Abstract
Aim
To investigate the clinical application of a technique for patient set-up verification in breast cancer radiotherapy based on a 3D surface image registration system.
Background
Accurate and reproducible patient set-up is a prerequisite to correctly deliver fractionated radiotherapy. Various approaches are available to verify and correct patient setup for 3D image acquisition in a radiation treatment room.
Materials and methods
The study analyzed the setup reproducibility of 15 patients affected by breast cancer and candidates for conformal radiotherapy by using the AlignRT system (VisionRT, London, UK). At the initial setup, electronic portal imaging device (EPID) images were compared with Digitally Reconstructed Radiographs (DRRs) and a reference three-dimensional (3D) surface image was obtained by AlignRT. Surface images were acquired prior to every subsequent setup procedure. The systematic and random errors along longitudinal and vertical directions were measured and compared for the two systems.
Results
The procedure for surface registration, image acquisition and comparison with the reference image took less than 1 min on average. The T test for systematic error showed no significant difference between the 2 verification systems along the longitudinal (p = 0.69) and vertical (p = 0.67) axes. The T-test for random error showed a significant difference between the 2 systems along the vertical axis (p = 0.05).
Conclusion
AlignRT is fast, simple, non-invasive and seems to be reliable in detecting patient setup errors. Our results suggest that it could be used to assess the setup reproducibility for breast cancer patients.
Keywords: Surface imaging, Patient setup, Radiotherapy, Breast cancer
1. Background
Accurate and reproducible patient setup is a prerequisite to correctly deliver fractionated radiotherapy. Minimizing the position uncertainties in order to reduce the safety margins around the clinical target volume (CTV), i.e. the planning target volume (PTV), can be of great relevance especially when using highly conformal techniques such as intensity modulated radiation therapy (IMRT).1–3
Various approaches are available to verify and correct patient setup for three-dimensional (3D) image acquisition in a radiation treatment room. These include standard megavoltage electronic portal imaging device (EPID),4 megavoltage and kilovoltage computed tomography (CT) by helical and cone beam techniques5 as well as ultrasound systems.6 Alternatively, optical systems can be used to reconstruct the 3D coordinates of markers fixed to the patient.7,8 The latter technique, which requires no additional radiation exposure, has been employed in various tumour locations9,10 and can be of particular relevance when applied to targets located near the skin and the subcutaneous tissues like mammary gland.11
2. Aim
In the present study, we investigated a method for verifying and correcting treatment setup errors using a 3D surface imaging system installed in the treatment room to facilitate image-guided radiotherapy in breast cancer patients.
3. Materials and methods
3.1. Image acquisition system
The commercially available 3D surface image registration system AlignRT (Vision RT, London, UK) was installed in a treatment room equipped with a linear accelerator with multileaf collimator and amorphous silicon EPID (see Fig. 1). The AlignRT system consists of two imaging pods mounted on the ceiling under an oblique angle of 30° with respect to the treatment table. Each pod containing two stereo-vision cameras, a texture camera, a clear flash, a flash used for speckle projection and a slide projector for speckle projection, acquires 3D surface data over approximately 120° in the axial plane, from midline to posterior flank. The data are merged to form a single 3D surface image of the patient. The system includes software designed to facilitate patient setup by surface-model acquisition and alignment by surface matching with a reference image that can be obtained at the time of first treatment session by extraction of the surface image from CT data. In order to optimize the alignment process, the software is able to calculate the optimal rigid-body transformation (couch translation and rotation) that brings the surface model of the daily treatment fraction into congruence with the reference surface.
Fig. 1.

Photograph of the two camera pods (black arrows) of the surface registration system, mounted on the ceiling of the treatment room. The linear accelerator is also shown.
Before starting the clinical activity, a test was performed in order to verify the performance of the system in terms of precision and reproducibility of the measures as described in a previous article.10 An anthropomorphic phantom was positioned on the treatment table and aligned with the three laser system of the treatment room. Known shifts of the treatment table along the three axes were checked by the AlignRT with measurements for each axis X, Y and Z. The system demonstrated high accuracy and reproducibility with measured errors of less than 1 mm. A quality assurance procedure was adopted for the AlignRT system by daily checks to calibrate the cameras to the coordinates of the linear accelerator using a dedicated calibration plate with a printed grid.
3.2. Clinical series
Fifteen patients aged from 36 to 76 years (mean 55 years), operated by conservative surgery for breast cancer, were enrolled in the present study after having given their informed consent following the rules of our institution. All patients underwent simulation by helical CT-scan (Lightspeed, General Electric, Milwaukee, WI, USA) in a supine position with contiguous slices of 5 mm in thickness. The breast Posiboard system (CIVCO, Kalona, USA) was used for patient setup. Three skin tattoos, two anteriors and one lateral, were marked for position verification by alignment to the 3 laser system.
CT data were transferred to the treatment planning system Pinnacle 8.0 (ADAC, Philips, Eindhoven, the Netherlands). Target volumes and organs at risk (OARs) (ipsilateral lung and heart) were outlined. The CTV was defined as the entire breast tissue starting 5 mm below the skin. The PTV was obtained by adding 10 mm margin to the CTV, except in the direction of the skin. Treatment consisted of 3D-conformal radiotherapy using tangential fields to a total dose of 50 Gy in 25 fractions in 10 cases and of 45 Gy in 20 fractions in 5 cases. Subsequently, all patients received 9 Gy electron boost dose to the surgical bed delivered in 3 fractions of 3 Gy each.
3.3. Image acquisition
During the first treatment session, portal images of the two tangential treatment fields were acquired with a double exposure and compared with the treatment plan Digitally Reconstructed Radiographs (DRRs). At the same time, a reference surface image of the thorax (from the supraclavicular region to submammary sulcus) was obtained and recorded by the AlignRT system. Surface images were acquired daily during every setup procedure and co-registered with the reference image obtained at the first treatment session. Portal images were acquired in the first 3 days and then once a week. The setup errors detected by EPID were retrospectively compared with those produced by the surface imaging system. Setup deviations measured by EPID were decomposed along the main axis of the treatment tangential fields, and the setup errors measured by means of the AlignRT system were acquired in the treatment room reference system, which corresponds to the International Electrotechnical Commission (IEC) coordinates of the treatment unit. In order to compare the setup errors measured from the 3D mismatch of patient surfaces and those obtained by the co-registration of 2D portal images with DRR, the setup error 3D vectors calculated by AlignRT were projected on the 2D reference frame described by the plane of the images passing through the isocentre. The error component along the axis oriented along the cranio-caudal direction was called “longitudinal error” and that along the other image axis oriented along the anterior-posterior direction was called “vertical error”.
3.4. Statistical analysis
Systematic and random errors along the main field axes from EPID images and surface co-registration (AlignRT) were calculated and reported as mean and standard deviation (SD).
The T-test for paired data was used to analyze systematic and random errors.
The correlation between the positioning errors measured by AlignRT and EPID images were performed by linear regression and by Spearman method.
4. Results
The procedure for surface registration, image acquisition, and comparison with the reference image took less than 1 min on average.
The mean systematic and random errors detected by AlignRT along the main axes (longitudinal and vertical) are reported in Table 1 and in Fig. 2a and b.
Table 1.
Systematic and random errors (mm) along vertical and longitudinal axis.
| Positioning system | Field axis | Systematic error (mean ± SD) | Random error (mean ± SD) |
|---|---|---|---|
| EPID | Vertical | 0.10 ± 0.08 | 0.12 ± 0.04 |
| ALIGNRT | Vertical | 0.12 ± 0.26 | 0.16 ± 0.06 |
| EPID | Longitudinal | 0.10 ± 013 | 0.13 ± 0.07 |
| ALIGNRT | Longitudinal | 0.07 ± 0.17 | 0.18 ± 0.07 |
Fig. 2.
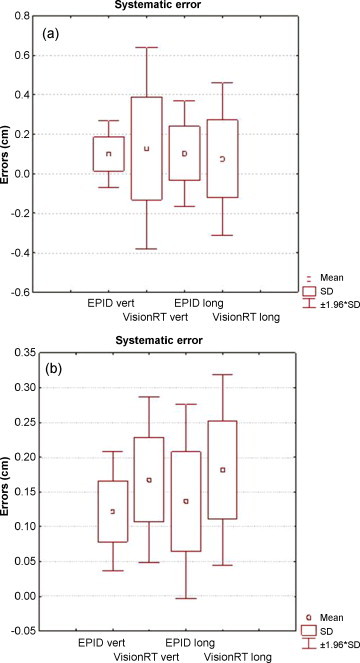
Representation of systematic (a) and random (b) errors along the main field axis from EPID images and surface co-registration.
The mean systematic error for AlignRT was 1.2 mm (SD = 2.8 mm) along the vertical axis and 0.7 mm (SD = 1.9 mm) along the longitudinal axis. The mean random error was 1.7 mm (SD = 0.6 mm) along the vertical axis and 1.8 mm (SD = 0.7 mm) along the longitudinal axis.
Random errors along vertical and longitudinal directions were larger for AlignRT than for EPID.
The T test for systematic error showed no significant difference between measures by EPID and by AlignRT along the longitudinal (p = 0.69) and vertical (p = 0.67) axes. The T test for random error showed a significant difference between the two systems along the vertical axis (p = 0.05), but not along the longitudinal axis (p = 0.15).
The correlation factor calculated by means of linear regression between the positioning errors measured by AlignRT and EPID images was 0.26 along the vertical axis and −0.26 along the longitudinal axis. The errors measured with AlignRT and EPID were less than 2 mm; therefore, no correlation between the two data sets emerged from linear regression method.
5. Discussion
A number of studies using video-surface imaging systems for patient setup verification have been published over the last few years.9–12 Some of them were performed on breast cancer and intra-thoracic tumours and showed that surface imaging is a reliable method for patient position verification and may improve the precision of setup and reduce the effects of respiratory motion. In the present study, we applied a 3D surface image registration system to verify the position of the mammary gland during fractionated radiotherapy.
This technique aims to verify the patient position before each treatment session. As a matter of fact, optical imaging may only provide information on the external anatomy, but is completely non-invasive and requires zero radiation dose. Its effective use requires knowledge of the relationship between the position of the target and the external anatomy.
In our experience, the AlignRT system was able to detect systematic and random errors of less than 2 mm along the main field axis in tangential beams setup.
In the study of Bert et al.,13 the authors used the same 3D surface patient setup system. The reference surface model was selected to be the surface model acquired at the first treatment fraction after portal film alignment. Simulated setup with the AlignRT system yielded mean displacement of 1 mm (SD = 1.2 mm), while the displacement was 7.3 mm (SD = 4.4 mm) and 7.6 mm (SD = 4.2 mm) for laser and portal film, respectively. Distance analysis revealed mean distances of 3.7 mm (SD = 4.9 mm), 4.3 mm (SD = 5.6 mm), and 1.6 mm (SD = 2.4 mm) for laser, portal film, and AlignRT, respectively. The alignment of the 3D breast surface achieved by stereo-photogrammetry showed greater breast topology congruence than for patients set up by laser or portal imaging.
Our study comparing EPID with AlignRT showed a difference between the two system of 0.2 mm for systematic error and 0.4 mm for random error in the anterior–posterior (longitudinal error) and superior–inferior (vertical error) direction. These results were similar to those of Spadea et al.,14 who investigated the clinical application of a technique for patient setup verification in breast cancer RT based on the 3D localization of a hybrid configuration of surface control points. The application of the corrective spatial transformation estimated by the registration procedure led to a significant improvement of patient setup. Median value of 3D errors affecting three additional verification markers within the irradiation field decreased from 5.7 to 3.5 mm and errors variability (25–75%) decreased from 3.2 to 2.1 mm.
The applicability and the technical performance of the AlignRT system was analyzed also by Schoffel et al.9 Measurements were performed in a rigid anthropomorphic phantom as well as in healthy volunteers. The system showed a high stability and detected pre-defined shifts of the phantom and healthy volunteers with an accuracy of 0.40 ± 0.26 mm and 1.02 ± 0.51 mm, respectively (spatial deviation between pre-defined shift and suggested correction). These results demonstrate that the camera system provides highly accurate setup corrections in a phantom and in healthy volunteers, similar to those observed in our study.
In the present study, random errors were systematically larger for AlignRT (1.7 mm) than for EPID (1.2 mm) and the difference showed a trend for vertical direction with a p value of 0.05, although such difference was not clinically relevant. This variation could be explained by the fact that small soft tissue changes during RT may not have been visible by portal imaging. A similar finding was reported also by Bert et al.13 who measured changes in arm position from day to day. These changes were likely to influence breast deformation that could not be detected by portal imaging.
In the present study, we used the acquisition at the time of the first session as a reference image, since we did not have a surface image system in the simulation room and we decided to avoid any possible error in the matching of the CT reconstruction data and the Align-RT data. The latter procedure could actually be critical in relation to a change of the coordinate system from CT to surface imaging system, as observed by Bert et al.13
Ideally, the surface of the reference setup is acquired during the treatment planning CT using a second camera system installed in the CT room. This would help to reduce both random and systematic setup errors.15,16 This may be used to monitor the accuracy of the setup, similar to the comparison of portal images with DRRs.
A limitation of the present study is the absence of breathing control. Breathing can influence patient setup by introducing a variation as large as the breathing amplitude of the surface used.
Bert et al.13 analyzed this aspect: free breathing can affect the measured surface models and, consequently, lead to incorrect predictions for the realignment. The surface registration system could minimize motion artefacts by performing gated surface imaging, which resulted in surface-model capture at the same respiratory phase. This feature is still a compromise because breathing studies show that respiration baseline can drift with time, e.g. when the patient relaxes on the couch after a few minutes.17 Gated captures were implemented toward the latter part of this patient study but were not used to allow comparison of the data acquired previously. Through post-processing of continuous-acquisition data, the breathing signal could be extracted and the analysis showed a peak-to-peak amplitude of 1.9 ± 1.1 mm over the breast for the combined results of all patients at isocentre. Mageras and Yorke17 studied the influence of breathing in the positioning of breast patients as well. They reported that controlled acquisition at end of exhale decreased marker displacement only slightly in comparison to free-breathing measurement. This finding was consistent with small-breathing peak-to-peak amplitude.
6. Conclusions
The surface imaging system AlignRT seems to be reliable in detecting setup errors in breast cancer patients. Our results suggest that the system could be used to assess the reproducibility of patient setup in fractionated radiotherapy for breast cancer. In particular, it appears to be fast, simple and non invasive. After EPID acquisition at the beginning of the radiation treatment, portal images might be replaced with the AlignRT surface images for daily controls. An additional advantage of such optical system not using ionizing radiation is that images may be easily acquired before and after applying the setup correction without additional dose to the patient.
References
- 1.Jain P., Marchant T., Green M. Inter-fraction motion and dosimetric consequences during breast intensity-modulated radiotherapy (IMRT) Radiother Oncol. 2009;90:93–98. doi: 10.1016/j.radonc.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 2.van Mourik A., van Kranen S., den Hollander S., Sonke J.J., van Herk M., van Vliet-Vroegindeweij C. Effects of setup errors and shape changes on breast radiotherapy. Int J Radiat Oncol Biol Phys. 2010 doi: 10.1016/j.ijrobp.2010.07.032. [DOI] [PubMed] [Google Scholar]
- 3.Sas-Korczyńska B., Śladowska A., Rozwadowska-Bogusz B. Comparison between intensity modulated radiotherapy (IMRT) and 3D tangential beams technique used in patients with early-stage breast cancer who received breast-conserving therapy. Rep Pract Oncol Radiother. 2010;15:79–86. doi: 10.1016/j.rpor.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith R.P., Bloch P., Harris E.E. Analysis of interfraction and intrafraction variation during tangential breast irradiation with an electronic portal image device. Int J Radiat Oncol Biol Phys. 2005;54:57–64. doi: 10.1016/j.ijrobp.2004.10.022. [DOI] [PubMed] [Google Scholar]
- 5.Groh B.A., Siewerdsen J.H., Drake D.G., Wong J.W., Jaffray D.A. A performance comparison of flat-panel imager-based MV and kV cone-beam CT. Med Phys. 2002;29:967–975. doi: 10.1118/1.1477234. [DOI] [PubMed] [Google Scholar]
- 6.Langen K.M., Pouliot J., Anezinos C. Evaluation of ultra-sound-based prostate localization for image-guided radiotherapy. Int J Radiat Oncol Biol Phys. 2003;57:635–644. doi: 10.1016/s0360-3016(03)00633-3. [DOI] [PubMed] [Google Scholar]
- 7.Baroni G., Garibaldi C., Riboldi M. A 3D optoelectronic analysis of interfractional patient setup variability in frameless extracranial stereotactic radiotherapy. Int J Radiat Oncol Biol Phys. 2003;64:635–642. doi: 10.1016/j.ijrobp.2005.07.964. [DOI] [PubMed] [Google Scholar]
- 8.Liebler T., Hub M, Scanner C., Schlegel W. An application framework for computer-aided patient positioning in radiation therapy. Med Inform Internet Med. 2003;28:161–182. doi: 10.1080/14639230310001613458. [DOI] [PubMed] [Google Scholar]
- 9.Schoffel P.J., Harms W., Sroka-Perez G. Accuracy of a commercial optical 3D surface imaging system for realignment of patients for radiotherapy of the thorax. Phys Med Biol. 2007;52:3949–3963. doi: 10.1088/0031-9155/52/13/019. [DOI] [PubMed] [Google Scholar]
- 10.Krengli M., Gaiano S., Mones E. Reproducibility of patient setup by surface image registration system in conformal radiotherapy of prostate cancer. Radiat Oncol. 2009;4:9. doi: 10.1186/1748-717X-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gierga D.P., Riboldi M., Turcotte J.C. Comparison of target registration errors for multiple image-guided techniques in accelerated partial breast irradiation. Int J Radiat Oncol Biol Phys. 2008;70:1239–1246. doi: 10.1016/j.ijrobp.2007.11.020. [DOI] [PubMed] [Google Scholar]
- 12.Bert C., Metheany K.G., Doppke K.P., Chen G.T.Y. A phantom evaluation of a stereo-vision surface imaging system for radiotherapy patient setup. Med Phys. 2005;32:2753–2761. doi: 10.1118/1.1984263. [DOI] [PubMed] [Google Scholar]
- 13.Bert C., Metheany K.G., Doppke K.P., Taghian A.G., Powell S.N., Chen G.T.Y. Clinical experience with a 3D surface patient setup system for alignment of partial-breast irradiation patients. Int J Radiat Oncol Biol Phys. 2006;64:1265–1274. doi: 10.1016/j.ijrobp.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 14.Spadea M.F., Baroni G., Riboldi M. Patient set-up verification by infrared optical localization and body surface sensing in breast radiation therapy. Radiother Oncol. 2006;79:170–178. doi: 10.1016/j.radonc.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 15.Van Herk M. Errors and margins in radiotherapy. Semin Radiat Oncol. 2004;14:52–64. doi: 10.1053/j.semradonc.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Bortfeld T., van Herk M., Jiang S.B. When should systematic patient positioning errors in radiotherapy be corrected? Phys Med Biol. 2002;47:297–302. doi: 10.1088/0031-9155/47/23/401. [DOI] [PubMed] [Google Scholar]
- 17.Mageras G.S., Yorke E. Deep inspiration breath hold and respiratory gating strategies for reducing organ motion in radiation treatment. Semin Radiat Oncol. 2004;14:65–75. doi: 10.1053/j.semradonc.2003.10.009. [DOI] [PubMed] [Google Scholar]


