Abstract
Background
Treatment of breast fibroadenoma remains a subject of clinical discussion. Recommended methods include clinical observation or surgical excision of the lesion. The procedure involves hospitalisation and anaesthesia, leaving a scar on the breast.
Aim
The aim of this study was to present the Centre's experience in removing lesions radiologically suspicious of fibroadenoma by means of an ultrasound-guided vacuum-assisted core-needle biopsy as an alternative to a classical surgery.
Materials and methods
Between March 2007 and April 2010, 196 ultrasound-guided vacuum-assisted biopsies were performed in the Mammotome Biopsy Laboratory of the 1st Surgical Oncology and General Surgery Department at the Greater Poland Cancer Centre in Poznań. The procedure was delivered to female patients aged 17–91 years (mean 40.8, median 39). Qualified for removal were ultrasound identified lesions described as fibroadenomas.
Results
The average size of excised lesions according to pre-biopsy ultrasound image was 13.53 ± 8.92 mm (median 11 mm, range 4–60 mm). In 184 cases (93.9%), benign lesions were found in the final histopathologic examination. Pre-cancer lesions were found in 10 cases, and invasive lesions in two cases. Overall, after follow-up ultrasound examination, four patients were qualified for subsequent surgical resection of lesions that had been left behind.
Conclusion
Vacuum core-needle biopsy is an effective tool enabling removal of breast fibroadenomas. It combines features of a lesion resection and histopathologic material collection providing an access with minimum invasiveness.
Keywords: Fibroadenoma, Breast biopsy, Cosmetic effect
1. Introduction
Fibroadenoma is a benign tumour, in most cases distinctly separated from the surrounding tissue, originating from the epithelium and stroma of the terminal ductolobular unit. It is most common in young women under 25 years of age. The lesion occurs rarely in the post-menopausal period; however, with hormone-replacement therapies widely used, the prevalence of fibroadenoma has increased in that age group, too.1 The most frequent clinical manifestation is a palpable tumour detected during self-examination of the breast or control medical examination. In most cases, tumours are found to be smooth-surfaced, painless, and mobile in relation to their surrounding tissue, sized 1–3 cm. Larger or multifocal fibroadenoma lesions occur in less than 20% of cases. According to Smalwood et al., 15% of lesions regress, while 19% grow in size.2 In most cases, having reached the size of 2–3 cm, they remain static for months or even years. Sometimes, fibroadenomas are found to co-exist with phyllodes tumours. These lesions may be difficult to distinguish in clinical and ultrasound examination. Large size, fast growth and ultrasound visible liquid-filled areas suggesting phyllodes tumour may prove to be useful differentiating characteristics. Transformation into a malignant neoplasm is extremely rare. As Ozello and Gump report, it applies to 0.3% of cases in women under 40 years of age.3 Lobular cancers are then observed more likely than ductal lesions.
A triple test comprising clinical examination, ultrasound and biopsy remains the basic method for diagnosing fibroadenomas. Fine-needle or core-needle biopsy may be proposed in order to collect material for histopathologic examination.
Treatment of breast fibroadenoma remains a subject of clinical discussion. For non-palpable lesions, clinical observation, including necessary ultrasound, and histopathologic diagnosis are recommended. For palpable lesions, some authors recommend surgical excision, given patients’ anxiety and their frequent reluctance to cooperate in the monitoring of such lesions. Others propose observation until the age of 35 and surgical procedure, should the lesion fail to regress. The surgery involves hospitalisation and anaesthesia, leaving a scar on the breast. In recent years, a new option has emerged for minimal invasive treatment of benign breast lesions – ultrasound-guided vacuum-assisted biopsy.
The aim of this study was to present the Centre's experience in removing lesions radiologically suspicious of fibroadenoma by means of an ultrasound guided vacuum core-needle biopsy.
2. Materials and methods
Between March 2007 and April 2010, 196 ultrasound-guided vacuum biopsies were performed in the Mammotome Laboratory of the 1st Oncologic and General Surgery Department at the Greater Poland Cancer Centre in Poznań. The procedure was delivered to female patients aged 17–91 years (mean 40.8, median 39). Qualified for removal were ultrasound demonstrable lesions described as consistent with fibroadenoma (Fig. 1). The biopsies were initially performed with Mammotom manufactured by Ethicon Endo-Surgery Inc., USA, then with the equipment of Encor Breast Biopsy System Sono RX Inc. USA, under the guidance Siemens Sonoline G20 ultrasound system, Siemens Medical Solutions Inc. USA. As a rule, procedures were performed in an outpatient setting, in 13 cases they were performed in patients hospitalised at the 1st Oncologic and General Surgery Department, preliminarily qualified for surgical excision of the lesion. The procedures, preceded by sterile draping of the operative field, were performed with single-use needles 8, 11 G (Mammotom) or 7, 10 G (EnCor). All patients were informed of the method to be used, the benefits and possible complications arising from it. They were also advised that a surgical resection of the lesion would be necessary if pre-cancer, pre-invasive or invasive lesions were to be found. Biopsy sites were locally anaesthetised using 1% solution of lignocaine and in the event of pain occurring during the procedure, additional anaesthetic was introduced through the chamber of the biopsy needle. After the procedure was completed, patients were asked to stay in the outpatient clinic or hospital department for a short observation, with the biopsy site compressed for 10–20 min with an ice pack. Their biopsy sites having been controlled, patients were sent home with an information sheet and further recommendations.
Fig. 1.
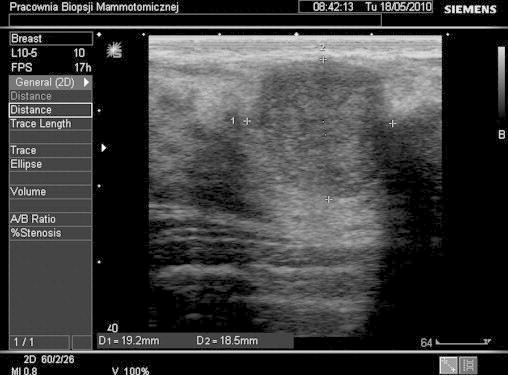
Ultrasound image of fibroadenoma sized 19.2 mm × 18.5 mm prior to vacuum-assisted biopsy.
3. Results
All patients were qualified for removal of one breast lesion at one procedure. The average procedure duration was 10–25 min. A procedure was terminated upon removal of the entire lesion, as visualised by the ultrasound image, or when bleeding occurred preventing it from being continued. The average size of excised lesions according to pre-biopsy ultrasound image was 13.53 ± 8.92 mm (median 11 mm, range 4–60 mm). 108 (55.1%) lesions were located in left breasts, 88 (44.9%) in right ones. Tumours were most often found in the outer upper quadrant – 107 cases (54.6%).
An average of 14.88 ± 9.03 (median 13, range 2–60) tissue casts were collected per biopsy. In 184 cases (93.9%) benign lesions were found in the final histopathologic examination. Of these, most commonly diagnosed was fibroadenoma (n = 157, 80.1% of all lesions subjected to biopsy). Other benign lesions identified included (in order of occurrence): adenosis (sclerosing, simple, blunt duct, apocrine, tubular, microglandular), UDH, microcalcifications, cystic mastopathy, steatosis, fibrosis, inflammations, glandular enlargement, papillomatosis, lobular hyperplasia, radial scar, fat necrosis. Pre-cancer lesions were found in 10 cases. Four patients were diagnosed with atypical ductal hyperplasia (ADH), other four with flat epithelial atypia (FEA), one was diagnosed with both ADH and FEA, and one with atypical lobular hyperplasia (ALH). Two post-biopsy patients were diagnosed with invasive cancer. All patients with diagnosed pre-cancer and cancer lesions were qualified for extended surgical excision in hospital setting.
Non-radical removal of lesions was reported for six cases at the time of biopsy. In two cases, vacuum-assisted core-needle biopsy was not successful as lesions qualified for treatment were too large (50 and 60 mm) and located deep down the cardiac muscle fascia. A similar parafascial location prevented biopsy in one patient with a tumour of 5 mm in diameter. In two other patients residual lesions were left unremoved due to heavy haemorrhage that disabled the procedure from being completed. In one case, haemorrhage was so massive that a surgical revision of the biopsy site was necessary. Overall, after follow-up ultrasound examinations performed in the surgery clinic, four patients were qualified for subsequent surgical resection of lesions that had been left behind.
Complications included pain, hematoma at the biopsy site, and skin ecchymosis. None of the patients has reported infection of the biopsy site. All complications subsided within two months following the procedure and had no serious clinical consequences. All patients were happy with the cosmetic effect of the procedure (Fig. 2).
Fig. 2.

Core-needle biopsy procedure.
4. Discussion
A tumour exhibiting clinical features of breast fibroadenoma is one of the most common causes of young women's visits to breast disease specialists. A palpable lesion in the breast arouses patients’ anxiety about its oncologic potential as well as cosmetic effect following removal of the lesion. Having recognised the nature of the tumour, that is after the triple confirmation of the diagnosis by clinical examination, radiology and biopsy, a method of treatment may be proposed to the patient. In the case of benign lesions, a choice arises between surgical removal or close observation. In most cases, singular lesions are removed surgically, mainly because young patients’ are concerned about having a tumour in their breast.4–8 Ultrasound-guided vacuum-assisted core-needle biopsy is a new method that provides the benefits of an operative procedure, while eliminating some of its drawbacks. For more than one decade, it has been recognised around the world as a low-invasive technique of diagnosing and treating benign breast lesions9. Importantly, this technique does not require general anaesthesia. Another advantage it offers is the size of a resulting scar. In the case of a surgery, it is usually around 3–4 cm, while in the case of biopsy it is in the region of 3–5 mm (Fig. 3). It seems particularly essential for patients concerned with their appearance.10,11 Reliable histopathologic material, collected to confirm a benign nature of the lesion and to exclude an invasive process, is an important prerequisite of a vacuum-assisted biopsy It should be mentioned that vacuum-assisted biopsies are reported to cause fewer complications than a classical surgery. Of importance is also the cost of the procedure, which in most countries is much lower than that of a surgery and related hospitalisation. In Poland, costs related to the work of an operating theatre are underestimated and regarded as lower than the costs of purchase of a biopsy needle.
Fig. 3.

Two neighbouring scars in a single patient: one following a classical surgical resection of fibroadenoma (left) and one following a vacuum-assisted biopsy (right, closer to the aureola).
The size of tumour is a limitation for an effective removal by biopsy. As stated by Sperber et al., all lesions less than or equal to 1.5 cm (mean volume 0.25 mL) were completely excised. Of the lesions measuring 1.5–2.0 cm, 11 (55%) were completely excised, while for diameters larger than 2 cm (mean volume 1 mL) tumours could not be removed completely.11 In Polish studies conducted by Stanek et al. on a group of 28 patients, a complete ultrasound-confirmed removals of lesions were achieved in 82% of cases. In all of them, histopathologic material was received.10 The study by Grady et al. states that the incidence of fibroadenoma reoccurrence following biopsy excision for lesions larger than 2 cm in diameter is 15% after 22 months and as much as 33% after 5 years of follow-up observation.11
75% of patients reported no pain, the remaining ones reported but moderate pain during the procedure.11 Thurley et al. note that 55% of patients report pain rated 3/10 within up to one week after the procedure.12 The post-biopsy scar was acceptable for all patients and after a year, hardly noticeable in 40% of them. Frequently observed subcutaneous extravasation was found in 25% of patients, but not leading to any further consequences.11 Other significant complications included livedo in 19% and infections in 6% of cases. 85% of patients assessed the cosmetic effect as good.
Vacuum-assisted core-needle biopsy is an effective tool enabling excision of breast fibroadenomas.13,14 It combines features of a lesion resection and histopathologic material collection providing an access with minimum invasiveness. It marks another major step on the way towards minimal invasive surgery, which may be comparable to open surgery versus laparoscopy in gallstone treatment.
References
- 1.Santen R., Mansel R. Benign breast disorders. N Eng J Med. 2005;353:275–285. doi: 10.1056/NEJMra035692. [DOI] [PubMed] [Google Scholar]
- 2.Smalwood J.A., Roberts A., Guyer D.P., Taylor I. The natural history of fibroadenoma. Br J Clin Pathol. 1991;95:614–622. [Google Scholar]
- 3.Ozello L., Gump F. The management of patients with carcinoma in fibroadenomatous tumors of the breast. Surg Gynecol Obstet. 1985;160:99–104. [PubMed] [Google Scholar]
- 4.Brenner R.J. Lesions entirely removed during stereotactic biopsy: preoperative localization on the basis of mammographic landmarks and feasibility of free-hand technique: initial experience. Radiology. 2000;214:585–590. doi: 10.1148/radiology.214.2.r00ja18585. [DOI] [PubMed] [Google Scholar]
- 5.Cant P.J., Madden M.V., Coleman M.G., Dent D.M. Non-operative management of breast masses diagnosed as fibroadenoma. Br J Surg. 1995;82:792–794. doi: 10.1002/bjs.1800820624. [DOI] [PubMed] [Google Scholar]
- 6.Cant P.J., Madden M.V., Close P.M., Learmonth G.M., Hacking E.A., Dent D.M. Case for conservative management of selected fibroadenomas of the breast. Br J Surg. 1987;74:857–859. doi: 10.1002/bjs.1800740936. [DOI] [PubMed] [Google Scholar]
- 7.Alle K.M., Moss J., Venegas R.J., Kalkhali I., Klein S.R. Conservative management of fibroadenoma of the breast. Br J Surg. 1996;83:992–993. doi: 10.1002/bjs.1800830735. [DOI] [PubMed] [Google Scholar]
- 8.Dixon J.M., Dobie V., Lamb J., Walsh J.S., Chetty U. Assessment of the acceptability of conservative management of fibroadenoma of the breast. Br J Surg. 1996;83:264–265. [PubMed] [Google Scholar]
- 9.Jayashinghe Y., Simmons P.S. Fibroadenomas in adolescence. Curr Opin Obstet Gynecol. 2009;21:402–406. doi: 10.1097/GCO.0b013e32832fa06b. [DOI] [PubMed] [Google Scholar]
- 10.Stanek J., Szpurek D., Moszyński R., Uchman P., Targowska-Ferenc A., Sajdak S. Ocena skuteczności leczenia operacyjnego gruczolakowłókniaków piersi mammotomem pod kontrolą mammosonografii. Przegląd Ginekologiczno-Położniczy. 2004;4(4):167–171. [Google Scholar]
- 11.Grady I., Gorsuch H., Wilburn-Bailey S. Long term outcome of benign fibroadenomas treated by ultrasound-guided percutaneous excision. Breast J. 2008;14:275–278. doi: 10.1111/j.1524-4741.2008.00574.x. [DOI] [PubMed] [Google Scholar]
- 12.Thurley P., Evans A., Hamilton L. Patient satisfaction and efficacy of vacuum-assisted excision biopsy of fibroadenomas. Clin Radiol. 2009;64:381–385. doi: 10.1016/j.crad.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 13.Sperber F., Blank A., Metser U., Flusser G., Klausner J.M., Lev-Chelouche D. Diagnosis and treatment of breast fibroadenomas by ultrasound-guided vacuum-assisted biopsy. Arch Surg. 2003;138:796–800. doi: 10.1001/archsurg.138.7.796. [DOI] [PubMed] [Google Scholar]
- 14.Wilkinson S., Forrest A.P. Fibroadenoma of the breast. Br J Surg. 1985;72:838–840. doi: 10.1002/bjs.1800721021. [DOI] [PubMed] [Google Scholar]


