications associated with NG tube insertion. These include altered mental status, heavy sedation, the presence of a tracheostomy, critical illness, an absent cough reflex and difficult or multiple tube placements.5 Although our patient was demented, her mental status was not depressed; she was oriented to persons and responded to verbal commands.
To our knowledge, this is the first reported case of a pneumothorax caused by nasogastric tube removal. Prior cases in the literature have reported pneumothoraces, which occurred with the placement of an NG tube and not with its withdrawal.1–5 It is important, therefore, to monitor the patient after the removal of a malpositioned NG tube to ensure that no significant damage occurs. A follow-up chest X-ray after the removal of the NG tube is helpful and should be performed, especially when the tube abuts the pleura.
Learning points.
Clinical signs of nasogastric (NG) tube placement are not reliable. A chest X-ray is usually obtained to confirm the tube position.
Pneumothorax is extremely rare after NG tube removal.
A chest X-ray after the removal of a malpositioned NG tube should be obtained to evaluate for complications, when the NG tube is in the proximity of the pleura.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Pillai JB, Vegas A, Brister S. Thoracic complications of nasogastric tube: review of safe practice. Interact CardioVasc Thorac Surg 2005;4:429–33 [DOI] [PubMed] [Google Scholar]
- 2.Benya R, Langer S, Morbarhan S. Flexible nasogastric feeding tube tip malposition immediately after placement. JPEN J Parenter Enteral Nutr 1990;14:108–9 [DOI] [PubMed] [Google Scholar]
- 3.Sorokin R, Gorrlieb JE. Enhancing patient safety during feeding-tube insertion: a review of more than 2000 insertions. JPEN J Parenter Enteral Nutr 2006;30:440–5 [DOI] [PubMed] [Google Scholar]
- 4.de Aquilar-Nascimento JE, Kudsk KA. Clinical costs of feeding tube placement. JPEN J Parenter Enteral Nutr 2007;31:269–73 [DOI] [PubMed] [Google Scholar]
- 5.Krenitsky J. Blind bedside placement of feeding tubes: treatment or threat? Practical Gastro 2011; 3:32–42. [Google Scholar]


