Abstract
Objective
One of the key goals of the current reforms in the English National Health Service (NHS) under the Health and Social Care Act, 2012, is to increase the accountability of those responsible for commissioning care for patients (clinical commissioning groups (CCGs)), while at the same time allowing them a greater autonomy. This study was set out to explore CCG's developing accountability relationships.
Design
We carried out detailed case studies in eight CCGs, using interviews, observation and documentary analysis to explore their multiple accountabilities.
Setting/participants
We interviewed 91 people, including general practitioners, managers and governing body members in developing CCGs, and undertook 439 h of observation in a wide variety of meetings.
Results
CCGs are subject to a managerial, sanction-backed accountability to NHS England (the highest tier in the new organisational hierarchy), alongside a number of other external accountabilities to the public and to some of the other new organisations created by the reforms. In addition, unlike their predecessor commissioning organisations, they are subject to complex internal accountabilities to their members.
Conclusions
The accountability regime to which CCGs are subject to is considerably more complex than that which applied their predecessor organisations. It remains to be seen whether the twin aspirations of increased autonomy and increased accountability can be realised in practice. However, this early study raises some important issues and concerns, including the risk that the different bodies to whom CCGs are accountable will have differing (or conflicting) agendas, and the lack of clarity over the operation of sanction regimes.
Keywords: Accountability, Case Study Research, Clinical Commissioning Groups
Strengths and limitations of this study.
The study took place in the early phases of CCG establishment, and therefore provides a snapshot of a developing situation.
The study included detailed case studies in eight sites across England, and so provides a robust picture of clinical commissioning groups (CCGs) developing accountability relationships.
The triangulation of evidence from interviews, document analysis and observation enhances the trustworthiness of the findings.
Introduction
‘The Government's reforms will liberate professionals and providers from top-down control. This is the only way to secure the quality, innovation and productivity needed to improve the outcomes. We will give responsibility for commissioning and budgets to groups of general practitioner (GP) practices; and providers will be freed from government control to shape their services around the needs and choices of patients. A greater autonomy will be matched by an increased accountability to patients and democratic legitimacy, with a transparent regime of economic regulation and quality inspection to hold providers to account for the results they deliver’.1
Having initially promised ‘no more top-down reorganisations of the National Health Service (NHS)’,2 the UK Coalition Government elected in 2010 immediately embarked on a radical overhaul of the NHS in England (the NHSs in Wales, Scotland and Northern Ireland are governed by the devolved authorities), with a reorganisation that affects most parts of the service. As this quote suggests, the driving force behind the reforms was a desire to ‘liberate’ professionals from top-down control, at the same time as making them more accountable. In brief, the changes maintain and extend the notion of a ‘quasi-market’ in the NHS, first introduced in the 1990s.3 The overall responsibility for running the NHS has been removed from the department of health (DH) and handed to a new arm's length body, NHS England (NHSE).i The responsibility for commissioning (purchasing) the majority of services for a defined geographical population was historically held by primary care trusts (PCTs). These organisations were managerially dominated, and were directly accountable to the DH (ie, the health ministry). The Health and Social Care Act (HSCA)4 abolished PCTs (from 1 April 2013), passing responsibility for commissioning to primary care physicians (GPs) working together in local clinical commissioning groups (CCGs). These groups were established as statutory bodies from 1 April 2013, and are now responsible for 65% of the overall budget of the NHS, covering a defined geographical area and commissioning routine and emergency care. NHSE will oversee CCGs, and will be responsible for commissioning some services (eg, primary care, specialised services) at a national level. Managerial budgets for CCGs will be significantly less than was the case for PCTs, and they will be expected to ‘buy in’ managerial commissioning support from standalone organisations, known as ‘Commissioning Support Units’ (CSUs).5 Further regulation will be provided by Monitor, who is an arm's length government body originally established to regulate quasi-independent NHS hospitals known as ‘Foundation Trusts’.6 Monitor now has an expanded role as economic regulator of the new NHS system, responsible for the prevention of anticompetitive behaviour, the promotion of integration, setting prices within the system and ensuring service continuity. The responsibility for public health is transferred to local government authorities (LAs), and new LA subcommittees known as Health and Well-being Boards (HWBs) have been created, charged with setting the overarching strategic direction for health and social care services across a geographical area. CCGs will be members of these bodies, and will be expected to set their own priorities in response to the strategic direction set by their local HWBs.
Thus, the new system creates a number of new bodies with significant responsibilities, and redefines relationships in significant ways, with an associated increase in complexity. This increase in complexity in part has come about because of the continued commitment by the UK government to the idea of a market in healthcare, a commitment shared by other governments across the world. However, markets require regulation, and recent scandals in England (such as the recent significant failings of care at Mid Staffordshire NHS Trust (http://www.midstaffspublicinquiry.com/)) have demonstrated just how difficult that regulation can be. One of the official aspirations underpinning the creation of CCGs in England (as demonstrated by the quotation opening this article) is to enable greater accountability, and it is clear from the brief description given above that the success of the new system will, to some extent, depend on how successfully the new accountability relationships are established. However, in spite of very extensive documentation issued to guide CCGs as they established themselves (see http://www.england.nhs.uk/resources/resources-for-ccgs/, accessed June 2013) the exact nature of CCG accountability relationships remains ill-defined and somewhat underspecified. One of the key guidance documents issued to CCGs was a guide to governance processes. Accountability is thus referred to:
CCGs will have to account to the patients and population they serve as well as being accountable to the NHS Commissioning Board (NHSCB; NHSE). This will require a comprehensive and effective patient and public engagement strategy with systems and processes to assure the governing body that this is taking place throughout the organisation. They will need to play a full role on their local HWBs including cooperating, preparing joint strategic needs assessments (JSNAs) and agreeing a joint Health and Wellbeing Strategy. They will also work in partnership with LAs and (as members of the HWBs) have a role in encouraging health and social care commissioners with the aim of securing better integrated health and social care for their patients. They will have a responsibility to ensure that relevant health and care professionals are involved in the design of services and that patients and the public are actively involved in the commissioning arrangements (ref. 7, p.4, emphasis added).
This paragraph summarises potential complexities facing CCGs, referring to a number of different audiences and stakeholders. However, it is silent about the mechanics of the various accountability relationships, and provides no advice as to how any conflicts between them might be resolved.
This article uses evidence from a study of the early development of CCGs to explore how claims to increased accountability might play out in practice. We examine CCG constitutional documents, interviews with CCG leaders and observations of CCG meetings to explore how CCGs are interpreting their accountabilities and how the new system is developing in practice. Although it is early days, and the full effect of the various accountability relationships will not become clear for some time, we believe that it is valuable to highlight developing complexities and potential issues at this point.
What follows is divided into five sections. A short discussion of the relevant dimensions of ‘accountability’ is followed by a more detailed account of the obligations and roles given to CCGs under the HSCA 2012.4 A description of our methods is followed by results and discussion, with a final section summarising the implications of our findings.
Definitions of accountability
Mulgan8 describes accountability as a ‘complex and chameleon-like term’ that has extended beyond an original concern with being ‘called to account’ by some legitimate authority, to incorporate a multitude of additional concepts such as internal notions of personal responsibility and professional accountability to peers. Ryan and Walsh9 argue that, driven by the so-called ‘new public management’ approach,10 accountability in the public sector is particularly complex, with actors in public sector organisations being potentially accountable to multiple audiences, including an informed public as well as to ministers. In order to make sense of this complexity, in this article, we will use the definition suggested by Bovens11: ‘(accountability is) a relationship between an actor and a forum, in which the actor has an obligation to explain his or her conduct, the forum can pose questions and pass judgement, and the actor may face consequences’. This definition brings into focus the notion of authority, alongside the potential for judgement and sanctions. However, it leaves open the currency of accountability: for what aspects of his/her ‘conduct’ must an actor answer? A number of authors have addressed this question.12–14 Leat15offers a fourfold classification: fiscal accountability, focusing on expenditure and financial probity; process accountability, exploring the adequacy of procedures for decision-making; accountability for priorities, providing justification for the way in which an organisation has focused its activities; and programme accountability, by which an actor is held to account for the outcomes of their activity. Turning to the question of sanctions, Brinkerhoff12 sketches the idea of a spectrum, from accountability as the provision of information about an organisation's actions at one end, through the additional requirement to justify those actions, to a sanction-backed formal ‘answerability’, in which different types of sanctions may be enforced in order to ensure compliance at the other. This provides a useful lens through which to consider the strength of any particular accountability relationship.
Accountability thus defined encompasses what Day and Klein16 call ‘managerial accountability’; that is, accountability as a largely technical process, by which those with delegated authority are held to account against clearly specified criteria, agreed in advance, and ‘political accountability’, by which those with delegated authority are answerable for their actions to the public. In this latter form of accountability, the criteria for judgement are themselves subject to debate, and it is characterised by reasons, justification and explanations of behaviour (ibid, p.26), rather than by technical assessment against specified criteria. Such accountability is rarely backed by any form of sanctions other than the possibility that those involved might be subject to a democratic process or public opprobrium. In the real world, simple separation between these two forms of accountability rarely exists, (ibid, p.28), but the distinction remains analytically useful, as it provides a framework within which to think about public accountability, which is rarely tied to specific performance criteria (unlike managerial accountability). Furthermore, political accountability carries the possibility that moral and ethical dimensions of performance might be incorporated into the accountability framework.
Taking these definitions together, five key questions emerge, which were addressed in this study. These are set out in box 1.
Box 1. Key questions about accountability.
To whom are these actors accountable?
For what are they accountable?
What sanctions may apply?
What enforcement mechanisms exist?
Is this accountability managerial (with clear criteria for judgement) or political (involving justification and argument)?
Role and functions of CCGs
Since the introduction of the quasi-market into the NHS there has been an ambition to involve frontline primary care physicians more closely in purchasing care for their patients. Examples include: GP fundholding, total purchasing pilots, GP Commissioning Groups, primary care groups and practice-based commissioning.17 Each of these previous attempts at involving clinicians in commissioning shares one thing: alongside the clinical group there existed an administrative body (initially the Health Authority, latterly the PCT) to take statutory and financial responsibility. Under the HSCA 2012, no such administrative support exists, with CCGs taking on full statutory responsibility from April 2013. From this date, CCGs have been responsible for planning, agreeing, procuring and monitoring a full range of services for their populations. The exact distribution of commissioning responsibilities between CCGs and other new bodies, such as NHSE, is complex, but essentially CCGs are responsible for most elective, urgent and community care.18 In addition, they are responsible for improving the quality of primary care services, and are under a duty to work cooperatively with the LA.19 Finally, they are under a duty to break even financially, and carry responsibility for ensuring that they meet their obligations with regard to safeguarding children and other general duties such as complying with equalities legislation.
Methods
The study took place between September 2011 and June 2012. Data collection involved in-depth case studies in eight emerging CCGs,ii and national web surveys carried out at two points in time (December 2011 and April 2012). In this article, we focus on the results from the qualitative case studies. For a full description of the methods see Checkland et al.20
The eight case study sites were selected to provide maximum variety across a number of characteristics, including size, the homogeneity of the sociodemographic profile of the site and the complexity of the local health economy and local government institutions (table 1).
Table 1.
Site characteristics
| Site | Size (quintile) | Sociodemographic profile and area | Major providers | Local authorities |
|---|---|---|---|---|
| 1 | 3 | Mixed, north | 1 | >1 |
| 2 | 5 | Relatively homogeneous, pockets of deprivation, north | >1 | 1 |
| 3 | 5 | Relatively homogeneous, affluent, pockets of deprivation, south | >1 | >1 |
| 4 | 2 | Relatively homogeneous, deprived, north east | >1 | 1 |
| 5 | 3 | Relatively homogeneous, deprived, midlands | 1 | >1 |
| 6 | 2 | Relatively homogeneous, affluent, south | 1 | 1 |
| 7 | 4 | Mixed, south | >1 | 1 |
| 8 | 4 | Mixed, northwest | 1 | 1 |
The smallest sites covered a population of 88 000–138 000, while the largest were responsible for a population of >500 000. Data collection involved observation of a wide variety of different types of meetings, semistructured interviews and analysis of available documents such as meeting minutes, strategy plans and draft constitutions. In total, we observed 439 h of meetings and carried out 96 interviews (see table 2). Meetings included, for example, CCG governing body meetings, working group meetings and meetings of the local HWB.
Table 2.
Interviews
| Type of respondent | Number interviewed | Number of interviews (some interviewed twice) |
|---|---|---|
| Managers (NHS) | 47 | 49 |
| GPs | 33 | 36 |
| Lay members | 5 | 5 |
| Practice managers | 3 | 3 |
| Nurse (clinical lead) | 1 | 1 |
| Others (eg, Trust manager) | 1 | 1 |
| Local authority representatives | 1 | 1 |
| Total | 91 | 96 |
GP, general practitioner; NHS, National Health Service.
Interviews were recorded and transcribed, and detailed contemporaneous fieldnotes were written in meetings. These data sources were analysed alongside available documents (including those produced locally and guidance issued by the DH/NHSCB) supported by the qualitative data analysis software Atlas ti. We also examined available constitutional documents for our case study sites.
In this article, the analysis focused on the ways in which the ideas of accountability surfaced in all of the data sources, looking to answer the following questions:
To whom are developing CCGs formally accountable, and to whom do they regard themselves as being accountable?
For what aspects of their performance do they expect to provide an account to each stakeholder?
What sanctions might apply?
What (if any) potential conflicts or problems can be identified in the new system?
Results and discussion
In the following section, the results from the study will be presented. We identified two main forms of accountability relationships of concern to the groups: accountability to external groups and internal accountability.
External accountability
Relationship with NHSE
NHSE provided a ‘model constitution framework’,21 which CCGs were encouraged to adapt for their own purposes. This makes it clear that CCGs are formally accountable to NHSE and to the Secretary of State for Health22:
The group will (1) comply with all relevant regulations; (2) comply with directions issued by the Secretary of State for Health or the NHSCB; and (3) take account, as appropriate, of documents issued by the NHSCB (NHSE).21
The ‘regulations’ referred to are pieces of secondary legislation. The potential accountabilities here are broad and as yet undefined. In addition to general duties (such as a duty to promote integration, a duty to involve the public) first set out in earlier documents,18 the model constitution sets out some specific financial duties, including the need to maintain expenditure within agreed limits, the duty to ‘take account’ of directions issued by NHSE and the requirement to ‘publish an account’ of how additional payments had been spent (ref. 21, para 5.3).
As well as this essentially fiscal accountability, CCGs are also accountable for the outcomes, set out in the form of a new ‘Clinical Commissioning Group Outcomes Indicator Set’ (CCGOIS). This was first mooted in the White paper, ‘Equity and Excellence: Liberating the NHS’:
A new NHS Outcomes Framework will provide direction for the NHS. It will include a focused set of national outcome goals determined by the Secretary of State, against which the NHSCB 9NHSE will be held to account, alongside overall improvements in the NHS. In turn, the NHS Outcomes Framework will be translated into a commissioning outcomes framework for GP consortia, to create powerful incentives for effective commissioning (ref. 1, p.22).
The indicators that have been published so far vary in scope, from those focused on reducing mortality to those requiring the provision of particular services, such as ensuring patients with a stroke have a visit from a specialist nurse (http://www.nice.org.uk/aboutnice/cof/cof.jsp). Guidance issued in December 201223 suggests that, in addition to a payment for meeting target thresholds on these indicators, what Leat15 calls ‘programme accountability’ for these outcomes will form part of NHSE's overall annual assessment of CCG performance.
The first hurdle for CCGs to pass was the requirement to be ‘authorised’ by NHSE. This process involved the submission of evidence by CCGs under six ‘domains’ relating to a strong clinical and professional focus, patient and public engagement, good governance arrangements, collaboration and good leadership. Those CCGs not deemed ready for full authorisation were initially ‘authorised with conditions’. While public comments by the then Secretary of State for Health Andrew Lansley initially implied that such conditions would be minimal or rare,24 in practice, only 43 of 211 CCGs achieved authorisation without conditions, 158 had conditions imposed and 10 had significant conditions backed by legal directions.
Once authorised, the guidance states:
Annual assessment: once authorised (with or without conditions), each CCG is subject to an annual assessment. This will consider how well a CCG has performed its functions in that year, and as part of that assessment, determine the nature of support or conditions going forward, based on its performance and other aspects of its organisational capabilities and relationships, and will enable the continued development of CCGs (ref. 25, p.11).
The requirements against which this ‘assessment’ will be made have not yet been set out, although it seems likely that the CCGOIS will be involved.26
It is thus clear that CCGs will be held accountable by NHSE, and that this will be backed up by sanctions, including loss of ability to function as an autonomous statutory body, and loss of income (the ‘quality premium’ will be tied to performance against the CCGOIS). The accountability implied here is a managerial one, backed up by explicit performance measures.
We found that this significant formal (and sanction-backed) accountability to NHSE was recognised in the draft constitutions under development in our case study sites, with most carrying unchanged the language provided by the model documents. However, those involved with setting up CCGs in our case study sites did not seem to have appreciated either the extent of these obligations or their potential impact. Indeed, across 439 h of observation and 96 interviews, there were only three references to ‘being held to account’ by NHSE, and ‘accountability’ of all sorts was hardly mentioned either in the meetings which we observed. Furthermore, although it was known that there would be an ‘outcomes framework’, this was also rarely mentioned. It may be that this was in part a function of the timing of our data collection, which took place before NHSE was formally constituted and before the draft CCGOIS was published. However, it still seems worthy of remark that the discourse within our case study CCGs showed little apparent recognition of the extent of the external accountability regime to which they will be subjected to. When accountability to the wider NHS was discussed, the most common type of accountability mentioned was fiscal accountability. Furthermore, in response to an open-ended question in our second web-based survey (followed up in subsequent telephone interviews) about their ongoing relationship with NHSE, by far the largest category of responses were those calling for NHSE to give CCGs freedom, imposing few burdens such as reporting requirements, targets or other forms of performance management.
Accountability to the public
Clause 4.5 of the model draft constitution provided by NHSE is headed ‘accountability’. It appears to construe this largely in the relatively weak sense of transparency, listing a series of mechanisms the CCG will use to ‘demonstrate accountability’:
4.5.1. The group will demonstrate its accountability to its members, local people, stakeholders and the NHSCB (NHSE) in a number of ways, including by:
Publishing its constitution;
Appointing independent lay members and non-GP clinicians to the group's governing body;
Holding meetings of the group's governing body in public (except where the group considers that it would not be in the public interest in relation to all or part of a meeting);
Publishing annually a commissioning plan;
Complying with local authority health overview and scrutiny (O&S) requirements;
Meeting annually in public to publish and present its annual report;
Producing annual accounts with respect to each financial year which must be externally audited;
Having a published and clear complaints process;
Complying with the Freedom of Information Act 2000;
Providing information to NHSE as required;
Publishing the group's principal commissioning and operational policies.
Most of our case study CCGs adopted this clause as it stands for their constitutions, although two sites omitted clause K.
In contrast to the relative silence about their future relationship with NHSE, our case study CCGs appeared keenly aware of the need to be accountable to their patients and the public. This GP expressed this clearly:
I think what we haven’t done yet and what we’re trying to organise now…is go one step further and recognise that we are after all accountable to the public, we’re there to serve them, we are paid by them, we’re there to provide their health needs [GP ID 200]
The same GP went on to describe a pilot programme to engage local people in discussions about service developments, arguing that setting up robust mechanisms would in some way protect them against the centralising tendencies of NHSE:
‘that will give true public accountability to the CCGs and Health and Wellbeing Boards and I think it will be very hard for agencies like [NHS England] to argue against it if the public back it. So I think that counteracts the fear of centralisation in the new reforms. [GP ID 200]
Mechanisms for ensuring accountability to the public were in the early stages of development at the time of our data collection. Holding meetings in public was seen as important, but there were some concerns. One site had set up these meetings with the opportunity for the public to ask questions only at the beginning of the meeting, rather than at the end when they might have been able to respond to what they had heard. In an interview we were told:
I don't know why they've set it up this way to be honest. I haven't been involved in that, so I don't know what the rationale is. I've got a feeling that was how the PCT used to operate, but I might be wrong. I mean I think if we're trying to engage with our public, but only allow them to speak at the beginning, before we've actually said anything…it does rather go against the ethos, I think [Manager ID 122]
There was a general awareness that meeting in public alone will not ensure true public accountability, and all of our study site CCGs were intending to set up additional forums for patients and the public to become involved with the work of the CCG, including patient forums, community involvement groups, public events and the publication of newsletters. They thus showed a significant rhetorical commitment to the essentially political accountability represented by the so-called ‘public accountability’, but, at the time of data collection, arrangements to put this in practice were rudimentary and did not yet differ significantly than those set up by their predecessor organisations, PCTs.
CCGs are also required to have at least two lay members in their governing body.27 In practice, those appointed as ‘lay’ members in our case study sites tended to be people with past NHS experience, with ex-non-executive directors of PCTs a popular choice. PCTs were required to have a majority of non-executive directors, so that the executive directors could be outvoted if necessary. This will not be the case in CCGs, suggesting that, on paper at least, the ‘public’ voice within CCGs’ governing bodies will be less powerful than it has been in the past NHS commissioning bodies. We saw no clear differences in attitude or approach between the lay members and the professional members of governing bodies.
In addition to these CCG-led approaches to public accountability, the HSCA 2012 establishes new bodies called local Healthwatch.1 These organisations did not exist at the time of our data collection, but official documents suggest that they will be expected to scrutinise CCGs’ performance and hold them to account in some way, although the mechanisms by which this will take place are far from clear.
Other external accountabilities
CCGs also have some external accountability to other organisations. These include the economic regulator, Monitor (responsible for ensuring that CCGs adhere to competition rules); HWBs; LA O&S committee (OSC); and the Local Medical Committee (LMC). The LMC is the local representative body for GPs. Members are elected from the local GP population, and, historically, LMCs have played a role in negotiating with PCTs on behalf of GPs in their role as providers of services.
Monitor
Under the HSCA 2012, Monitor is the economic regulator of the whole NHS system, including promoting competition between providers of care. It is empowered to require CCGs to account for their behaviour with respect to procurement, and this accountability will be formally backed up by the sanctions of competition law. At the same time, Monitor is required to promote the integration and cooperation between providers of health services (HSCA 2012 section 66). It remains to be seen how these apparently conflicting responsibilities will play out. At the time of our fieldwork, the future role of Monitor impinged little on our case study sites. This is not surprising, as at this time, the details of how Monitor's future role will operate are not yet fully developed at the national level.
Accountability relationships with the LA
HWBs are new LA bodies which are responsible for setting the strategic direction for health and social care, leading to the formal assessment of local needs. These are in differing states of development across the country, and, at the time of data collection, it was unclear how the mutual ‘holding to account’ between HWBs and CCGs would operate in future. HWBs are responsible for developing the annual Joint Strategic Needs Assessment (JSNA), and CCGs are required to ‘take account’ of this in developing their own strategic plans. CCGs have representatives on their local HWBs, and will therefore be party to the JSNA development. Should the HWB consider that the CCGs plans do not fit within it, they will be able to ask the CCG to ‘provide an account’ to explain why this is the case. However, no sanctions exist should the CCG continue to disregard the HWB. While it remains early days, our study found evidence of two approaches to this developing relationship.28 In some sites, the CCGs appeared to see themselves as an integral and important part of the development of the HWB, seeing themselves as ‘co-owners’ of the HWB with the LA. In other areas, we saw HWBs developing separately, with the CCG representatives present at meetings but apparently seeing themselves as representing the CCG rather than as partners in the HWB process. It remains to be seen how these differing approaches develop over time, and how HWBs will react should CCGs decide to disregard their concerns.
The other key LA accountability mechanism is via the Overview and Scrutiny (O&S) process. Historically, Overview and Scrutiny Committees (OSCs) were empowered to examine any ‘significant’ changes to local services, requiring relevant NHS senior managers to attend and explain their plans. Should the committee be unconvinced, they had the power to refer the proposed change to the Secretary of State for Health. It was initially proposed that this scrutiny function would be assumed by HWBs, but after some debate, it was decided that LAs should retain it as a separate function.29 However, considerable uncertainties remain as to how this will function in practice.19 Given the early stages of development of the new structures, it is not surprising that the majority of respondents in our case study sites were as yet little concerned with their obligations to account for themselves before the local OSC. This manager expressed some scepticism:
To be honest with you, I didn't really understand why we were held to account by the OSC because…especially if they don't understand the area of work that we're talking about. If you go in and talk about diagnostics and how we're going to reconfigure that in the health economy, really, they wouldn't really know what…so I think it's…I think it's useful for some things, the joint initiatives like…like the stability, transport and all those sort of things that kind of have a cross-cutting effect, but I'm not really sure that it's useful for the specific health issues. [manager ID 152]
Others were more positive, describing the O&S process as ‘helpful’ in the past in refining and developing plans.
Local Medical Committees
Finally, many of our CCGs were keen to include their LMC in discussions of their development plans. LMCs have no formal role in CCG development, but those we studied were aware that antagonising the LMC could carry significant consequences in terms of member engagement. Many utilised the LMC to organise the elections to their board, and continued to liaise and consult with the group. In one site, we witnessed a long discussion about the future relationship between the CCG and the local LMC. The LMC had requested regular formal meetings with the CCG governing body, but the CCG resisted this, agreeing that they should engage, but suggesting that frequent meetings would be unnecessarily burdensome. The CCG lay member commented: ‘now you (as GPs) are directly responsible, you are the accountable body and the LMC have no role to hold you to account’. Another group included this clause in their constitution:
The LMC
3.6.1 The CCG recognises [local] Local Medical Committee as the statutory representative body of general practice for provider purposes in relation to local primary care contracts. There will also be full observer status for the LMC on the CCG Governing Body and the Chair of the CCG will regularly attend meetings of the LMC by invitation to provide updates, briefings and respond to individual areas of concern. Other opportunities for engagement (such as Locality Link Members) will be set out in the member practice engagement strategy. The LMC also plays an important role in independently running the election process for Locality GP representation.’
Overlapping accountabilities
It is thus clear that CCGs are subject to a wide range of external accountabilities. The most clearly developed of these is the sanction-backed accountability to NHSE, but it is also clear that a wide range of other bodies feel that they have a role. The extent of these external accountabilities was experienced as problematic at times, with one manager commenting:
…there’s people in the rest of the NHS are trying to work out what their roles are. You know, I have had four demands this week from different places for a slightly different perspective report on the same topic, and not just a report but then turn up and tell them and assure them you’re doing something about it. And that’s just on the one topic. That’s the world we’re living in. And while you’re satisfying that world, it’s very difficult to focus on what your organisation should be doing. [manger ID 173]
Internal accountability
CCGs are membership organisations, and this is said to be one of the key strengths of the new structures.30 As such, there is a two-way accountability relationship between the CCG governing body and the general practices who are members, as well as accountabilities between the various working groups within the CCG.
Members’ accountability to the CCG
The CCGs in our study were clear that their practice members would be in an accountability relationship with the CCG, and this relationship was one in which the CCG would ‘hold General Practices to account’ for their behaviour, including such things as referral practices and prescribing. This manager described it thus:
Q: What would you claim to be the early success of a CCG? I mean you, how would you see it?
A: That’s a very good question [laughter]. I think… one of things it has done is it has got more GPs involved and more GPs talking to one another and looking at their referral patterns and realising that…they are accountable rather than it maybe just being one person for a practice being the person who goes to this meeting, comes back and everybody goes oh, well that’s fine and just ignores it. I think there is certainly an additional…almost accountability, a buy in from more GPs across the patch. [Manager ID 254]
In many sites the relationship between general practices and the wider group is governed by a written agreement, called an ‘accountability’ or ‘membership’ agreement:
If you're working as a CCG and you've…signed up to your accountability agreement and everyone's in it together, you can't have some General Practices overspending ridiculously and some desperately trying to make savings. You know, that's not…I don't think that's on. [GP ID 37]
These agreements were usually developed in addition to the CCG constitution, and set out mutual obligations within the group. Thus, for example, in site 3 the ‘membership agreement’ forms an appendix to the formal constitution of the group. It sets out what the CCG will provide for general practices (such as the provision of timely information, educational events and prescribing support) and stipulates the following practice obligations:
To share named information by practice for peer review;
To actively participate in demand management using specified tools;
To actively communicate with other members, the locality and the CCG as a whole;
To develop a framework for quality within the practice;
To agree and sign up to the terms of the Constitution;
If any member practice fails to meet agreed targets, they agree to work on and implement a development plan;
To provide a practice patient representative for the patient and public engagement body;
To name a practice lead for clinical commissioning;
To work on and implement care closer to home pathways;
To actively manage the devolved budget to assist financial balance and quality, innovation, productivity and prevention (QIPP);
To support robust and effective clinical, financial and operational risk management across the CCG (extract from membership agreement site 3).
Such agreements suggest a degree of voluntarism, by which general practices are ceding some sovereignty to the wider group, in return for receiving support and access to the resources of the group. However, CCG membership is compulsory for all general practices in England, so this voluntarism is in practice somewhat illusory.
A membership agreement had been drawn up (see associated documents). This has to be signed by all GPs. [GP lead] asked how best to go about this. He also pointed out that this agreement is not a legally binding document. After some discussion it was agreed to send out the document to practice managers and ask them to oversee the process and [manager] was asked to follow up those that did not return the signed agreement. [participant] asked if they should plan for those who refuse to sign. [GP lead] said: there is no choice! [Extract from fieldnotes, Locality meeting ID M54]
It also remains unclear what sanctions might apply, should general practices break the terms of these agreements. One CCG constitution suggests that general practices failing to keep to the agreement would have to ‘give an account’ first to their local peers, and subsequently to the CCG board, but no sanctions and timescales are specified. Such agreements must walk a fine line, as performance management of GPs with respect to their clinical practice will be the responsibility of NHSE, and there has been national concern to ensure that CCGs do not stray into this aspect of practice.31
Accountability to members
The formal accountability of the CCG to its constituent members is mainly promulgated through the accountability of its governing body to the members and of the specific officers of the CCG (being the Chair, Accountable Officer (AO) and Chief Financial Officer) to the CCG. One aspect of accountability is the ability to dismiss those who do not perform well. The general principle for CCGs is that members elect their governing body and chair for time limited terms, but the model constitution does not specify exactly how the governing body, officers and committees should be elected and dismissed, and there is some variation in how this has been arranged in the constitutions adopted in the study sites. The governing body is accountable to the members for the running of the CCG in accordance with its constitution. Clause 7.3.1. of the model constitution explains how
‘each member of the governing body should share responsibility as part of a team to ensure that the group exercises its functions effectively, efficiently and economically, with good governance and in accordance with the terms of this constitution’
The officers of the CCG are also accountable to the governing body of the CCG, and through that to the CCG membership. Each CCG's draft constitution sets out its own requirements for appointment and removal. For example, the chair in one site must be a ‘provider of primary medical services’ who is elected by ‘qualifying providers of primary medical services’. There is a 2-year to 4-year term, renewable to a maximum of 10 years. Some of the constitutions state circumstances in which the chair would be obliged to stand down, for example, in another site, if the chair
‘has behaved in a manner or exhibited conduct which has or is likely to be detrimental to the reputation and interest of the group and is likely to bring the group into disrepute. This includes but is not limited to dishonesty, misrepresentation (either knowingly or fraudulently), defamation of any member of the governing body, abuse of position, non declaration of a known conflict of interest, seeking to lead or manipulate a decision of the governing body in a manner that would ultimately be in favour of that person whether financially or otherwise;’
As might be expected as CCGs were in the process of establishing themselves, we witnessed a considerable discussion about these internal governance issues within the groups. In meetings and in interviews comments were made about the following accountabilities:
The CCG governing body is accountable to the members;
Locality groups are accountable to the governing body;
Subcommittees are accountable to the governing body;
Employed officers are accountable to the governing body.
Elected governing body members are accountable to the membership.
However, such discussions rarely included any mention of either the mechanisms by which such accountabilities would be promulgated, or the sanctions that might apply. In practice, our findings suggest that the main mechanism by which these accountabilities will be enforced is by information sharing and transparency, with governing bodies receiving reports from sub groups and localities, and in turn reporting on their activities to assemblies of members. This would seem to be a form of political accountability, with the respective groups making an argument and providing justifications for their actions, with no explicit performance measures and few available sanctions. The only area in which there would seem to be some possible formal sanctions is in the election/selection of officers such as Chair and AO, as discussed above. It is also conceivable that a CCG governing body which had lost the confidence of its membership might find that general practices informally withdrew their cooperation; whether the governing body could use its authority to prevent this is unclear.
Summary
Our study shows that CCGs are subject to a complex web of accountability relationships. The strongest form of accountability would seem to be their accountability to NHSE, backed by sanctions and subject to annual assessment. Furthermore, the currency of this accountability is clearly established, encompassing fiscal accountability and programme accountability for the CCGOIS. The accountability to other external bodies such as HWB is, by contrast, much weaker, and less clearly defined, with CCGs required to ‘give an account’, with no associated sanctions. Accountability to Monitor may be more formal, as it would seem that Monitor will be empowered to enforce competition law, although how this will operate in practice is as yet unclear. Accountability to the public is a political accountability, focused on the relatively weak notion of ‘transparency’, with no associated sanctions. Internal accountability is similarly complex, with a mix of mutual and one-way relationships, some accompanied by the ultimate sanction of voting out office holders. General practices are said to be ‘held to account’ if they transgress the rules of the group, but it is unclear as yet if they could be ejected, as all general practices must be a member of a CCG. These external accountabilities can be summarised in diagrammatic form (figure 1).
Figure 1.
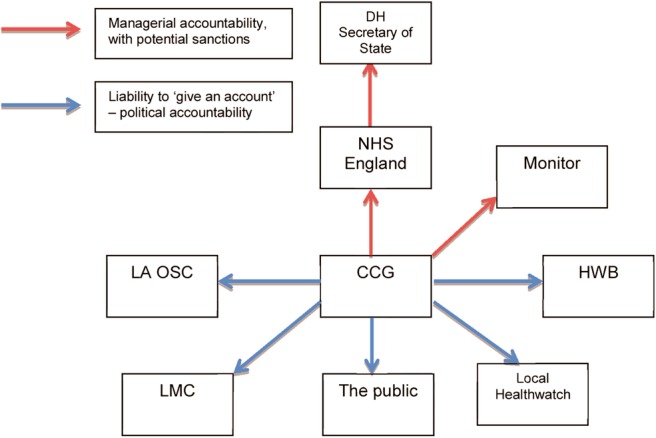
Clinical commissioning group external accountabilities. CCG, clinical commissioning group; DH, department of health; HWB, Health and Well-being Board; LA OSC, local authority overview and scrutiny committee; LMC, local medical committee; NHS, National Health Service.
Internal accountability relationships are similarly complex. Figure 2 summarises these, distinguishing between those bodies within CCGs which will hold each other to account and those which are accountable.
Figure 2.
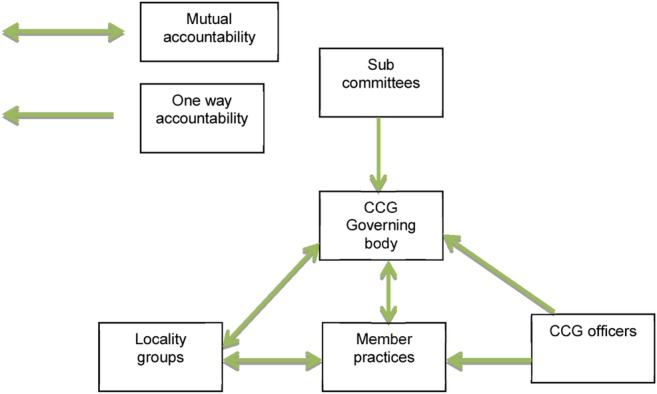
Clinical commissioning group internal accountabilities. CCG, clinical commissioning group.
Discussion
Principal findings and their implications
The HSCA 2012 promised ‘increased accountability’ as justification for the wide ranging NHS reforms in England. Our study suggests that CCGs will indeed be ‘more accountable’ than their predecessor organisations (PCTs) in the sense that they will be accountable to a much wider range of organisations and bodies of people. Indeed, we have shown that CCGs are at the centre of a complex web of accountability relationships, both internal and external. However, whether this translates into being more responsive, or more easily held to account, remains to be seen.
In general, studies suggest that complex accountability arrangements tend to generate confusion,32 and that, where organisations are accountable to multiple audiences, the interests of those audiences may differ, generating unintended consequences.33 This may be important for CCGs, as they attempt to balance the demands of the multiple audiences to whom they are being asked to account. We have shown that, as things stand, the accountability relationship with NHSE is the only one in which the currency and focus of accountability is clearly set out, although even this managerial accountability remains untested. However, our study participants also showed a keen commitment to other, more political forms of accountability, and it is possible that in future, CCGs will choose to satisfy their public audiences rather than NHSE or the DH. Thus, for example, NHSE has suggested that CCGs’ closeness to their members and their responsibility to account to local politicians via HWBs will make it easier to make difficult decisions about service reconfigurations34 but it is equally likely that CCGs accountable to local politicians and to local people via daily contacts in their surgeries will avoid such hard decisions in the face of public opposition. This latter interpretation is perhaps supported by evidence from other fields where such direct local accountability exists. Thus, for example, the introduction of directly elected Police and Crime Commissioners in the UK raised fears that the need to satisfy a local electorate may lead to a short-term focus on retaining popularity, rather than a longer term focus on strategic needs.35
Strengths and weaknesses
This study took place during the early phases of CCG establishment, and therefore provides a snap shot of a developing situation. However, the data collected were wide and deep, and the findings therefore provide a robust picture of the developing landscape of CCG accountability.
Comparison with previous studies
It is instructive to compare CCGs with their predecessor organisations, PCTs. PCTs were straightforwardly accountable (via a managerial accountability regime, backed by the sanction that senior individuals could lose their jobs) to their local Strategic Health Authority, who were, in turn, accountable to the Secretary of State. In addition, they had a duty to account to patients and the public, consulting them and providing information about their decisions. In practice, the strong accountability backed by personal sanctions for the senior executives drove the agenda, with studies highlighting the clear distinction between ‘must do’ actions, where one's job could be at risk, versus those which could be negotiated or modified.36 The potential distorting effect of this type of strong accountability has been well documented,37 and PCTs were generally held to be poorly accountable to their local populations.38 Senior staff in CCGs do not appear at present to be subject to personal sanctions in quite such an immediate way, and it will be interesting to explore over the coming months whether the threat of organisational sanctions will act to drive the agenda in a similar way. It also remains to be seen how far the early rhetorical commitment to public accountability that we found translates into meaningful activity.
It is too early for there to be any published empirical study of CCG accountability, although some commentaries have been published. In the most comprehensive of these, writing from a legal perspective, Davies39 argues that the complex additional accountabilities to which CCGs are subject may, in practice, act to dilute the important central accountability to parliament that the act is ostensibly designed to promote.
Unanswered questions
CCGs are responsible for significant amounts of public money, and it is important that they are subject to scrutiny as they develop their new ways of working. This study provides an early look on their developing accountability relationships, and highlights the complexity and potential problems which may arise. It is vital that further work follows these finding up and explores in depth the way in which the complex relationships identified here play out in practice over time. Ultimately, the extent to which CCGs are felt to be truly accountable for their work will be an important aspect of any overall judgement about the success of this significant reform programme.
Supplementary Material
Acknowledgments
The study formed part of the programme of the Policy Research Unit on Commissioning and the Healthcare System. The authors are grateful to their participants who were very generous in allowing access to their organisations at a time of considerable turmoil and change. A project advisory group provided valuable advice and support in the development and management of the study. The authors are also grateful to Ms Ros Miller and Dr Andrew Wallace who undertook much of the fieldwork for them and contributed to the analysis and final report. Employees of the Department of Health were members of an advisory group who supported the conduct of the research, and commented on an initial draft of the study final report, but the findings are those of the authors.
Footnotes
This body was initially called ‘the NHS Commissioning Board’ (NHSCB), but just prior to its formal establishment this was changed to NHS England.
CCGs are not formally established until they have been through the authorisation process. At the time of this research, CCGs were technically subcommittees of their local PCT, and should properly be referred to as ‘emerging’, ‘aspirant’ or ‘Pathfinder’ CCGs. However, in order to make the paper more readable, the term ‘emerging’ is omitted, using the shorthand of ‘CCG’ to refer to the groups putting themselves forward for authorisation.
Contributors: All of the authors meet the criteria for authorship, and were involved in the design and data analysis of the study, and contributed to the drafting, revision and finalisation of this article. In addition, JS, AC, IM, CP and KC took part in the data collection.
Funding: The Policy Research Unit in Commissioning and the Healthcare System (PRUComm), is funded by the Department of Health Policy Research Programme.
Competing interests: All of the authors received grant funding from the Department of Health via its Policy Research Programme for this research.
Ethics approval: The study received ethical approval from National Research Ethics Service North West ref 0375.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Department of Health Equity and excellence: liberating the NHS. London: The Stationary Office, 2010 [Google Scholar]
- 2.Cabinet Office The coalition: our programme for government. Freedom, fairness, responsibility. London: Cabinet Office, 2010 [Google Scholar]
- 3.Flynn R, Williams G. eds Contracting for health: quasi-markets and the NHS. Oxford: Oxford university Press, 1997 [Google Scholar]
- 4.Health and Social Care Act. Department of Health, 2012
- 5.NHS Commissioning Board Developing commissioning support: towards service excellence, 2012 [Google Scholar]
- 6.Department of Health A short guide to NHS Foundation Trusts. London: The Stationary Office, 2005 [Google Scholar]
- 7.NHS Commissioning Board Towards establishment: Creating responsive and accountable Clinical Commissioning Groups. 2012
- 8.Mulgan R. ‘Accountability’: an ever-expanding concept? Public Adm 2000;78:555 [Google Scholar]
- 9.Ryan C, Walsh P. Collaboration of public sector agencies: reporting and accountability challenges. Int J Public Sector Manag 2004;17:621–31 [Google Scholar]
- 10.Hood C. A public management for all seasons? Public Adm 1991;69:3–19 [Google Scholar]
- 11.Bovens M. Analysing and assessing accountability: a conceptual framework1. Eur Law J 2007;13:447–68 [Google Scholar]
- 12.Brinkerhoff DW. Accountability and health systems: toward conceptual clarity and policy relevance. Health Policy Plan 2004;19:371–9 [DOI] [PubMed] [Google Scholar]
- 13.Friedman A. Beyond accountability for reasonableness. Bioethics 2008;22:101–12 [DOI] [PubMed] [Google Scholar]
- 14.Yamin AE. Beyond compassion: the central role of accountability in applying a human rights framework to health. Health Hum Rights 2008;10:1–20 [PubMed] [Google Scholar]
- 15.Leat D. Voluntary organisations and accountability. London: Policy Analysis Unit, National Council for Voluntary Organisations, 1988 [Google Scholar]
- 16.Day P, Klein R. Accountabilities: five public services. London and New York: Tavistock, 1987 [Google Scholar]
- 17.Miller R, Peckham S, Checkland K, et al. Clinical engagement in primary care-led commissioning: a review of the evidence. London: Policy Research Unit in Commissioning and the Healthcare System (PRUComm), 2012 [Google Scholar]
- 18.Department of Health The Functions of GP Commissioning Consortia. A Working Document. Gateway ref 15472, 2011
- 19.Coleman A, Harrison S. What next for health scrutiny? J Integr Care 2013;21:54–63 [Google Scholar]
- 20.Checkland K, Coleman A, Segar J, et al. Exploring the early workings of emerging Clinical Commissioning Groups: final report. London: Policy Research Unit in Commissioning and the Healthcare System (PRUComm), 2012 [Google Scholar]
- 21.NHS Commissioning Board Model CCG Constitution Framework, 2012 [Google Scholar]
- 22.Department of Health The mandate: a mandate from the government to the NHS Commissioning Board. London: The Stationary Office, 2012 [Google Scholar]
- 23.NHS Commissioning Board Quality Premium: 2013/14 guidance for CCGs. Draft, 2012
- 24.McLellan A. Lansley expects ‘nearly all’ CCGs to be authorised by deadline. Health Serv J 2012. http://www.hsj.co.uk/news/policy/lansley-expects-nearly-all-ccgs-to-be-authorised-by-deadline/5045904.article#.Upce2cRcXS4 (accessed 28 Nov 2013). [Google Scholar]
- 25.Department of Health Developing Clinical Commissioning Groups: towards authorisation. London: The Stationary Office, Gateway Reference 16367, 2011 [Google Scholar]
- 26.Kaffash J. Revealed: CCG targets for quality premium. Pulse 18 Dec 2012
- 27.NHS Commissioning Board Clinical commissioning group governing body members: role outlines, attributes and skills. 2012 [Google Scholar]
- 28.Coleman A, Checkland K, Segar J, et al. Joining it up? Health and wellbeing in the new English National Health Service organisation: early evidence from Clinical Commissioning Groups and shadow Health and Wellbeing Boards. Local Government Studies In press [Google Scholar]
- 29.Department of Health Government response to the NHS Future Forum report CM8113, 2011
- 30.NHS Commissioning Board Clinical Commissioning Groups HR Guide. 2012 [Google Scholar]
- 31.Iacobucci G. CCGs ramp up performance management of GPs as thousands sign inter-practice agreements. Pulse;23 June 2012
- 32.Dixon A, Storey J, Alvarez Rosete A. Accountability of Foundation Trusts in the English NHS: views of Directors and Governors. J Health Serv Res Policy 2010;15:82–9 [DOI] [PubMed] [Google Scholar]
- 33.Davies A. Tangled web—accountability and the Commissioning Role in the New NHS. King's Coll Law J 2007;18:393 [Google Scholar]
- 34.NHS Commissioning Board Clinical commissioning group authorisation: draft guide for applicants. 2012
- 35.Sampson F. Hail to the chief?—how far does the introduction of elected Police Commissioners Herald a US-style politicization of policing for the UK? Policing 2012;6:4–15 [Google Scholar]
- 36.Macfarlane F, Exworthy M, Wilmott M, et al. Plus ça change, plus c'est la même chose: senior NHS managers’ narratives of restructuring. Sociol Health Illn 2011;33:914–29 [DOI] [PubMed] [Google Scholar]
- 37.Bevan G, Hamblin R. Hitting and missing targets by ambulance services for emergency calls: effects of different systems of performance measurement within the UK. J R Stat Soc 2009;172:161–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.South J. Rising to the challenge: a study of patient and public involvement in four primary care trusts. Prim Health Care Res Dev 2004;5:125–34 [Google Scholar]
- 39.Davies ACL. This time, it's for real: the Health and Social Care Act 2012. Mod Law Rev 2013;76:564–88 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


