Abstract
Gastrointestinal tuberculosis is a major health problem in the developing countries. Duodenal involvement is uncommon and can mimic superior mesenteric artery syndrome. Our case presented as proximal intestinal obstruction had tubercular stricture in the third part of the duodenum, proximal jejunum and ileocecal region, an uncommon and difficult intraoperative situation.
Background
Tuberculosis is a major health problem worldwide. In India, it is endemic. The most common manifestation is a pulmonary disease, but involvement of the gastrointestinal tract is not uncommon. Gastrointestinal tuberculosis often involves the ileocecal region. The stomach as well as the duodenum are rare sites for tuberculosis and are usually a result of secondary spread from a primary pulmonary disease. An autopsy series reported an incidence of only 0.5%. A primary case of gastroduodenal tuberculosis is an even rarer disease and only a few cases are reported in the literature.1
Case presentation
A 35-year-old woman presented with fullness after solid food, but not with liquids for the past 3 years. For the past 6 days she had pain in the abdomen with distension even with liquids, which was relieved with non-projectile, bilious vomiting. She lost 10 kg weight in the last 1 year. The patient had symptoms of ball rolling sensation in her abdomen. No history of fever, cough, haematemesis and melaena was found. On examination, the patient was emaciated with pulse 96/min and blood pressure 106/70 mm Hg. The abdomen was soft, non-tender and non-distended.
Investigations
The patient had haemoglobin of 15.3 g/dL, total leucocyte count 20 100/mm3 and erythrocyte sedimentation rate 39 mm/h. HIV test was non-reactive. Chest X-ray was normal. Esophagogastroduodenoscopy showed dilated first and second part of duodenum. CT of the abdomen showed dilation of the first and second part of the duodenum with abrupt narrowing and wall thickening of the third part (figure 1). Small bowel loops distal to the third part of duodenum were collapsed.
Figure 1.
CT scan of the abdomen showing dilated second part of the duodenum with collapsed distal bowel loops secondary to stricture at third part.
Differential diagnosis
Superior mesenteric artery syndrome
Duodenal third part stricture
Treatment
The patient was kept nil per oral with continuous Ryle's tube suction, intravenous fluids and antibiotics. On abdominal exploration we found three strictures. They were in the third part of the duodenum, jejunum at 15 cm from duodenojejunal junction (figure 2) and ileocaecal junction (figure 3). Multiple tubercles were seen, so diagnosis of multiple tubercular strictures was made. Jejunal stricture was resected. Distal end of jejunum was brought transmesocolic and anastomosed with the second part of the duodenum (side-to-side Roux-en-Y duodenojejunostomy). Proximal end of resected jejunum was anastomosed with jejunum (end to side). Segmental ileocecal resection with ileocolic anastomosis was performed.
Figure 2.
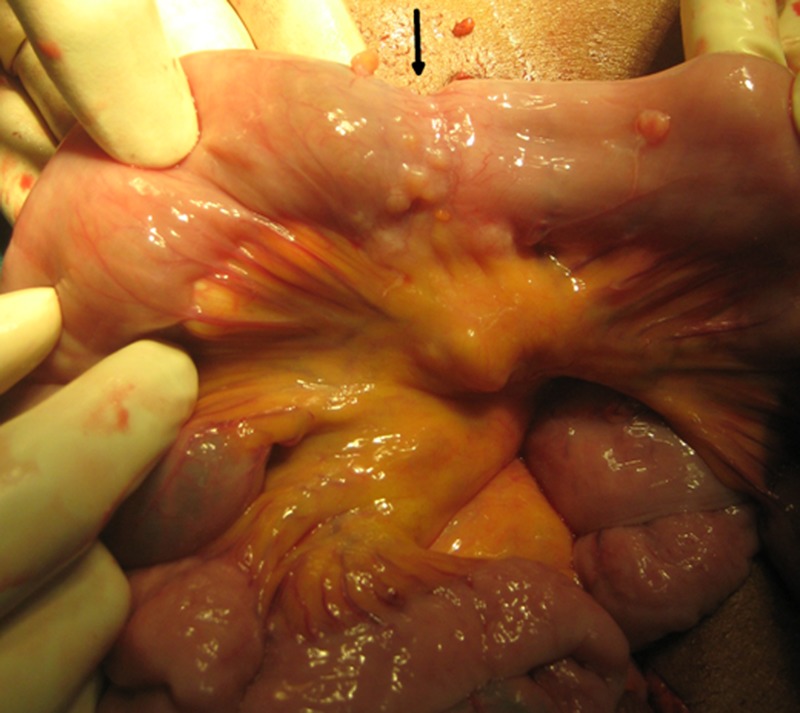
Proximal jejunal stricture with tubercles.
Figure 3.

Tubercular stricture at ileocecal region.
Outcome and follow-up
The patient had an uneventful postoperative period. Her histopathology showed granulomas composed of epitheloid cells and foreign body giant cells with foci of caseous necrosis along with fibrin and inflamed adipose tissue consistent with tuberculosis peritonei (figure 4). She was started on a 9-month course of antitubercular treatment (ATT) with rifampicin, isoniazid and pyrazinamide. She was fine at follow-up.
Figure 4.

Granulomas composed of epitheloid cells and foreign body giant cells with foci of caseous necrosis.
Discussion
Duodenal involvement by tuberculosis is 30 times rarer than ileocaecal region, which is the most common site involved in intestinal tuberculosis.2 3 Factors such as scarcity of lymphoid tissue, an intact mucosa, gastric acidity and a rapid transit of tubercular bacilli due to gastric peristalsis explain the rarity of duodenal involvement even in patients with advanced tuberculosis. The possible routes of infection considered in its aetiopathogenesis include: haematogenous spread, lymphatic spread, spread from serosa by continuity from adjacent structures, especially lymph nodes, and in the present case the infection may have spread directly through mucosa mainly by ingested bacilli. Duodenal tuberculosis is pathologically classified into four types: (1) ulcerative, (2) hyperplastic, (3) enteroperitoneal and (4) infiltrative. The duodenal obstruction in the present case seems to be the result of development of fibrous stricture due to its hyperplastic variety.2 4 In cases presenting with intestinal obstruction, extensive surgical procedures such as resections, etc, are no longer required and patients respond well to minimal surgical interventions like stricturoplasty with an adequate ATT.5 Bypass procedures along with ATT are required in the presence of extra luminal duodenal obstruction or in cases where duodenoplasty is not feasible due to extensive periduodenal inflammation.4 5 In cases with proximal tubercular stricture we should rule out any other stricture in rest of bowel as in our case with stricture in duodenal third part, jejunum and at ileocecal region. Gastrojejunostomy remains the procedure of choice in such patients with pyloroduodenal involvement.2 4 6 Owing to its associated complications like stoma ulceration and blind loop syndrome, duodenojejunostomy is preferred in cases with distal duodenal involvement.
Learning points.
Apart from developing countries like India where tuberculosis is endemic, a recent increase in its incidence has been mainly due to an increase in AIDS, thus demanding awareness among physicians of this rare clinical entity.
The patient with duodenal third part tuberculosis also mimics superior mesenteric artery syndrome.
The patient may have multiple tubercular strictures, so rest of the intestine should be explored.
Stricturoplasty and segmental resection anastomoses are the treatment options.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Rao YG, Pande GK, Sahni P, et al. Gastro duodenal tuberculosis management guidelines, based on a large experience and a review of the literature. Can J Surg 2004;47:364–8 [PMC free article] [PubMed] [Google Scholar]
- 2.Deshpande SG, Mehta MJ. Tubercular stricture of duodenum. JIMA 1975;65:306. [PubMed] [Google Scholar]
- 3.Acharya GV, Gheewala MN, Dastur DK. Tuberculosis of the duodenum: a review of five cases. J Post Grad Med 1967;13:140. [PubMed] [Google Scholar]
- 4.Morirangthan GS, Singh NS, Bhattacharya IN, et al. Gastric outlet obstruction due to duodenal tuberculosis: a case report. Int Surg 2001;86:132. [PubMed] [Google Scholar]
- 5.McGee GS, Williams LF, Potts J, et al. Gastrointestinal tuberculosis. Resurgence of an old pathogen. Am Surgeon 1989;55:16. [PubMed] [Google Scholar]
- 6.Gupta SD. Duodenal tuberculosis. Indian J Surg 1971;33:123 [Google Scholar]



