Abstract
Aim
The place of adjuvant radiotherapy in the treatment of sinonasal melanoma.
Background
Sinonasal mucosal melanoma is a rare disease with poor prognosis and requires a complex treatment. Elective neck dissection in patients with N0 and adjuvant radiotherapy has been a source of controversy. High late regional recurrence rates rise questions about elective irradiation of the neck nodes in patients with N0 stage disease.
Methods
We present our two years’ follow up in a case of locally advanced sinonasal melanoma and literature review of the treatment options for mucosal melanoma.
Results
In locally advanced sinonasal melanoma treated with surgical resection, postoperative radiotherapy and chemotherapy we had local tumor control. Two years later, a regional contralateral recurrence without distant metastasis occurred.
Conclusions
Literature data for frequent neck lymph nodes recurrences justify elective neck dissection. Postoperative elective neck radiotherapy for patients with locally advanced sinonasal melanoma and clinically N0 appears to decrease the rate of late regional recurrences.
Keywords: Sinonasal melanoma, Complex treatment, Mucosal melanoma, Surgery, Radiotherapy
1. Introduction
Malignant melanoma affecting the nasal cavity and paranasal sinuses is a rare disease1–5 with a poor prognosis.3,12–16 Optimal complex treatment and the role of adjuvant radiotherapy for sinonasal melanoma remains an open issue.13
2. Case reports
A 65-years-old male with locally advanced paranasal malignant melanoma. According to Tanaka et al. the types of melanoma are histologically subdivided into nonpigmented mixed type.17,18 Immunohistochemistry – the tumor cells strongly expressed S-100 protein and HMB-45 monoclonal antibody microstaging as described by Prasad et al. Level III, deep invasion into surrounding tissue.2,3,9,10
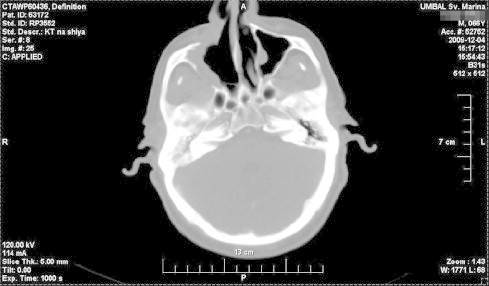
CT scan-head and neck – tumor, involving right nasal cavity, right paranasal sinuses-maxillary, ethmoidal, frontal and retrobulbar space. There is no evidence for positive cervical lymph nodes (Fig. 1). The stage was defined according to the Union International Contre le Cancer stage І (confined to the primary site without positive cervical lymph nodes).9
Fig. 1.
Preoperative CT scan – locally advanced sinonasal melanoma.
Surgery – a mediofascial resection with positive excision margins R2 was done. Postoperative CT scan demonstrates residual tumor in all paranasal sinuses (Fig. 2).
Fig. 2.
Postoperative CT scan – residual tumor.
CT scans of the brain, thorax and abdomen were negative. Bone scan showed no metastases. Postoperative external beam radiation therapy to total dose of 70 Gy was performed. Conventional radiotherapy was prescribed. CTV covered also the right eye and retrobulbar space, due to tumor infiltration. CT scan (one month after radiotherapy) – tumor reduction around 80%, tumor size – 15–20 mm, localized in the right frontal and ethmoidal sinuses (Fig. 3).
Fig. 3.
CT scan – one month after postoperative radiotherapy – residual tumor.
Five cycles of chemotherapy with Vinblastin – 1.2 mg/m for 1–4 days, Cisplatinum – 25–50 mg/m for 1–4 days, DTIC – 800 mg/m for 1 day were applied. MRI imaging after the fourth cycle showed poor response to systemic treatment (Fig. 4).
Fig. 4.
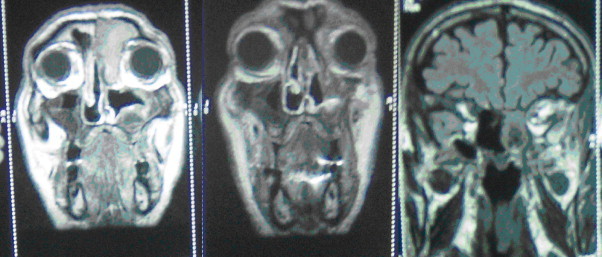
MRI imaging – residual tumor in the right frontal sinus and ethmoidal cells without right eye infiltration.
Second surgical excision was performed. Surgical margins were macroscopic and microscopic clear – R0. MRI imaging six months after the re-surgery showed no evidence of disease – local tumor control(Fig. 5).
Fig. 5.
MRI imaging – local tumor control – after surgical changes in maxillary and paranasal sinuses.
Two years after the treatment, PET/CT was performed. The results revealed metastatic contralateral neck lymph nodes (25–27 mm). Selective left neck dissection was done. Pathologic examination showed lymph nodes with metastases from malignant melanoma with pigment.
3. Discussion
Our observations rise a number of questions: (1) What is the optimal complex treatment according to local tumor control and disease free survival? (2) What is the benefit from adjuvant radiotherapy in locally advanced sinonasal melanoma? (3) What is the role of elective neck irradiation (in patients with N0 disease)?
At the time of diagnosis, sinonasal melanoma is often locally advanced5 with all paranasal sinuses affected, including retrobulbar infiltration (our case). Treatment of choice for mucosal melanoma is radical surgical excision with clear margins.1,14–16 This is possible for early stage melanomas, without infiltration in adjacent structures. The literature data for incidence of lymph node metastases is controversial – rare (below 6%)16 or frequent.8 Metastatic neck lymph nodes worsen the prognosis and require neck dissection.17,18 It is curative only for 30% of cases, because the others already have occult distant metastases.19
Despite high rates of local and regional recurrences in patients with N0, elective neck dissection is still controversial.5 It seems that the dissection is beneficial in selective group of patients – with deep infiltration and high risk of occult lymph node metastases.16,19 Elective neck dissection will probably improve the rates of local neck metastases and disease free survival.
In our case we have a contralateral late regional recurrence two years after treatment, without local relapse and distant metastases. According to McMasters et al., in the neck region, drainage patterns vary and tend to be a higher number of sentinel lymph nodes.21 Lymph drainage is unpredictable and it is mandatory to perform preoperative lymphoscintigraphy.5,22 If interval sentinel lymph nodes are negative, there is no place for lymphadenectomy. In stage 3 disease (without palpable neck nodes), we should suggest elective neck dissection.5
Postoperative radiotherapy in patients with R1–R2 resection is indicated, although melanoma has always been considered as a radioresistant tumor.14,23–25 Irradiation is more often used in the sinonasal melanoma because of the difficulty in obtaining satisfactory clear surgical margins in this region 8. We report 80% regression of the tumor after total dose of 70 Gy and after second operation we have local tumor control for two years. Many authors published data for improved loco-regional control after adjuvant radiotherapy, without survival benefit because of the high rate of distant metastases.8,13,26,27 Local control of three years was at 57% after surgery alone and 71% after surgery and adjuvant radiotherapy.28 Some authors reported improvement in loco-regional control with postoperative radiotherapy only for patients with early stage disease.27
Many investigators recommend postoperative radiotherapy for patients with advanced stage melanoma with positive surgical margins (R1–R2) and pN1 with extracapsular extension.13 Adjuvant radiotherapy resulted in a 10-year regional control rate of 94%. The authors recommend adjuvant irradiation for patients with extracapsular extension, lymph nodes measuring 3 cm in size or larger, the involvement of multiple lymph nodes, recurrent disease, or any patient having undergone a selective therapeutic neck dissection.25 The optimal radiotherapy schedule and the fractionation remain uncertain. Most authors suggest high dose per fraction for macroscopic disease and standard fractionation for microscopic remnants.30 Clinical target volume in sinonasal melanoma often includes many critical tissues and organs, thus increasing the risk of late complications. High incidence of local and regional recurrences even after neck dissection rises questions about elective irradiation of neck lymph nodes in patients with N0 disease.28,31 We agree with this approach and recommend adjuvant irradiation of primary tumor and neck lymph nodes in patients with locally advanced sinonasal melanoma with clinically N0.23,24
4. Conclusions
-
•
In locally advanced sinonasal melanoma we had local tumor control after multimodality treatment (mediofascial resection, postoperative radiotherapy, five cycles of chemotherapy and re-surgery).
-
•
Late local relapses (in our case – two years after treatment) require careful investigation of neck lymph nodes at the time of diagnosis.
-
•
Literature data for frequent lymph node metastasis in sinonasal melanoma justify elective neck dissection.
-
•
Postoperative elective neck lymph nodes radiotherapy in patients with locally advanced sinonasal melanoma (N0) decreases the rate of late regional recurrences.
References
- 1.Narasimhan K., Kucuk O., Lin H.S. Sinonasal mucosal melanoma: a 13-year experience at a single institution. Skull Base. 2009;19(4):255–262. doi: 10.1055/s-0028-1115321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson L.D.R., Wieneke J.A., Miettinen M. Sinonasal tract and nasopharyngeal melanomas: a clinicopathologic study of 115 case with a proposed staging system. Am J Surg Pathol. 2003;27(5):594–611. doi: 10.1097/00000478-200305000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Brandwein M.S., Rothstein A., Lawson W. Sinonasal melanoma: a clinicopathologic study of 25 cases and literature meta-analysis. Arch Otolaryngol – Head Neck Surg. 1997;123(3):290–296. doi: 10.1001/archotol.1997.01900030064008. [DOI] [PubMed] [Google Scholar]
- 4.Andersen L.J., Berthelsen A., Hansen H.S. Malignant melanoma of the upper respiratory tract and oral cavity. J Otolaryngol. 1992;21(3):180–185. [PubMed] [Google Scholar]
- 5.Larson D.D., Larson J.D. Head and neck melanoma. Clin Plast Surg. 2010;37:73–77. doi: 10.1016/j.cps.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 8.Patel S.G., Prasad M.L., Escrig M. Primary mucosal malignant melanoma of the head and neck. Head Neck. 2002;24:247–257. doi: 10.1002/hed.10019. [DOI] [PubMed] [Google Scholar]
- 9.Prasad M.L., Patel S.G., Huvos A.G. Primary mucosal melanoma of the head and neck: a proposal for microstaging localized, stage I (lymph node-negative) tumors. Cancer. 2004;100:1657. doi: 10.1002/cncr.20201. [DOI] [PubMed] [Google Scholar]
- 10.Prasad M.L., Busam K.J., Patel S.G. Clinicopathologic differences in malignant melanoma arising in oral squamous and sinonasal respiratory mucosa of the upper aerodigestive tract. Arch Pathol Lab Med. 2003;127:997–1002. doi: 10.5858/2003-127-997-CDIMMA. [DOI] [PubMed] [Google Scholar]
- 12.Kienstra M.A., Padhya T.A. Head and neck melanoma. Cancer Control. 2005;12(4):242–247. doi: 10.1177/107327480501200406. [DOI] [PubMed] [Google Scholar]
- 13.Krengli M., Jereczek-Fossa A.B., Kaanders J.H.A.M. What is the role of radiotherapy in the treatment of mucosal melanoma of the head and neck? Crit Rev Oncol/Hematol. 2008;65:121–128. doi: 10.1016/j.critrevonc.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 14.Mucke T., Holzle F., Kesting M.R. Tumor size and depth in primary malignant melanoma in the oral cavity influences survival. Int J Oral Maxillofac Surg. 2009;67:1409–2115. doi: 10.1016/j.joms.2008.12.021. [DOI] [PubMed] [Google Scholar]
- 15.Rapini R.P., Goliz L.E., Greer R.O., Jr. Primary malignant melanoma of the oral cavity. A review of 177 cases. Cancer. 1985;55:1543. doi: 10.1002/1097-0142(19850401)55:7<1543::aid-cncr2820550722>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 16.Meleti M., Leemans C.R., deBree R. Head and neck head mucosal melanoma: experience with 42 patients, with emphasis on the role of postoperative radiotherapy. Head Neck. 2008;30:1543–1551. doi: 10.1002/hed.20901. [DOI] [PubMed] [Google Scholar]
- 17.Tanaka N., Mimura M., Ogi K. Primary malignant melanoma of the oral cavity: assessment of outcome from the clinical records of 35 patients. Int J Oral Maxillofac Surg. 2004;33:761. doi: 10.1016/j.ijom.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 18.Tanaka N., Amagasa T., Iwaki H. Oral malignant melanoma in Japan. Oral Surg Oral Med Oral Pathol. 1994;78:81. doi: 10.1016/0030-4220(94)90121-x. [DOI] [PubMed] [Google Scholar]
- 19.Wagner J.D., Gordon M.S., Chuang T.Y. Current therapy of cutaneous melanoma. Plast Reconstr Surg. 2000;105:1774–1799. doi: 10.1097/00006534-200004050-00028. [DOI] [PubMed] [Google Scholar]
- 21.McMasters K.M., Reintgen D.S., Ross M.I. Sentinel lymph node bopsy or melanoma controversy despite widespread agreement. J Clin Oncol. 2001;19:2851–2855. doi: 10.1200/JCO.2001.19.11.2851. [DOI] [PubMed] [Google Scholar]
- 22.Aydin A.A., Okudan B., Aydin Z.D. Lymphoscintigraphic drainage patterns of the auricle in healthy subjects. Head Neck. 2005;27:893–900. doi: 10.1002/hed.20255. [DOI] [PubMed] [Google Scholar]
- 23.Mendenhall W.M., Amdur R.J., Hinermann R.W. Head and neck mucosal melanoma. Am J Clin Oncol. 2005;28:626. doi: 10.1097/01.coc.0000170805.14058.d3. [DOI] [PubMed] [Google Scholar]
- 24.Penel N., Mallet Y., Mirabel X. Head and neck mucosal melanoma. Am J Clin Oncol. 2005;26:626–630. doi: 10.1097/01.coc.0000170805.14058.d3. [DOI] [PubMed] [Google Scholar]
- 25.Ballo T., Garden A.S., Myers J.N. Melanoma metastatic to cervical lymphnode: can radiotherapy replice formal dissection after local excision of nodal disease? Head Neck. 2005;27:718–721. doi: 10.1002/hed.20233. [DOI] [PubMed] [Google Scholar]
- 26.Owens J.M., Roberts D.B., Myers J.N. The role of postoperative radiotherapy in the treatment of mucosal melanomas of the head and neck region. Arch Otolaryngol – Head Neck Surg. 2003;129:864–868. doi: 10.1001/archotol.129.8.864. [DOI] [PubMed] [Google Scholar]
- 27.Temam S., Mamelle G., Maranas P. Postoperative radiotherapy for primary mucosal melanomas of the head and neck. Cancer. 2005;103:313–319. doi: 10.1002/cncr.20775. [DOI] [PubMed] [Google Scholar]
- 28.Krengli M., Masini L., Kaanders J.H.A.M. Radiotherapy in the treatment in the mucosal melanomas of the upper aero-digestive tract. A rare cancer network study. Int J Radiat Oncol Biol Phys. 2006;65:751–759. doi: 10.1016/j.ijrobp.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 30.Wada H., Nemoto K., Ogawa Y. A multi-institutional retrospective analysis of external radiotherapy for mucosal melanoma of the head and neck in northern Japan. Int J Radiat Oncol Biol Phys. 2004;59:495–550. doi: 10.1016/j.ijrobp.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 31.Lee S.P., Shimizu K.T., Tran L.M. Mucosal melanoma of head and neck. The impact of local control on survival. Laryngoscope. 1994;104:121. doi: 10.1288/00005537-199402000-00001. [DOI] [PubMed] [Google Scholar]


