Abstract
Introduction
Prostate embryonal rhabdomyosarcoma (ERMS) is a common tumour in infants and children, with a median occurrence age of 5 years, but it is rare in adults. It is characterized by a high degree of malignancy, both local rapid growth with formation of large pelvic masses, often leading to renal failure due to urethral obstruction, and systemic spread, commonly to the lungs, liver and bone. Several therapeutic approaches have been employed in the effort to treat prostate ERMS, but all of them have failed to gain a significant survival benefit in adult patients.
Case report
We report on a case of a stage IV prostate ERMS, approached with combined-modality treatment, with the administration of 5 courses of doxorubicin, ifosfamide and 2-mercaptoethane sulfonate sodium (mesna), and, subsequent radiotherapy to the prostatic bed (60 Gy/30 fxs). The patient remained free of progression of disease for about 1 year to finally experience a systemic relapse with multiple lung metastases and pleural effusion. The patient died for metastatic disease 27 months following the initial diagnosis.
Conclusion
While it remains questionable which therapeutic approach for prostate ERMS in adults is the most appropriate, our report demonstrates that a chemo-radiation combined treatment can control the prostate disease, reducing the symptoms and improving the quality of life of these patients, for the most part destined to die for systemic progression of disease.
Keywords: Prostate cancer, Embrional, Rhabdomyosarcoma, Adults, Radiation therapy
1. Background
Rhabdomyosarcoma (RMS) is the most frequent soft tissue tumour in paediatric patients, accounting for up to 50% of all soft tissue sarcomas.1 In adults RMS is very rare2 and clinical experience is limited to case reports. Three histological subtypes have been identified: embryonal with botryoid and alveolar histiotypes, generally affecting young children and adolescents,3 and the pleomorphic histiotype that is usually encountered in adult patients.2 This neoplasm has a mesenchymal origin, involves skeletal muscle, and therefore can be localized in almost any site. In paediatric patients, it is most frequently localized in the cervical-cephalic region and genito-urinary system; in adults, RMS involving the thorax and extremities accounts for 2–5% of all soft tissue sarcomas.4 The primary prostate embryonal rhabdomyosarcoma (ERMS) is rare in adults and its clinical manifestations, natural history, prognosis and treatment options can be found only in anecdotal descriptions. It is usually characterized by extensive loco-regional spread, with symptoms of urinary obstruction (due to bladder outlet obstacle), and a tendency to metastasize by blood stream and regional lymphatics and to give early lung and bone involvement.
Several therapeutic approaches have been employed in the management of ERMS of the prostate, such as radical surgery, radiotherapy and chemotherapy. This combined approach has significantly improved the outcome, in terms of survival and quality of life in children, while in adults the prognosis has been poor.
We herein present a case of 27-year-old male affected by stage IV ERMS of the prostate treated with a combined chemo-radiotherapy approach, resulting in a disease-free survival of 2 years and a good quality of life, with a complete remission of the urinary symptoms. Moreover, we provide a systematic overview of all reported cases available within the medical literature.
2. Case report
In October 2007, a 27-year-old male was referred to a practitioner because of dysuria and fever. Over the past three weeks, he had noticed occasional difficulty and increased frequency of micturition, as well as anorexia and weight loss. The patient started treatment with antibiotic but, after 2 days, he was hospitalized with clinical signs and symptoms of acute urinary retention. On catheterisation, 800 ml of urine could be rescued. Physical examination was unremarkable, except for digital rectal examination which revealed an uneven swollen and enlarged prostate gland of stony-hard consistency with an irregular capsule profile.
His family history was irrelevant. The patient had been healthy until the time of our observation and denied venereal infection, allergy and the use of alcohol and tobacco.
A complete diagnostic work-up was planned. Laboratory data were unremarkable. Blood chemistry showed normal levels of prostate-specific antigen (PSA). Urine examinations showed a heavy trace of albumin and many red blood cells. An abdominal computed tomography (CT) scan was then performed, disclosing a large mass (62 mm × 50 mm × 61 mm) of prostatic origin filling the pelvis, with disruption of the prostate anatomy and suspected infiltration of bladder base and rectal wall (Fig. 1). No enlarged lymph nodes were detected at any abdominal site. Chest CT images showed multiple (>20) bilateral nodular densities with maximum diameter of 1 cm, of clear metastatic nature (Fig. 1). Pelvic magnetic resonance (MR) study confirmed the CT findings. The pathological mass replaced the entire prostate gland, destroyed the seminal vesicles and infiltrated the recto-vesical space and rectal wall. A subsequent FDG-positron emission tomography (PET) scan was performed and revealed prostate and bilateral lung pathological uptake; no signs of other sites of disease, as reported in Fig. 2.
Fig. 1.
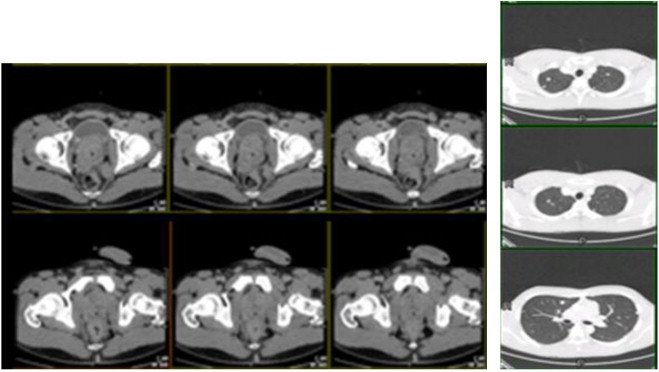
Total body TC at diagnosis: massive enlargement of prostate gland and multiple nodules in both lungs.
Fig. 2.

CT/PET scan at diagnosis: prostate and bilateral lung pathological uptake.
A prostate transrectal biopsy was performed and histology showed sheets of multinucleated cells in addition to small round cells. The round cells demonstrated immunohistochemical positivity for muscle-specific markers, such as myoglobin, actin and desmin and negativity for citocheratine (AE1/AE3), CD34, S100 protein and PSA. Proliferation index, evaluated with Ki67/MIB1 antibodies, was high (>30%). This account was referable to ERMS of the prostate, classified as high-risk, according to the criteria of the Intergroup Rhabdomyosarcoma Study Group (IRSG).
A surgeon oncologist was consulted, and because of the local extension to rectal wall the tumour was regarded as primary unresectable. Thus, also in view of the metastatic diffusion, the patient underwent first-line chemotherapy, with doxorubicin 25 mg/mq/die d 1, 2, 3, ifosfamide 2000 mg/mq/die in 2 h d 1, 2, 3, 4, 5, and 2-mercaptoethane sulfonate sodium (mesna) for 5 cycles. After chemotherapy completion, CT and CT/PET showed a complete remission of pulmonary disease and partial response of the prostate mass.
Subsequently, the patient underwent a full course of intensity modulated radiation therapy (IMRT) with Tomotherapy Hi-Art, up to 60 Gy in 30 fractions to the prostate bed. Treatment was well tolerated, without acute toxicity.
After therapy had been completed, the patient was periodically controlled, with a clinical and radiological follow-up. A CT-scan, performed every 3 months, revealed a major downsizing of the prostate tumour and persistent complete remission of the multiple pulmonary nodules. Pelvic CT-scan images, performed 6 months after RT completion, are shown in Fig. 3. The patient remained free from progression of disease for 17 months without urinary symptoms and with a good quality of life.
Fig. 3.
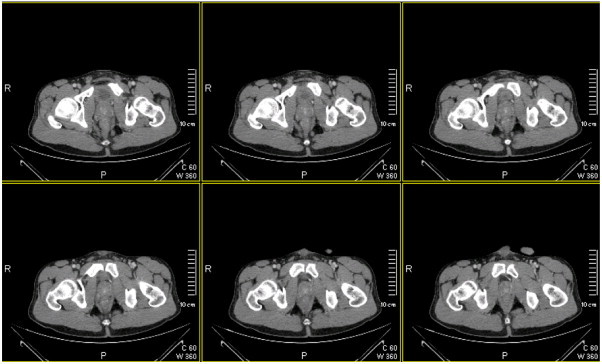
Pelvic CT scan 6 months after radiotherapy completion: reduction of prostate mass.
Unfortunately, at 17 months following the radiotherapy completion, he developed symptoms of fatigue, dyspnoea and pain in the right thorax. CT scan (Fig. 4) revealed multiple lung metastases with pleural effusion. No response was seen to palliative chemotherapy (Ecteinascidin-743) and the patient died for metastatic disease (pulmonary failure) 27 months following the initial diagnosis.
Fig. 4.
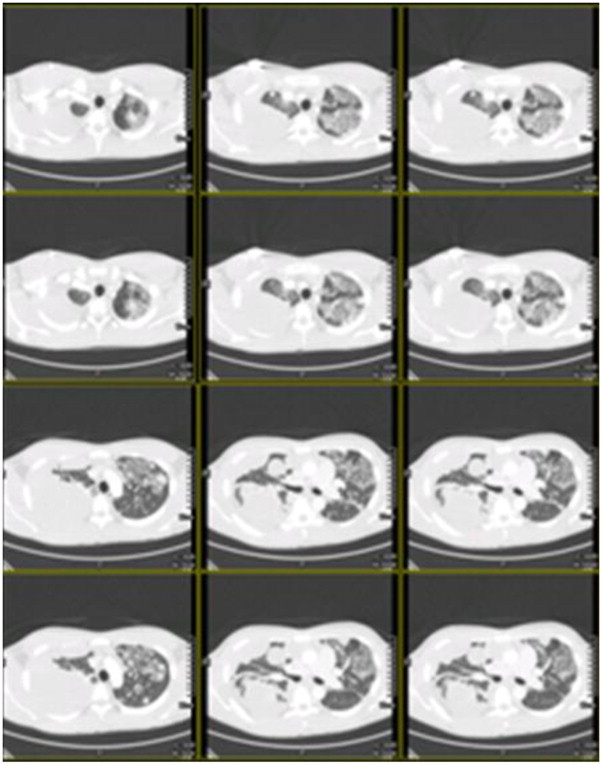
Total body CT scan at moment of progression disease: appearance of multiple nodules in bilateral lung and large bilateral pleural effusion and diffuse pulmonary lymphangitis carcinomatosa.
3. Discussion
Primary ERMS of the prostate gland is an extremely rare pathological and clinical entity in adults,5 with fewer than twelve cases reported in literature.6 The natural history of the prostate RSM, deduced from the few cases published in literature, is characterized by a rapid growth, with the typical formation of large pelvic or abdominal masses, often leading to renal failure due to bilateral urethral/ureteral obstruction. The tumour often disseminates widely, mainly to the lungs, bone, liver, and serosal surfaces and, unlike most other sarcomas, regional lymph node metastases are common. The presenting symptoms are often related to urethral obstruction, with frequency, hesitancy, and dysuria as predominant symptoms or, less often, with hematuria and acute urinary retention. In some patients, the compression of the rectum can cause constipation, rectal bleeding and a sense of rectal fullness.7
There is no pathognomonic radiological finding for prostate ERMS. CT scan and MRI study reveal a large soft tissue mass with areas of necrosis replacing the whole prostate, but the radiological differential diagnosis with prostate adenocarcinoma can be very difficult. The mass may invade periurethral and perivesical tissue or it may extend into the ischiorectal fossa. Calcifications are rare. MRI can clearly show the site of origin as the central prostate area, with compression of a recognizable peripheral portion. The mass can display a well-defined low signal intensity pseudocapsule in T2 weighted images and a heterogeneous enhancement in post-Gadolinium T1 weighted images. The utilization of PET-CT for ESRM staging in adults is still to be consolidated in the literature, however, some reports have demonstrated the relevance of this method in the detection of the primary focus in metastatic disease or obscure metastases.
The diagnosis is usually performed with a transurethral, transrectal or perineal biopsy. Histopathological evaluation can reveal variable grade of differentiation along the myogenesis pathway, and strap cells or myotubes may appear. In well-differentiated ERMS, the recognition of rhabdomyoblasts directs the pathologist to the correct diagnosis, above all when the combined light and electron microscopic studies have been used. In the major part of cases, immunohistochemistry for skeletal muscle specific markers, such as antisera against myoglobin and skeletal muscle actin and myosin, can help identify the tumour as rhabdomyosarcoma.
In children, the treatment and prognosis of rhabdomyosarcoma of the urogenital tract have changed dramatically over the past few decades. Until the 1970s radical prostatectomy was the only therapeutic option. Since then, multiagent chemotherapy has achieved remarkable cure rates, with the goal to improve patients’ quality of life.
In adults, rhabdomyosarcoma of the prostate is a very rare malignancy with a poor prognosis secondary to aggressiveness of tumour growth, lack of early symptoms and late presentation. Moreover, 25% of prostate ESRM patients show distant metastases at the time of diagnosis. The treatment option largely depends on the disease stage at the time of appearance. A localized prostate disease can be treated with radical surgery.8,9 Unfortunately, prostate rhabdomyosarcoma is often caught late in the disease process, and the tumour size at time of surgical resection is commonly too extensive, as in our patient's case. Patients with non-metastatic large prostate ERMS, which is not initially resectable, can be treated with neo-adjuvant chemo-radiation therapy.
Conversely, the impact and optimal timing of local therapy for metastatic disease is unknown. A recent study showed that, for metastatic rhabdomyosarcoma, radiotherapy was the only significant factor in improved progression free survival and overall survival.10 In the 25 patients with metastatic disease, median progression free survival times in patients with or without local therapy (surgery and/or radiotherapy) were 13.4 versus 7.0 months (p < 0.001), respectively, and median overall survival times were 36.1 versus 7.6 months (p < 0.001), respectively. Then, the local therapy to the primary tumour site during the treatment approach may be necessary for metastatic rhabdomyosarcoma, as the patients who received local therapies showed significantly longer survival than those who did not. Obviously, the timing of local therapy should be individually determined depending on patient conditions and characteristics.
Lee et al.11 recently reported a retrospective review of 48 patients with urological sarcoma treated with a multidisciplinary therapy. The results of this study suggest that any type of local approach (surgery or radiotherapy) can provide the best chance of survival in patients with or without metastasis.
In a recent review, Ashlock and colleagues reported an improvement of the outcome, in terms of survival and quality of life in children treated with a multimodality therapy. Nevertheless, in adults the prognosis remains poor, despite a good initial response to chemotherapy, with all patients dying of disseminated disease within 16 months from the diagnosis (mean survival, 8 months).12
To date, there is no consensus policy on the treatment of prostate rhabdomyosarcoma of the adult, due to the small number of cases reported in the literature and to enormous variability of its management.
Ewing et al.13 reported 3 cases of prostate RMS in young adults and Culver14 4 cases of ERMS in a series of 76 patients affected by primary prostate sarcomas. Katzmann et al.15 published a paper on 30 cases of prostate malignant sarcoma, among which there were 3 cases of RMS. Recently, Nabi et al.16 reported two cases of adults prostate ERMS with poor prognosis for both. In addition, Esnaola et al.17 reported, in a series of 30 adults with rhabdomyosarcoma, seven patients affected by prostate rhabdomyosarcoma, four of which were submitted to radical surgery and three to radio-chemotherapy. In this report, there were no 5-year survivors among patients with prostate tumours, whereas the 5-year-survival rates were 42%, 42% and 15% for head and neck, extremity and truncal localizations, respectively. Previous series of adults with prostatic rhabdomyosarcoma have reported similarly poor results, suggesting that the natural history of genitourinary tract tumours is significantly different in these patients in comparison to children, independently from the therapeutic approach.6,18
It appears evident that no definitive conclusions can be drawn up to now regarding the best available treatment option towards prostate ERMS in adults. Nonetheless, certain features might be noteworthy.
In a clinical situation of an organ-confined disease, radical surgical extirpation should be performed. The extent of the surgical procedure remains unclear. In contrast, in the case of locally advanced disease the surgery can lead to severe impairment of function and its therapeutic gain is questionable. Furthermore, it should be considered that most of the non-metastatic patients die in a short time for systemic spread of disease, even if locally treated. As alternative to surgery, radiation therapy combined with chemotherapy might be useful to achieve local control with organ functional preservation and good quality of life. In our experience, RT resulted in an effective approach in a prostate ERMS adult patient with advanced disease. The delivered dose of 60 Gy was able to control locally the disease without toxicity. The chemotherapeutic schema adopted in our patient (doxorubicin ifosfamide, mesna) was initially useful, but the most effective drugs to be used have yet to be established.
More data and further studies are needed in the future in order to improve the understanding of biological behaviour of prostate ERMS in adults and to define the most appropriate therapeutic approach, as well as the timing of local therapy in metastatic disease.
Conflict of interest
All authors disclose no actual or potential conflict of interest including any financial, personal or other relationships with other people or organizations that could inappropriately influence their work.
Financial disclosure
None declared.
References
- 1.Garay M., Chernicoff M., Moreno S., Pizzi de Parra N., Oliva J., Apréa G. Rabdomiosarcoma alveolare congenito in un neonato. Eur J Pediatr Dermatol. 2004;14:9–12. [Google Scholar]
- 2.Little D.J., Ballo M.T., Zagars G.K. Adult rhabdomyosarcoma. Outcome following multimodality treatment. Cancer. 2002;95:377–388. doi: 10.1002/cncr.10669. [DOI] [PubMed] [Google Scholar]
- 3.Hicks J., Flaitz C. Rhabdomyosarcoma of the head and neck in children. Oral Oncol. 2002;38:450–459. doi: 10.1016/s1368-8375(01)00105-1. [DOI] [PubMed] [Google Scholar]
- 4.Hawkins W.G., Hoos A., Antonescu C.R. Clinicopathologic analysis of patients with adult rhabdomyosarcoma. Cancer. 2001;91:794–803. [PubMed] [Google Scholar]
- 5.Batsakis J.G. Urogenital rhabdomyosarcoma: histiogenesis and classification. J Urol. 1963;90:180–186. doi: 10.1016/S0022-5347(17)64385-4. [DOI] [PubMed] [Google Scholar]
- 6.Waring P.M., Newland R.C. Prostatic embryonal rhabdomyosarcoma in adults. A clinicopathologic review. Cancer. 1992;69:755–762. doi: 10.1002/1097-0142(19920201)69:3<755::aid-cncr2820690324>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 7.Tannenbaum M. Sarcomas of the prostate gland. Urology. 1975;5:810–814. doi: 10.1016/0090-4295(75)90363-5. [DOI] [PubMed] [Google Scholar]
- 8.Russo P., Brady M.S., Colon K. Adult urological sarcoma. J Urol. 1992;147:1032–1037. doi: 10.1016/s0022-5347(17)37456-6. [DOI] [PubMed] [Google Scholar]
- 9.Stojadinovic A., Leung D.H., Hoos A. Analysis of the prognostic significance of microscopic margins in 2.084 localised primary adult soft tissue sarcomas. Ann Surg. 2002;235:424–434. doi: 10.1097/00000658-200203000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kojima Y., Hashimoto K., Ando M. Clinical outcomes of adult and childhood rhabdomyosarcoma treated with vincristine, d-actinomycin, and cyclophosphamide chemotherapy. J Cancer Res Clin Oncol. 2012;138:1249–1257. doi: 10.1007/s00432-012-1199-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee G., Lee S.Y., Seo S. Prognostic factors and clinical outcomes of urological soft tissue sarcomas. Korean J Urol. 2011;52:669–673. doi: 10.4111/kju.2011.52.10.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ashlock R., Johnostone P.A. Treatment modalities of bladder/prostate rhabdomyosarcoma: a review. Prostate Cancer Prostatic Dis. 2003;6:112–120. doi: 10.1038/sj.pcan.4500652. [DOI] [PubMed] [Google Scholar]
- 13.Ewing J. 3rd ed. W.B. Saunders Company; Philadelphia: 1928. Neoplastic diseases; pp. 234–239. 832. [Google Scholar]
- 14.Culver H. Sarcoma of the prostate. J Urol. 1925;14:47–55. [Google Scholar]
- 15.Katzmann Kurt. Beitrag zur Kenntnis von malignen Rhabdomyomen der kindlichen Prostata. Frankufurt Ztscher f Path. 1931;4:297–305. [Google Scholar]
- 16.Nabi G., Dinda A.K., Dogra P.N. Int Urol Nephrol. 2002;34:531–534. doi: 10.1023/a:1025638711476. [DOI] [PubMed] [Google Scholar]
- 17.Esnaola N.F., Rubin B.P., Baldini E.H. Response to chemotherapy and predictors of survival in adult rhabdomyosarcoma. Ann Surg. 2001;234:215–223. doi: 10.1097/00000658-200108000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Russo P. Urologic sarcoma in adults: Memorial Sloan-Kattering Cancer Center experience based on prospective database between 1982 and 1989. Urol Clin North Am. 1991;18:581–588. [PubMed] [Google Scholar]


