Abstract
Background
In radiation therapy with orthovoltage units, the tube design has a crucial effect on its dosimetric features.
Aim
In this study, the effect of anode angle on photon beam spectra, depth dose and photon fluence per initial electron was studied for a commercial orthovoltage unit of X-RAD320 biological irradiator.
Materials and methods
The MCNPX MC code was used for modeling in the current study. We used the Monte Carlo method to model the X-RAD320 X-ray unit based on the manufacturer provided information. The MC model was validated by comparing the MC calculated photon beam spectra with the results of SpekCalc software. The photon beam spectra were calculated for anode angles from 15 to 35 degrees. We also calculated the percentage depth doses for some angles to verify the impact of anode angle on depth dose. Additionally, the heel effect and its relation with anode angle were studied for X-RAD320 irradiator.
Results
Our results showed that the photon beam spectra and their mean energy are changed significantly with anode angle and the optimum anode angle of 30 degrees was selected based on less heel effect and appropriate depth dose and photon fluence per initial electron.
Conclusion
It can be concluded that the anode angle of 30 degrees for X-RAD320 unit used by manufacturer has been selected properly considering the heel effect and dosimetric properties.
Keywords: Monte Carlo modeling, X-RAD320 irradiator, Anode angle effect, Radiation therapy
1. Background
In spite of a considerable reduction in the application of orthovoltage X-ray units following the advent of electron linear accelerators in radiation therapy, they have found several applications in recent radiation therapy as well as radiobiological experiments.2,4–6,9
The anode type and angle as well as filters play an influential role in photon beam spectra and, consequently, depth dose characteristics for orthovoltage radiotherapy units. The X-ray tube manufacturers design and optimize the tube structural plan based on multiple mechanical and radiation considerations. The anode angle has a determinant effect on photon beam intensity characteristics across the X-ray beam which is known as heel effect in X-ray tubes. On the other hand, changing the anode angle alters the X-ray absorption inside the tungsten target and photon beam spectra received by therapeutic beam are changed accordingly. Monte Carlo (MC) modeling of X-ray units including kilovoltage and orthovoltage units has been done in several comprehensive studies.1,2,5–7,9–11 The rationale behind the need for MC modeling of these units has remained untouched yet. For instance, precise information regarding the absorbed dose distributions in water has a critical impact on the accuracy of results provided by means of dosimetry protocols. However, some MC studies have been performed to give rise to more detailed information about the effect of tube components on dosimetric characteristics including depth dose and photon beam spectra for a better and more efficient tube designation. In an MC study by Verhaegen et al. realistic models were built for two complete X-ray units using EGS4/BEAM code.11 They studied the electron contamination and photon dose build-up at water surface for two kilovoltage radiotherapy units. Recent interest in radiation therapy with orthovoltage beams for animal studies, as well as the application of high atomic number contrast media, such as iodine in radiation therapy have been new motivations for MC modeling of these units.2–5
2. Aim
In the current study, an MC model of X-RAD320 biological irradiator, which is being used currently for animal and cell culture irradiation, was built based on the manufacturer provided data. The effect of anode angle on dosimetric properties of this unit was studied and the optimum anode angle was selected for the unit. The purpose was to verify the appropriateness of anode angle for X-RAD320 biological irradiator by the MC method. Additionally, the validated MC model can be used either for further studies on its dosimetry or for the application of this unit for animal radiation therapy.
3. Materials and methods
3.1. Monte Carlo modeling
An MC model was made for X-RAD320 biological irradiator (Precision X-Ray Inc., USA) using MCNPX code. This unit generates orthovoltage X-ray beams and routinely is used for irradiation of small animals and cell cultures in radiobiological studies. The MC model consisted of a ceramic envelope, tungsten anode embedded in a copper part, a 3 mm beryllium intrinsic filter, 2 mm aluminum filter and beam defining collimators (Fig. 1). The lead shielding of the tube was not simulated and the X-ray leakage effect was not considered in our simulations. A monoenergetic electron source at the distance of 10 cm from the anode surface was considered. The electron beam diameter was 2.44 mm striking on the actual focal spot with area of 8 mm2. An anode angle of 30 was considered according to manufacturer's drawings. This setup remained constant in all simulations and in other simulations for an optimum anode angle determination; the only changing parameter was the anode angle.
Fig. 1.
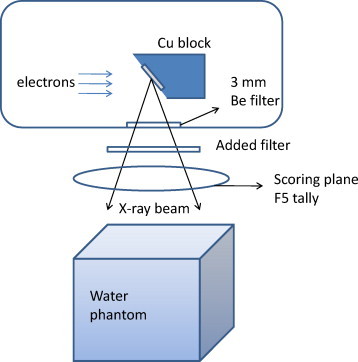
The schematic geometry of simulated tube and water phantom used for X-RAD320 biological irradiator.
A f5 tally (which scores fluence in terms of number per cm2), with a ring detector with a radius of 5 cm was defined under beam defining collimators at the distance of 20 cm from the focal spot. The detector covered a field size of 10 cm × 10 cm from the cathode side to the anode side of the exiting photon beam. The field size at the distance of 50 cm was 20 cm × 20 cm. Moreover, using the F5 tally, photon fluence in terms of photon per cm2 per initial electron was scored by running the input file for 2000 min in a personal computer 2.4 GHz. The statistical uncertainty of results was less than 1.5% for all tallies calculated in the current study. The depth doses with a 2 mm step were scored using a F6 tally inside a water phantom with dimensions of 20 cm × 20 cm × 20 cm at the source to surface distance of 50 cm. The F6 tally scores the absorbed dose in terms of MeV per gram of tallying cells. Absorbed dose inside the water phantom was scored for different anode angles. The statistical uncertainty for absorbed dose calculations was less than 1% in all depths. Because of modeling of low energy electrons and photons transport in this study, so as to avoid any bias in our results, no electron and photon energy cutoffs were used.
SpekCalc software (version 1.1) was used for validation of our MCNPX model. This software has been developed using the results of comprehensive MC modeling of orthovoltage X-ray tubes used for radiation therapy. It is free and can be obtained by sending request to its producers. The interested reader can find more detailed information about this software in the article of Poludniowski et al.8 It is capable to calculate X-ray spectra for X-ray tubes for different anode angles and filters. It can incorporate different types of filters and anode angles from 5 to 30 degrees in its calculations.8 Additionally, it should be noted that the calculations of this software were benchmarked against measurements and its calculations’ accuracy were validated by measured results.
4. Results and discussion
We calculated photon beam spectra in three tube voltages including 100, 200 and 300 kVp by the MC method and compared them with the results of SpekCalc software. The results for all tube voltages showed very a similar pattern between MC and SpekCalc calculations, so to summarize the results, only the 300 kVp spectra were shown (Fig. 2). Fig. 2 shows the photon beam spectra calculated by MCNPX and SpekCalc for 300 kVp + 2 mm Al and the anode angle of 30 degrees. In SepkCalc calculations due to its limitation, the lower photon energy cut-off was 30 keV, but in MCNPX calculations the photon spectra were calculated from zero energy to the maximum photon energy. There was a close agreement between the results of both methods for the whole energy spectra. However, the small differences can be attributed to the different algorithms and cross-section files used for MCNPX code and SpekCalc software. The results confirmed that our model is accurate and can be used for other MC applications, such as MC dose distribution calculations in water phantom.
Fig. 2.
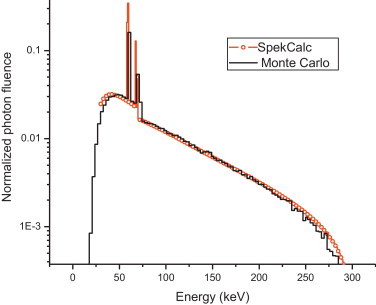
The comparison of MCNPX calculated spectrum with results of SpekCalc software for 300 kVp photon beam and 2 mm Al filter of XRAD320 X-ray irradiator with anode angle of 30 degrees.
In Fig. 3, the photon fluence per initial electron was calculated by MCNPX code for different anode angles from 15 to 35 degrees. The objective was to determine the anode angle with the highest photon fluence per initial electron striking on the target for the studied X-ray tube. It can be seen that photon fluence is raised with anode angle from 15 to 32 degrees. But it begins to decline after 32 degree anode angle. The output variation from 28 to 32 degrees is very slight and the optimum anode angle based on output information lies between 28 and 32 degrees for this X-ray tube. However, other considerations, including heel effect and penumbra, should be taken into account for a better anode angle selection.
Fig. 3.
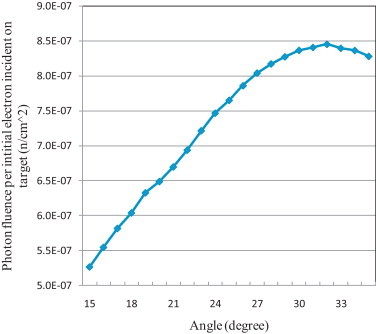
The photon fluence variation with anode angle for 300 kVp photon beam calculated by MCNPX.
It can be seen in Fig. 4 that the photon fluence and photon spectra are changed considerably with anode angle from 15 to 29 degrees. But it remains unchanged after 29 degrees. With increasing the anode angle, more photons can reach the useful beam because the self-absorption of the anode decreases with the anode angle being increased. However, it should be mentioned that there is a considerable trade-off between anode angle which determines the focal spot size and geometric penumbra and tube output in terms of cGy/min for radiation therapy applications.
Fig. 4.
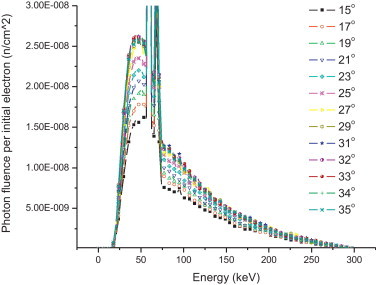
The photon beam spectra variation with anode angle for X-RAD320 unit at kVp of 300 + 2 mm Al.
To find an optimum anode angle using Fig. 5, the flatter beam profile can be selected. It can be seen that there are large differences between the anode and cathode ends of beam profile from 15 to about 28 degrees, while after 28 degrees, the beam flatness does not vary significantly with angles from 28 to 31 degrees. However, there is a drop-off in photon intensity at the cathode end of the profile for angles from 32 to 35 degrees. This decrease is pronounced for the 35 degree anode angle.
Fig. 5.
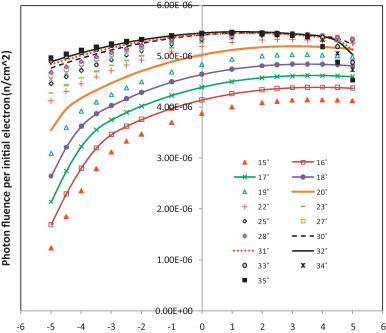
Photon fluence variation across the radiation field under collimator for field size of 10 cm × 10 cm at a distance of 20 cm from focal spot.
As can be seen in Fig. 6, there was very small difference among three depth doses calculated for 15, 25 and 30 degree anode angles. Nonetheless, evaluation of the data showed that surface dose increases with angle and its maximum increase was about 1% between 15 and 30 degrees. However, the difference between depth doses increased with depth and it reached up to 3% at the depth of 8 cm between 15 and 30 degree anode angles. The depth dose for 30 degrees is less than for 15 degrees because of photon spectra smoothing in large angles and more low energy photons are found in larger anode angles.
Fig. 6.
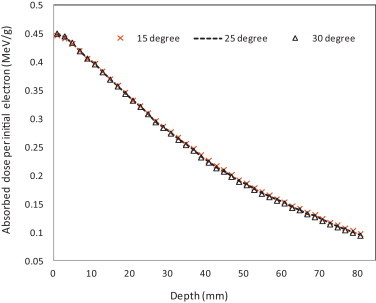
The MCNPX calculated depth dose for different anode angles for field size of 5 cm × 5 cm at source to surface distance of 50 cm.
5. Conclusions
The purpose of the current study was to evaluate the effect of anode angle on photon beam spectra and other dosimetric features of a kilovoltage radiation therapy unit. Our results showed that the anode angle has an influencing effect on heel effect and beam intensity across the therapeutic beam. But it did not show considerable effect on depth dose curves. The results confirmed that the anode angle of 30 degrees used in X-RAD320 irradiator is the optimum angle for beam uniformity and radiation output of the irradiator.
Conflict of interest
None declared.
Financial disclosure
None declared.
Acknowledgments
The authors would like to thank X-RAD 320 manufacturer for providing required information for Monte Carlo modeling. Also, we would like to thank Dr. James Hainfeld for his motivation and help in this project.
References
- 1.Bontempi M., Andreani L., Rossi P.L., Visani A. Monte Carlo simulator of realistic X-ray beam for diagnostic applications. Med Phys. 2010;37:4201–4209. doi: 10.1118/1.3453578. [DOI] [PubMed] [Google Scholar]
- 2.Currie B.E. Determining superficial dosimetry for the internal canthus from the Monte Carlo simulation of kV photon and MeV electron beams. Australas Phys Eng Sci Med. 2009;32:68–80. doi: 10.1007/BF03178631. [DOI] [PubMed] [Google Scholar]
- 3.Gao W., Raeside D.E. Orthovoltage radiation therapy treatment planning using Monte Carlo simulation: treatment of neuroendocrine carcinoma of the maxillary sinus. Phys Med Biol. 1997;42:2421–2433. doi: 10.1088/0031-9155/42/12/009. [DOI] [PubMed] [Google Scholar]
- 4.Garnica-Garza H.M. A Monte Carlo comparison of three different media for contrast enhanced radiotherapy of the prostate. Technol Cancer Res Treat. 2010;9:271–278. doi: 10.1177/153303461000900306. [DOI] [PubMed] [Google Scholar]
- 5.Kawase T., Kunieda E., Deloar H.M. Converging stereotactic radiotherapy using kilovoltage X-rays: experimental irradiation of normal rabbit lung and dose-volume analysis with Monte Carlo simulation. Int J Radiat Oncol Biol Phys. 2009;75:468–474. doi: 10.1016/j.ijrobp.2009.01.085. [DOI] [PubMed] [Google Scholar]
- 6.Kim J., Hill R., Claridge M.E., Kuncic Z. An investigation of backscatter factors for kilovoltage X-rays: a comparison between Monte Carlo simulations and Gafchromic EBT film measurements. Phys Med Biol. 2010;55:783–797. doi: 10.1088/0031-9155/55/3/016. [DOI] [PubMed] [Google Scholar]
- 7.Nunn A.A., Davis S.D., Micka J.A., DeWerd L.A. LiF: Mg, Ti TLD response as a function of photon energy for moderately filtered X-ray spectra in the range of 20–250 kVp relative to 60Co. Med Phys. 2008;35:1859–1869. doi: 10.1118/1.2898137. [DOI] [PubMed] [Google Scholar]
- 8.Poludniowski G., Landry G., DeBlois F., Evans P.M., Verhaegen F SpekCalc: a program to calculate photon spectra from tungsten anode X-ray tubes. Phys Med Biol. 2009;54:N433–N438. doi: 10.1088/0031-9155/54/19/N01. [DOI] [PubMed] [Google Scholar]
- 9.Schell M.C., Rosenzweig D.P., Weaver K.A., Fenton B.M., Rubin P. Characterization of the dose perturbation by stents as a function of X-ray beam energy. Cardiovasc Radiat Med. 1999;1:154–159. doi: 10.1016/s1522-1865(99)00013-x. [DOI] [PubMed] [Google Scholar]
- 10.Verhaegen F., Granton P., Tryggestad E. Small animal radiotherapy research platforms. Phys Med Biol. 2011;56:R55–R83. doi: 10.1088/0031-9155/56/12/R01. [DOI] [PubMed] [Google Scholar]
- 11.Verhaegen F., Nahum A.E., Van de Putte S., Namito Y. Monte Carlo modelling of radiotherapy kV X-ray units. Phys Med Biol. 1999;44:1767–1789. doi: 10.1088/0031-9155/44/7/315. [DOI] [PubMed] [Google Scholar]


