Abstract
This article is a summary of the conference “Clinical and technological transition in breast cancer” that took place in the Congress of the Spanish Society of Radiation Oncology, placed in Vigo (Spain) on June 21, 2013. Hugo Marsiglia and Philip Poortmanns were the speakers, the first discussed about “Clinical and technological transition” and the second about “EORTC clinical trials and protocols”.
Keywords: Breast cancer, Radiotherapy, Technological, Clinical trial
1. Introduction
Technological advances lived in the field of radiation therapy (RT), over the last decades have led us to have volume delineation, dose calculation and treatment units toward much more accurate treatment. With them we get more appropriate radiation dose to the level we want to treat. This unquestioned fact has caused that these new technologies will be adopted as standard without demonstrating their superiority in clinical trials. On the other hand, for the advance in knowledge of volumes that should be treated, which dose should receive or the best suitable fractionation, we need to have sufficient scientific evidence to support our treatment protocols. In this article we review the introduction of new technologies and most relevant clinical trials that are changing clinical practice in irradiation of breast cancer patients.
2. Clinical and technological transition
Radiation oncology is a field that has rapidly advanced over the last century. It holds a rich tradition of clinical care and evidence-based practice, and more recently has advanced with revolutionary innovations in technology and computer science [1]. Perhaps the most attractive feature of recent technological advances is the ability to approach any complex tumor geometry, regardless of shape, with an enhanced ability to optimize the dose distribution.
2.1. Accelerated partial breast irradiation
APBI can be successfully delivered using different radiation techniques (IMRT, brachytherapy, arc therapy, etc.) [2]. For instance, the University of Florence [3] evaluated with a randomized clinical trial the possibility of treating the index quadrant with IMRT in a selected group of patients with early-stage breast cancer. From 2005 to 2008, 259 patients were randomized and treated. The mean value of the ratio between the planning target volume and the ipsilateral breast volume was 21%. The rate of grade 1 acute skin toxicity was 22% and grade 2 was 19%.
Recent reports from the American Society for Radiation Oncology (ASTRO) and the Groupe Européen de Curiethérapie-European Society for Therapeutic Radiology and Oncology (GEC-ESTRO) have suggested selection criteria for “suitable patients” who could receive APBI outside of clinical trials [4]. Currently, there are 6 ongoing phase III trials. All are characterized by a significant heterogeneity regarding inclusion criteria and stratification factors. The French UNICANCER trial (SHARE; ClinicalTrials.gov identifier NCT01247233) will randomize 2800 patients in 3 arms: APBI (1 week) using 3-dimensional (3D) conformal radiotherapy, standard radiotherapy (6.5 weeks), and hypofractionated radiotherapy (3 weeks).
2.2. Arc dynamic therapy
Tomotherapy is a technique capable of delivering a well tolerated treatment with high homogeneity and coverage indexes and high capabilities for sparing the organs at risk [5,6], especially in patients with anatomically complex breast cancer, bilateral breast cancer or indication for internal mammary chain node irradiation. A Spanish report [7] described early clinical results of tomotherapy treatment in patients with breast cancer and complex treatment volumes. Ten patients were treated with tomotherapy between January 2009 and March 2010. All treatments included daily CT/megavoltage image guidance. The median homogeneity index was 1.09; and the median coverage index 0.81. Median V20 Gy and V10 Gy for ipsilateral lung was 20% and 37.1% respectively. Median V25 and V35 for heart was 15% and 4% respectively. Median dose for contralateral breast was 7 Gy. Skin acute toxicity was grade 1 in 41.7% and grade 2 in 58.3%.
Versmessen et al. [8] compared Health-related quality of life (HRQOL) in stage I–II breast cancer patients who were randomized to receive either conventional radiotherapy or hypofractionated tomotherapy. A total of 121 stage I–II breast cancer patients who had undergone breast conserving surgery or mastectomy were randomly assigned to receive either conventional radiotherapy or hypofractionated tomotherapy. Conventional radiotherapy patients received 25 × 2 Gy over 5 weeks, and breast conserving surgery patients also received a sequential boost of 8 × 2 Gy over 2 weeks. Hypofractionated tomotherapy patients received 15 × 2.8 Gy over 3 weeks, and breast conserving surgery patients also received a simultaneous integrated boost of 15 × 0.6 Gy over 3 weeks. Patients completed the EORTC (European Organization for Research and Treatment of Cancer) QLQ-C30 and BR23 questionnaires. Hypofractionated tomotherapy patients had a better improvement in global health status and role- and cognitive-functioning, and a faster recovery from fatigue, than conventional radiotherapy patients. These results suggested that a shorter fractionation schedule may reduce the adverse effects of treatment.
2.3. Intensity-modulated radiation therapy
Intensity-modulated radiation therapy can reduce radiation dose exposure to normal tissues while maintaining reasonable target homogeneity [9]. Jin et al. [10] compared the dosimetry for the left-sided breast cancer treatment using different radiotherapy techniques. Twenty patients with left sided breast cancer were planned using five different radiotherapy techniques, including: 1) conventional tangential wedge-based fields (TW); 2) field-in-field (FIF) technique; 3) tangential inverse planning intensity-modulated radiation therapy (T-IMRT); 4) multi-field IMRT (M-IMRT); and 5) volumetric modulated arc therapy (VMAT). The planning tumor volume dose prescribed was 50 Gy and V47.5 ≧ 95%. The same dose constraints were used for all five plans. The planned volumetric dose of PTV and organ at risk volumes (OARVs) were compared and analyzed. T-IMRT plan improved the PTV dose homogeneity index (HI) by 0.02 and 0.03 when compared to TW plan and VMAT plan, and decreased the V5, V10 and V20 of all OARVs. However, the high dose volume (≧30 Gy) of the OARVs in T-IMRT plan had no statistically significant difference compared with the other two inverse plans. In all five plans, the dose volume of coronary artery area showed a strong correlation to the dose volume of the heart (the correlation coefficients were 0.993, 0.996, 1.000, 0.995 and 0.986 respectively).
In order to increase the workload efficiency, a Canadian group [11] developed a template-based breast IMRT technique (TB-IMRT). TB- IMRT provided reduction of planning time compared with conventional breast radiation (14.0 vs 39.0 min, p < 0.001) and minimized the use of high energy beams, while providing similar treatment times and equal plans compared to conventional breast radiation.
2.4. Brachytherapy
The different indications of breast brachytherapy include all the breast irradiations focusing on the initial tumor bed (partial irradiation of the breast), such as boost, APBI and second conservative radiosurgical treatment in case of ipsilateral in-breast recurrence. Interstitial breast brachytherapy, performed according with the standard rules, remains a major technique for breast cancer treatment [12].
Partial breast brachytherapy and whole breast irradiation (WBI) has shown similar recurrence-free and overall survival rates in elderly breast cancer patients [13], even after adjustment for potential confusing factors. A sample of 29,647 female patients diagnosed with nonmetastatic breast cancer in 2002–2007 treated with breast-conserving surgery and radiotherapy was identified in the Surveillance, Epidemiology, and End Results Program-Medicare data set [13]. Recurrence-free survival and overall survival rates did not differ significantly between the two radiation modalities. After accounting for tumor characteristics, patient characteristics, community factors, and comorbidities, the recurrence-free survival (hazard ratio, 1.05; 95% confidence interval, 0.90–1.23; p = 0.5125) and overall survival (hazard ratio, 0.87; 95% confidence interval, 0.72–1.04; p = 0.1332) rates were still not significantly different between patients treated with APBI- brachytherapy and WBI.
Hannoun-Levi et al. [14] prospectively evaluated 40 patients aged >70 years, T1-2 <30 mm, and pN0 treated with APBI by means of high-dose rate-brachytherapy from July 2004 to April 2008. The total delivered dose was 34 Gy of 10 fractions for 5 days. Median Quality Index was 13.3% (1–70%). It was considered acceptable, partially acceptable, and nonacceptable in 10, 28, and 2 patients, respectively. Within 12 months after APBI, overall rates of toxicity were 59%, 28%, and 2% for Grade 1, 2, and 3 events, respectively. Twelve months after APBI, 35 patients (87%) achieved excellent/good cosmetic result. Compared with baseline values, Activity of Daily Living and Instrumental Activity of Daily Living scores remained unchanged 6 and 12 months after APBI. Therefore, APBI by means of high-dose rate-brachytherapy seemed to have an significant negative impact on functional dependence in the treatment of elderly women with early breast cancer.
2.5. Intraoperative electron radiotherapy
Although this technique is not widely available, IOERT followed by external beam radiotherapy allows for the delivery of a high dose to the tumor bed and an adequate dose to the whole breast [15]. This treatment is feasible, compliance is high, and the preliminary data on chronic toxicity seems acceptable. Ivaldi et al. [16] reported the acute and preliminary data on late toxicity of a pilot study of boost with IOERT followed by hypofractionated external beam radiotherapy of the whole breast performed between June 2004 and March 2007. In that study, 108 women with a diagnosis of early-stage breast cancer were treated with breast-conserving surgery and evaluated for late toxicity. During surgery, an IOERT boost of 12 Gy was administered to the tumor bed. Adjuvant local treatment was completed with hypofractionated external beam radiotherapy, consisting of a course of 13 daily fractions of 2.85 Gy to the whole breast to a total dose of 37.05 Gy. The recorded late skin toxicity was Grade 4 in 1 patient (0.9%), Grade 3 in 1 patient, and Grade 2 or less in 106 patients (98.2%).
The Rambam Health Care Campus in Haifa [17] began utilizing IOERT in 2006. From April 2006 to September 2010, 31 patients affected by unifocal invasive duct breast carcinoma ≦2 cm diameter received wide local resection followed by IOERT. After a mean follow-up of 36 months, seven patients developed mild breast fibrosis and three suffered from mild postoperative infection. Rib fractures were observed in four patients before routine lead shielding was initiated. Additional whole-breast irradiation was given to four patients. None of the patients developed local recurrences or other ipsilateral cancers. Similarly, no contralateral cancers or distant metastases were observed.
The University of North Carolina [18] conducted a phase 2 study of pre-excision IOERT for early-stage breast cancer. A total of 53 patients ≥48 years of age (median age was 63 years) with invasive ductal carcinoma, ≤3 cm (median tumor size was 1.2 cm), and clinically node-negative received IOERT. Ultrasound was used to select electron energy and cone size to cover the tumor plus 1.5- to 2.0-cm lateral margins and 1-cm-deep margins (90% isodose). Fifteen Gy was delivered with a Mobetron irradiator, and immediate needle-localized partial mastectomy followed. Of all patients, 81% were positive for estrogen receptor or progesterone receptor, 11% were positive for human epidermal growth factor receptor 2, and 15% were triple-negative. Also, 42%, 49%, and 9% would have fallen into the Suitable, Cautionary, and Unsuitable groups, respectively, of the American Society of Therapeutic Radiation Oncology consensus statement for accelerated partial breast irradiation. With a median follow-up of 69 months, ipsilateral events occurred in 8 of 53 patients and the 6-year actuarial rate of ipsilateral events was 15% (95% confidence interval = 7%-29%). The crude event rate for Suitable and Cautionary groups was 1 of 22 (5%) and 7 of 26 (27%), respectively. Overall survival was 94.4%, and breast cancer-specific survival was 100%. Therefore, the rate of local events was a matter of concern, especially in the Cautionary group. On the basis of these findings, pre-excision IOERT may not provide adequate local control for less favorable early-stage breast cancers.
In summary, the clinical and technological transition in breast cancer management experienced in the last decades offers a diverse array of advanced technologies and treatment techniques [19]. This variety of options allows us to offer the more optimal treatment for each patient according to clinical, pathological, and patient preferences. The knowledge of this novel technology should be incorporated in the educational programs.
3. EORTC clinical trials and protocols
Over the last decades, the EORTC Radiation Oncology and Breast Cancer Groups have conducted a number of practice-changing randomized phase III studies in the field of loco-regional treatment for breast cancer. These studies have contributed to building evidence for the ability of RT to improve loco-regional control, which in turn is translated into a long-term survival benefit for the patients. This knowledge highlights the key role that radiation oncology plays in the multidisciplinary management of cancer patients. Apart from the trials focussing on loco-regional management, several others have been conducted in the field of breast cancer focussing on systemic therapy.
3.1. Breast conserving treatment
One of the randomized clinical trials that has shown equivalent results after breast-conserving therapy (BCT) and after modified radical mastectomy (MRM) in stage I and II breast cancer was EORTC 10801, for which recently an update after a median follow up of 22.1 years was conducted [20]. Compared with BCT, MRM resulted in a better local control, but did not significantly affect time to distant metastases (which was the primary endpoint of this trial). Cumulative incidence of distant metastases and overall survival were similar in both groups as well. The results were similar for both patients younger and older than 50 years. The meta-analysis of the Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) confirmed the equivalence of BCT and MRM with survival as endpoint [21]. It also demonstrated the need for RT following lumpectomy to reduce the 5-year local recurrence rate from 26 to 7% and to improve long term survival [22]. Therefore, BCT, including RT, is accepted as standard care for patients with early stage breast cancer.
The cosmetic outcome after BCT as given in trial 10801 could often be considered as suboptimal. As a possible relation with the higher dose (boost) of 25 Gy to the primary tumor bed was suggested, the subsequent EORTC “Boost-no-boost” 22881/10882 trial investigated the potential impact of the boost on local control and on treatment complications. This was done in two parallel prospective randomized trials. After a microscopically complete resection –as stated by the local pathologist- 5318 patients were randomized between either a 16 Gy boost or no boost to the primary tumor bed after 50 Gy of WBI. This clearly demonstrated that the boost dose significantly reduces the local recurrence rate [23]. Whereas the absolute reduction of the local recurrence rate by nearly 50% could be demonstrated in all patient subgroups, especially age turned out to be a very important prognostic factor for the absolute benefit as the local recurrence rate was demonstrated to be inversely related to age, as displayed in Fig. 1 [24]. The presence of DCIS (Ductal carcinoma in situ), tumor size, tumor grade and the administration of adjuvant systemic treatment were other prognostic factors for local control after BCT [25]. Based on these results, a nomogram was designed and made available at http://research.nki.nl/ibr/ [26]. In the much smaller group of 251 patients that was randomized after a microscopically incomplete resection –again as stated by the local pathologist – between either a 26 Gy boost or a 10 Gy boost, no significant difference could be found [27].
Fig. 1.
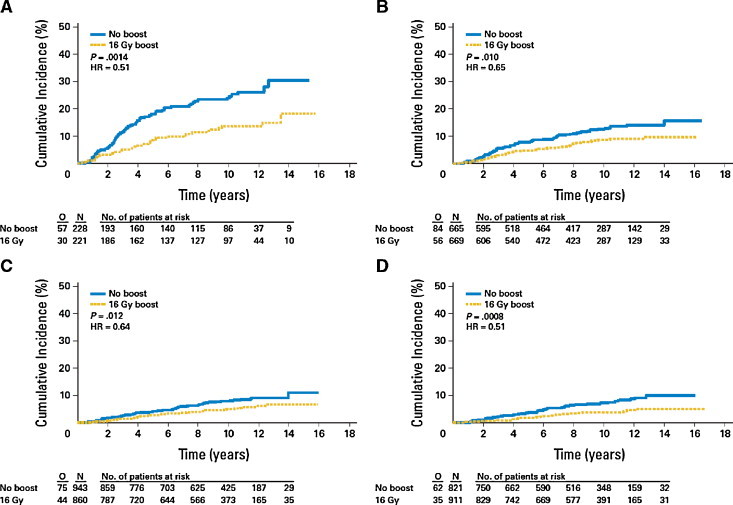
Cumulative incidence of ipsilateral breast cancer recurrence according to age. Age (A) ≤40, (B) 41–50, (C) 51–60, and (D) ≥60 years. HR, hazard ratio; O, occurrences; N, number of patients at risk.
Reproduced with permission from Bartelink H, Horiot JC, Poortmans PM, et al. Impact of a higher radiation dose on local control and survival in breast-conserving therapy of early breast cancer: 10-year results of the randomized boost versus no boost eortc 22881-10882 trial. J Clin Oncol 2007; 25(22): 3259–3265.
Remarkably, we could not find an association between positive resection margins –as based on central pathology review- and the risk of local recurrence after BCT [25]. Of note is that this subgroup analysis only involved patients that were considered as having a complete excision by the local pathologist.
Apart from disease outcome parameters, we scored the rate of fibrosis at the whole breast and at the primary tumor site at each follow up visit. The boost dose significantly increased the development of fibrosis in both the whole breast and the boost area. A clear dose-effect relation for fibrosis was seen, as displayed in Fig. 2 [28]. It remained, however, of minor or moderate severity in most patients. Based on this, we developed nomograms to predict the impact of a boost dose of 16 Gy on the risk for developing fibrosis at any site in the breast, also available at the same internet site (http://research.nki.nl/ibr) [26,28].
Fig. 2.
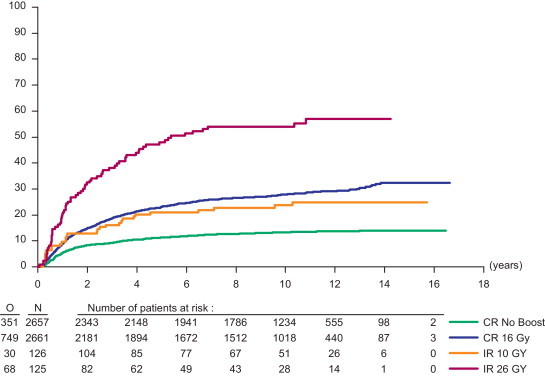
Cumulative incidence of moderate or severe fibrosis after 50 Gy whole breast irradiation, followed by no boost or a boost dose of 10 Gy, 16 Gy and 26 Gy, respectively. O, observed; N, number of patients at risk; CR, complete resection; IR, incomplete resection.
Reproduced with permission from Collette S, Collette L. Budiharto T, et al. Predictors of the risk of fibrosis at 10 years after breast conserving therapy for early breast cancer: a study based on the EORTC trial 22881-10882 “boost versus no boost”. Eur J Cancer 2008; 44: 2587–2599.
Moreover, a cosmetic evaluation was performed with pictures taken at randomization and every 3 years thereafter. The cosmetic result was scored as excellent to good in 86% of the patients without a boost and in 71% of the patients with a boost [29]. Apart from the boost, other independent predictive factors for a worse cosmetic outcome were a location of the primary tumor in the lower quadrants of the breast, the size of the excision specimen, the occurrence of a breast infection and/or a hematoma, and larger tumor size [30]. An inhomogeneous dose distribution of WBI was also found to negatively influence the risk of developing fibrosis, as was also demonstrated by Donovan et al. [31].
3.2. DCIS
EORTC Trial 10853 contributed to the knowledge about the value of WBI after lumpectomy for DCIS [32]. The EBCTCG analysis, including this trial, demonstrated that after lumpectomy and RT the number of recurrences are about halved, for as well in situ as for invasive recurrences [33]. The number of patients needed to treat to avoid 1 recurrence within 10 years from treatment is 7. Notwithstanding this, the annual recurrence rate in these trials, which were mostly conducted in the 80's and early 90's, still amounted to an annual rate of 1.3%, of which half are invasive. Nowadays, results are demonstrated to be better.
A special case is Paget disease of the nipple, for which little evidence exist about the optimal treatment approach. The prospective phase 2 registration trial EORTC 10873 did not succeed to collect enough patients for bringing a high level of evidence for a conservative treatment composed of a complete excision of the nipple–areolar complex including possible underlying disease followed by WBI [34]. Thanks to this work, this treatment can be considered as a valuable alternative to mastectomy, leaving mastectomy for patients with more extensive disease or recurrence after RT.
3.3. Quality assurance
Quality assurance (QA) in radiation oncology has focussed greatly on trials in breast cancer. While the EORTC trial 10801 demonstrated equivalent overall survival rates for up to more than 20 years after treatment, a significant difference in local control was seen between the participating centers [35]. This has lead to an extensive QA program for the subsequent EORTC trial 22881/10882 [36]. Probably as a consequence of this, the variance in outcome for the participating patients did not vary from one center to another [37]. Since then, a QA program that is adapted to the design and the technical complexity became a standard procedure for all EORTC trial which have RT as a component of the treatment [38,39].
3.4. Challenges and failures
The outcome of breast cancer improved a lot thanks to ever-continuing progress in diagnosis and in locoregional and systemic treatment approaches. With the decrease in “events”, it become progressively more time consuming to accrue and follow enough patients to demonstrate a clinically relevant benefit. Moreover, when finally presented and published, part of the treatment given to the participating patients might be considered as outdated. This can complicate the acceptance of the results of the trials by part of the multidisciplinary team involved in breast cancer management.
Unfortunately, EORTC did not manage to bring the LAMANOMA trial (10974/22002) to a good end due to poor accrual of patients [40]. However, the main question of the trial, whether breast conserving treatment with RT with or without surgery following primary systemic treatment for locally advanced breast cancer can be considered as a valuable option still remains of interest for patient with non-inflammatory breast cancer after a good clinical response to systemic treatment. Due to a lack of interest and/of funding, the EORTC did also not manage to set up or contribute to a trial investigating the place of accelerated partial breast irradiation in low risk patients and to a trial further elaborating on the boost no boost trial but then focussing on young patients. Luckily enough, both efforts turned out to be successful in another setting and with a major contribution of RT departments that are dedicated members of the EORTC. The results obtained in the Young Boost trial, not yet split up per randomization group, clearly demonstrate to what extent local control in early stage breast cancer after breast conserving therapy has improved over the years (Fig. 3 [41]). After the very successful.
Fig. 3.

Local breast recurrence rate in three consecutive trials on breast conserving therapy from 1980 until 2012.
Reproduced with permission from Bartelink H, Bourgier C, Elkhuizen P. Has partial breast irradiation by IORT or brachytherapy been prematurely introduced into the clinic? Radiother Oncol 2012; 104(2): 139–142.
AMAROS trial [42] (Adjuvant Management of the Axilla, Radiotherapy of Surgery), EORTC did not succeed in setting up a successive trial, due to a number of reasons including the presentation of the results of other trials, ever again challenging the proposed trial designs.
3.5. Other trials
After the presentation and publication of new data on the selection of target volumes to be treated, we are now eagerly waiting for the results of the large prospective EORTC 22922/10925 trial that investigated to value of elective irradiation of the internal mammary and supraclavicular lymph node regions for stage 1–3 breast cancer patients after lumpectomy and axillary lymph node dissection or after modified radical mastectomy. An early analysis did not show an increased level of toxicity [43]. In Table 1, a division in three risk categories for locoregional relapse after mastectomy and axillary clearance is shown. Based on this, Table 2 is a proposed summary of the indications for radiotherapy for the different target volumes [44].
Table 1.
Risk categories for locoregional relapses after mastectomy and axillary clearance. Ax LN + = involved axillary lymph nodes.
| Risk category | Low | Intermediate | High |
|---|---|---|---|
| Tumor stage | T1-2 | T1-2 | T3-4 |
| Number of Ax LN+ | 0 | 1–3 | >3 |
| Grade | 1–2 | 3 | |
| Vascular invasion | – | + | |
| Histology | Ductal | Lobular | |
| Risk | <10% | 10–20% | >20% |
Reproduced with permission from Poortmans P. Educational review. Evidence based radiation oncology: breast cancer. Radiother Oncol 2007; 84: 84–101.
Table 2.
Indication for irradiation of the different target volumes after mastectomy and axillary clearance as well as for regional RT in the framework of BCT. Yes = evidence and generally accepted; Yes? = evidence but not generally accepted; No? = limited evidence, however advocated by some.
| Risk category | Low | Intermediate | High |
|---|---|---|---|
| Thoracic wall | No? | Yes? | Yes |
| Supraclavicular | No? | Yes? | Yes |
| Internal mammary | No | Yes? | Yes? |
| Axilla | No | No | No |
Reproduced with permission from Poortmans P. Educational review. Evidence based radiation oncology: breast cancer. Radiother Oncol 2007; 84: 84–101.
A prospective randomized EORTC 10981-22023 trial, AMAROS [42] was conducted to compare the treatment approaches for patients with involved sentinel lymph nodes. The results of this trial will be presented very soon. Together with the presentation and publication of the results of other studies, we can expect that the management of the axilla will continue to change markedly in the near future.
3.6. Current studies
Currently, EORTC participates to the intergroup trial led by the Australian Trans-Tasman Radiation Oncology Group (TROG) primarily investigating the value of a boost to the primary tumor bed in the framework of breast conserving treatment for patients with DCIS. In this trial, an optional randomization between the traditional and a hypofractionated radiation schedule is included as well. Accrual is going very well. Another intergroup trial, led by the Medical Research Council, SUPREMO (Selective Use of Postoperative Radiotherapy after Mastectomy) randomizes patients with 1–3 involved lymph nodes, and pT2pN0 tumors with grade 3 tumors and/or lymphovascular invasion between chest wall irradiation and follow-up [45]. Accrual will be completed this year. The trial also includes cardiac, quality of life, health economic and biological substudies.
3.7. Possible future trials
Currently, we are discussing the integration of partial breast irradiation into primary systemic treatment for patients with locally or loco-regionally advanced breast cancer that are possibly candidates for breast conserving treatment after tumor volume reduction. This fits into the principle of moving partial breast irradiation to the preoperative stage to decrease the amount of nontarget breast volume included, improve target volume definition. It also obviates the new challenges for target volume definition after oncoplastic surgery.
Conflict of interest statement
The authors of this manuscript have no actual or potential conflicts of interest to disclose.
Financial disclosure statement
None.
Acknowledgements
I would like to thank all patients and investigators including data managers, statisticians, medical advisors and others who have contributed to the conduct of the EORTC trials in breast cancer. A special word of thanks goes to Harry Bartelink, Walter van den Bogaert, Henk Struikmans, Alain Fourquet, Jean Claude Horiot, Helen Westenberg, Laurence Collette, Geertjan van Tienhoven, Marica Valli, and many others.
References
- 1.Lopez Guerra J.L., Isa N., Kim M.M., Bourgier C., Marsiglia H. New perspectives in radiation oncology: young radiation oncologist point of view and challenges. Rep Pract Oncol Radiother. 2012;17:251–254. doi: 10.1016/j.rpor.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kacprowska A., Jassem J. Partial breast irradiation techniques in early breast cancer. Rep Pract Oncol Radiother. 2011;16(6):213–220. doi: 10.1016/j.rpor.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Livi L., Buonamici F.B., Simontacchi G. Accelerated partial breast irradiation with IMRT: new technical approach and interim analysis of acute toxicity in a phase III randomized clinical trial. Int J Radiat Oncol Biol Phys. 2010;77:509–515. doi: 10.1016/j.ijrobp.2009.04.070. [DOI] [PubMed] [Google Scholar]
- 4.Belkacemi Y., Bourgier C., Kramar A. SHARE: a french multicenter phase III trial comparing accelerated partial irradiation versus standard or hypofractionated whole breast irradiation in breast cancer patients at low risk of local recurrence. Clin Adv Hematol Oncol. 2013;11:76–83. [PubMed] [Google Scholar]
- 5.Lopez Guerra J.L., Isa N., Matute Hypofractionated helical tomotherapy using 2.5–2.6 Gy daily fractions for localized prostate cancer. Clin Transl Oncol. 2013;15:271–277. doi: 10.1007/s12094-012-0907-y. [DOI] [PubMed] [Google Scholar]
- 6.Lopez Guerra J.L., Marrone I., Jaen J. Outcome and toxicity using helical tomotherapy for craniospinal irradiation in pediatric medulloblastoma. Clin Transl Oncol. 2013 doi: 10.1007/s12094-013-1048-7. [in press] [DOI] [PubMed] [Google Scholar]
- 7.Cendales R., Schiappacasse L., Schnitman F., García G., Marsiglia H. Helical tomotherapy in patients with breast cancer and complex treatment volumes. Clin Transl Oncol. 2011;13:268–274. doi: 10.1007/s12094-011-0652-7. [DOI] [PubMed] [Google Scholar]
- 8.Versmessen H., Vinh-Hung V., Van Parijs H. Health-related quality of life in survivors of stage I–II breast cancer: randomized trial of post-operative conventional radiotherapy and hypofractionated tomotherapy. BMC Cancer. 2012;12:495. doi: 10.1186/1471-2407-12-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ayata H.B., Güden M., Ceylan C. Comparison of dose distributions and organs at risk (OAR) doses in conventional tangential technique (CTT) and IMRT plans with different numbers of beam in left-sided breast cancer. Rep Pract Oncol Radiother. 2011;16(3):95–102. doi: 10.1016/j.rpor.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jin G.H., Chen L.X., Deng X.W., Liu X.W., Huang Y., Huang X.B. A comparative dosimetric study for treating left-sided breast cancer for small breast size using five different radiotherapy techniques: conventional tangential field, field-in-field, Tangential-IMRT, Multi-beam IMRT and VMAT. Radiat Oncol. 2013;8:89. doi: 10.1186/1748-717X-8-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nguyen S.K., Cao F., Ramaseshan R. Template based breast IMRT planning for increased workload efficiency. Radiat Oncol. 2013;8:67. doi: 10.1186/1748-717X-8-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chand M.E., Rivera S., Hennequin C., Hannoun-Lévi J.M., Quero L. Brachytherapy of breast cancer. Cancer Radiother. 2013 doi: 10.1016/j.canrad.2013.01.003. pii: S1278-3218(13)00014-0. [DOI] [PubMed] [Google Scholar]
- 13.Yao N., Mackley H.B., Anderson R.T., Recht A. Survival after partial breast brachytherapy in elderly patients with nonmetastasic breast cancer. Brachytherapy. 2013 doi: 10.1016/j.brachy.2013.01.168. pii: S1538-4721(13)00205-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hannoun-Levi J.M., Gourgou-Bourgade S., Belkacemi Y. GERICO-03 phase II trial of accelerated and partial breast irradiation in elderly women: feasibility, reproducibility, and impact on functional status. Brachytherapy. 2013 doi: 10.1016/j.brachy.2012.06.004. pii: S1538-4721(13)00007-X. [DOI] [PubMed] [Google Scholar]
- 15.Wareńczak-Florczak Z., Roszak A., Bratos K., Milecki P., Karczewska-Dzionk A., Włodarczyk H. Intraoperative radiation therapy as part of breast conserving therapy of early breast cancer. Results of one-year follow-up. Rep Pract Oncol Radiother. 2013;18(2):107–111. doi: 10.1016/j.rpor.2012.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ivaldi G.B., Leonardi M.C., Orecchia Preliminary results of electron intraoperative therapy boost and hypofractionated external beam radiotherapy after breast-conserving surgery in premenopausal women. Int J Radiat Oncol Biol Phys. 2008;72(2):485–493. doi: 10.1016/j.ijrobp.2007.12.038. [DOI] [PubMed] [Google Scholar]
- 17.Hershko D., Abdah-Bortnyak R., Nevelsky A., Gez E., Fried G., Kuten A. Breast-conserving surgery and intraoperative electron radiotherapy in early breast cancer: experience at the Rambam Health Care Campus. Isr Med Assoc J. 2012;14:550–554. [PubMed] [Google Scholar]
- 18.Vanderwalde N.A., Jones E.L., Kimple R.J. Phase 2 study of pre-excision single-dose intraoperative radiation therapy for early-stage breast cancers: six-year update with application of the ASTRO accelerated partial breast irradiation consensus statement criteria. Cancer. 2013 doi: 10.1002/cncr.27915. [in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Algara M., Arenas M., De las Peñas D. Radiation techniques used in patients with breast cancer: results of a survey in Spain. Rep Pract Oncol Radiother. 2012;17:122–128. doi: 10.1016/j.rpor.2012.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Litière S., Werutsky G., Fentiman I.S. Breast conserving therapy versus mastectomy for stage I–II breast cancer: 20 year follow-up of the EORTC 10801 phase 3 randomised trial. Lancet Oncol. 2012;13(4):412–419. doi: 10.1016/S1470-2045(12)70042-6. [DOI] [PubMed] [Google Scholar]
- 21.(EBCTCG) Early Breast Cancer Trialists’ Collaborative Group Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;366:2087–2106. doi: 10.1016/S0140-6736(05)67887-7. [DOI] [PubMed] [Google Scholar]
- 22.Darby S., McGale P., Correa C. Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011;378(9804):1707–1716. doi: 10.1016/S0140-6736(11)61629-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bartelink H., Horiot J.C., Poortmans P. Recurrence rates after treatment of breast cancer with standard radiotherapy with or without additional radiation. N Engl J Med. 2001;345:1378–1387. doi: 10.1056/NEJMoa010874. [DOI] [PubMed] [Google Scholar]
- 24.Bartelink H., Horiot J.C., Poortmans P.M. Impact of a higher radiation dose on local control and survival in breast-conserving therapy of early breast cancer: 10-year results of the randomized boost versus no boost eortc 22881-10882 trial. J Clin Oncol. 2007;25(22):3259–3265. doi: 10.1200/JCO.2007.11.4991. [DOI] [PubMed] [Google Scholar]
- 25.Jones H.A., Antonini N., Hart A.A. Impact of pathological characteristics on local relapse after breast-conserving therapy: a subgroup analysis of the EORTC boost versus no boost trial. J Clin Oncol. 2009;27:4939–4947. doi: 10.1200/JCO.2008.21.5764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Werkhoven E., Hart G., Tinteren H. Nomogram to predict ipsilateral breast relapse based on pathology review from the EORTC 22881-10882 boost versus no boost trial. Radiother Oncol. 2011;100:101–107. doi: 10.1016/j.radonc.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 27.Poortmans P.M., Collette L., Horiot J.C. Impact of the boost dose of 10 Gy versus 26 Gy in patients with early stage breast cancer after a microscopically incomplete lumpectomy: 10-year results of the randomised EORTC boost trial. Radiother Oncol. 2009;90:80–85. doi: 10.1016/j.radonc.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 28.Collette S., Collette L., Budiharto T. Predictors of the risk of fibrosis at 10 years after breast conserving therapy for early breast cancer: a study based on the EORTC trial 22881-10882 “boost versus no boost”. Eur J Cancer. 2008;44:2587–2599. doi: 10.1016/j.ejca.2008.07.032. [DOI] [PubMed] [Google Scholar]
- 29.Vrieling C., Collette L., Fourquet F. On behalf of the EORTC Radiotherapy and Breast Cancer Cooperative Groups, The influence of the boost in breast-conserving therapy on cosmetic outcome in the EORTC “boost versus no boost” trial. Int J Radiat Oncol Biol Phys. 1999;45:677–685. doi: 10.1016/s0360-3016(99)00211-4. [DOI] [PubMed] [Google Scholar]
- 30.Vrieling C., Collette L., Fourquet F. On behalf of the EORTC radiotherapy and breast cancer cooperative groups: the influence of patient, tumor and treatment factors on the cosmetic results after breast-concerving therapy in the EORTC “boost vs. no boost” trial. Radiother Oncol. 2000;55:219–232. doi: 10.1016/s0167-8140(00)00210-3. [DOI] [PubMed] [Google Scholar]
- 31.Donovan E.M., Bleackley N.J., Evans P.M. Dose-position and dose–volume histogram analysis of standard wedged and intensity modulated treatments in breast radiotherapy. Br J Radiol. 2002;75:967–973. doi: 10.1259/bjr.75.900.750967. [DOI] [PubMed] [Google Scholar]
- 32.Bijker N., Meijnen P., Peterse J.L. Breast conserving treatment with or without radiotherapy in ductal carcinoma-in-situ: ten-year results of European Organisation for Research and Treatment of Cancer randomized phase III trial 10853 – a study by the EORTC Breast Cancer Cooperative Group and EORTC Radiotherapy Group. J Clin Oncol. 2006;24:3381–3387. doi: 10.1200/JCO.2006.06.1366. [DOI] [PubMed] [Google Scholar]
- 33.Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) Effect of radiotherapy on local recurrence and survival in ductal carcinoma in situ of the breast (DCIS): an overview of the randomised trials. J Natl Cancer Inst Monogr. 2010;41:162–177. doi: 10.1093/jncimonographs/lgq039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bijker N., Rutgers E.J., Duchateau L., Peterse J.L., Julien J.P., Cataliotti L. EORTC breast cancer cooperative group, breast-conserving therapy for paget disease of the nipple: a prospective European organization for research and treatment of cancer study of 61 patients. Cancer. 2001;91(3):472–477. doi: 10.1002/1097-0142(20010201)91:3<472::aid-cncr1024>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 35.Bartelink H., Garavaglia G., Johansson K.A. Quality assurance in conservative treatment of early breast cancer, Report on a consensus meeting of the EORTC radiotherapy and breast cancer cooperative groups and the EUSOMA (European Society of Mastology) Radiother Oncol. 1991;22(4):323–326. doi: 10.1016/0167-8140(91)90172-d. [DOI] [PubMed] [Google Scholar]
- 36.van Tienhoven G., Mijnheer B.J., Bartelink H., González D.G. Quality assurance of the EORTC trial 22881/10882: boost versus no boost in breast conserving therapy. An overview. Strahlenther Onkol. 1997;173(4):201–207. doi: 10.1007/BF03039289. [DOI] [PubMed] [Google Scholar]
- 37.Poortmans P.M., Ataman F., Davis J.B. Quality assurance in the EORTC phase III randomised ‘boost vs. no boost’ trial for breast conserving therapy: comparison of the results of two individual case reviews performed early and late during the accrual period. Radiother Oncol. 2005;76(3):278–284. doi: 10.1016/j.radonc.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 38.Poortmans P., Kouloulias V., van Tienhoven G. EORTC Radiation Oncology and Breast Cancer Groups, Quality assurance in the EORTC randomized trial 22922/10925 investigating the role of irradiation of the internal mammary and medial supraclavicular lymph node chain works. Strahlenther Onkol. 2006;182(10):576–582. doi: 10.1007/s00066-006-1629-2. [DOI] [PubMed] [Google Scholar]
- 39.Fairchild A., Collette L., Hurkmans C.W. Do results of the EORTC dummy run predict quality of radiotherapy delivered within multicentre clinical trials? Eur J Cancer. 2012;48(17):3232–3239. doi: 10.1016/j.ejca.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 40.Sinacki M., Jassem J., van Tienhoven G. Conservative local treatment versus mastectomy after induction chemotherapy in locally advanced breast cancer: a randomised phase III study (EORTC 10974/22002, LAMANOMA) – why did this study fail? Eur J Cancer. 2005;41(18):2787–2788. doi: 10.1016/j.ejca.2005.06.027. [DOI] [PubMed] [Google Scholar]
- 41.Bartelink H., Bourgier C., Elkhuizen P. Has partial breast irradiation by IORT or brachytherapy been prematurely introduced into the clinic? Radiother Oncol. 2012;104(2):139–142. doi: 10.1016/j.radonc.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 42.Straver M.E., Meijnen P., van Tienhoven G. Sentinel node identification rate and nodal involvement in the EORTC 10981-22023 AMAROS trial. Ann Surg Oncol. 2010;17(7):1854–1861. doi: 10.1245/s10434-010-0945-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Matzinger O., Heimsoth I., Poortmans P. Toxicity at three years with and without irradiation of the internal mammary and medial supraclavicular lymph node chain in stage I to III breast cancer (EORTC trial 22922/10925) Acta Oncol. 2010;49(1):24–34. doi: 10.3109/02841860903352959. [DOI] [PubMed] [Google Scholar]
- 44.Poortmans P. Educational F review. Evidence based radiation oncology: breast cancer. Radiother Oncol. 2007;84:84–101. doi: 10.1016/j.radonc.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 45.Kunkler I.H., Canney P., van Tienhoven G., Russell N.S. MRC/EORTC (BIG 2-04) SUPREMO Trial Management Group, Elucidating the role of chest wall irradiation in ‘intermediate-risk’ breast cancer: the MRC/EORTC SUPREMO trial. Clin Oncol (R Coll Radiol) 2008;20(1):31–34. doi: 10.1016/j.clon.2007.10.004. [DOI] [PubMed] [Google Scholar]


