Abstract
Superior vena cava syndrome (SVCS) is characterized by a spectrum of clinical findings that result from the occlusion of the superior vena cava (SVC), usually caused by extracaval compression of the SVC by either a bronchogenic tumor or an enlarged mediastinal lymph node. Most efforts at treatment for SVCS are palliative, and long-term survival for malignancy-related SVCS is very low. Therefore, radiotherapy treatment is usually delivered with palliative intent utilizing hypofractionated regimens. The use of high dose per fraction may result in more rapid and more durable responses to treatment. Similarly, the high dose per fraction utilized in stereotactic body radiotherapy (SBRT) has been proven highly efficacious in treating early stage non-small cell lung cancer (NSCLC). Here we report the first reported case of a patient with SVCS from NSCLC successfully treated with SBRT to alleviate SVCS.
Keywords: Stereotactic, Superior vena cava syndrome, SBRT, SVCS
1. Background
Superior vena cava syndrome (SVCS) is characterized by a spectrum of clinical findings that result from the occlusion of the superior vena cava (SVC). The typical manifestations generally include edema and distention of the veins of the upper chest wall, upper extremities, neck, face and head. As symptoms progress patients may experience dyspnea, cough, stridor, headache or neurologic dysfunction related to cerebral edema.
Most cases of SVCS are caused by extracaval compression of the SVC by either a bronchogenic tumor or an enlarged mediastinal lymph node. Specifically, right paratracheal lymph nodes are the most common nodal site involved. Radiotherapy or chemotherapy is most commonly utilized to treat the offending lesion with the goal of relieving compression and restoring normal, physiologic flow through the SVC. The choice of which of these modalities to employ is largely dependent upon the histology of the obstructing lesion. Patients with chemosensitive tumors such as small cell lung cancers (SCLC) are typically treated with chemotherapy, while less sensitive tumors such as non-small cell lung cancers (NSCLC) are typically treated with radiotherapy.
Most efforts at treatment for SVCS are palliative, and long-term survival for malignancy-related SVCS is very low. Therefore, radiotherapy treatment is usually delivered with palliative intent utilizing hypofractionated regimens. The use of high dose per fraction may result in more rapid and more durable responses to treatment. Similarly, the high dose per fraction utilized in stereotactic body radiotherapy (SBRT) has been proven highly efficacious in treating early stage NSCLC. Here we report the case of a patient with SVCS from NSCLC treated with SBRT in an attempt to alleviate his SVCS and simultaneously offer definitive treatment for his underlying malignancy.
2. Case report
A previously healthy 82-year-old white male presented to the hospital with the complaint of a 3–4 day history of swelling of the face, neck, and left arm. The patient denied any shortness of breath, stridor, pain, or neurologic changes and otherwise felt well. Despite his symptoms he was able to carry on with his normal activities of daily living. He did however admit to a chronic, productive cough, and also endorsed a smoking history of approximately 70-pack-years.
At the time of presentation, physical exam was significant for edema of the bilateral upper extremities and face associated with well-formed collateral vessels on the anterior chest wall (Fig. 1).
Fig. 1.

Anterior chest wall collateral vessels.
Due to a high clinical suspicion for SVCS, a thoracic CT with contrast was performed, revealing a 2.5 cm mediastinal mass consistent with a pathologically enlarged right paratracheal lymph node completely obstructing the SVC (Fig. 2). Well-formed collateral vessels bypassing the obstructed portion of the SVC were noted as well.
Fig. 2.

Coronal reconstruction of a CT of the thorax with contrast revealing occlusion of the superior vena cava secondary to a right paratracheal lymph node. Collateral vessels are apparent proximal to the obstructing lesion.
The patient was clinically stable, therefore complete work-up and staging was performed. Endobronchial ultrasound guided biopsy of the offending right paratracheal lymph node revealed squamous cell carcinoma. PET/CT revealed increased uptake within the obstructing lymph node with no other evidence of disease throughout.
Given the patient's small overall volume of disease, small offending lesion size, and evidence of possible improved outcomes with large dose per fraction, SBRT was chosen as the optimal treatment modality. The intent of treatment was to both palliate his SVCS and definitively treat his NSCLC.
The patient underwent respiratory gated CT simulation with images acquired during passive breathing, inhalation and exhalation. To aid with immobilization a custom vacuum bag was conformed to the patients head, neck, thorax, abdomen and pelvis. The offending lesion was then delineated on each phase of the planning CT scan as gross tumor volume (GTV). All three identified GTVs were then fused to generate an internal target volume (ITV). Given that the lesion did not move with respiration, and was located wholly within the mediastinum, an expansion of 3 mm around the ITV was used to construct the planning target volume (PTV). He was then treated with three-dimensional conformal radiotherapy using 6 MV photons from a Varian Trilogy linear accelerator (Varian, Palo Alto, CA). Twelve coplanar beams were used to deliver a total dose of 50 Gy in five fractions of 10 Gy each, administered every other day. Dose was prescribed to the 95% isodose line covering the PTV (Fig. 3). Following his second treatment he was noted to have an appreciable response to therapy. His facial and upper extremity edema had resolved completely by the completion of treatment.
Fig. 3.
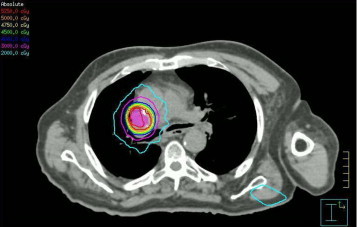
Axial dose distribution of treatment plan.
The patient reported no acute side effects from his radiation treatment. At the time of last follow-up he was 3 months out from completion of therapy. At the time he reported normal breathing without dyspnea or chest pain. His upper extremity edema had resolved although the collaterals evident on his anterior chest wall remained.
3. Discussion
It is reported that up to 90% of SVCS cases are due to malignancy.1 Of those cases, approximately 80% are secondary to a primary bronchogenic carcinoma. SVCS is actually the first presenting symptom in 10% of patients with SCLC and in 1.7% of patients with NSCLC.2 The obstruction in malignancy-related SVCS is usually caused by local extension of a right upper lobe tumor or, more commonly, enlarging mediastinal adenopathy with the right paratracheal node being most frequently involved.3
The prognosis is generally poor for malignancy-related SVCS, with studies demonstrating average survival time after diagnosis of SVCS due to NSCLC of 5–12 months.4,5 In NSCLC, the response to therapy for SVCS has not been as favorable as when related to SCLC. In a systematic review, external beam radiotherapy (EBRT) offered complete resolution of SVCS in 78% of patients with SCLC and in 63% of patients with NSCLC.1 NSCLC has been demonstrated to be somewhat more responsive to radiation therapy than chemotherapy, with complete relief obtained in 63% and 58% of patients, respectively.1
The rate of response of the symptoms of SVCS to EBRT is variable and highly dependent on the tumor histology. In general, there is usually some symptomatic improvement evident within 72 h after beginning EBRT, but some cases have been documented wherein relief was not provided for up to 4 weeks. Multiple studies have reported that approximately 20% of patients will exhibit no response to EBRT.1,6,7 However, high initial EBRT doses may result in a more rapid and more durable response to therapy. In addition, survival appears to be prolonged in those who respond within 30 days of initiating therapy.4
SBRT is a relatively new development with excellent outcomes reported for early stage lung cancer. Utilizing this technique to deliver high doses per fraction has resulted in very high rates of local control.8 Given the small volume and focality of disease, this patient offered a unique clinical scenario to achieve both relief of SVCS and potentially definitive treatment. For those patients with centrally located tumors, excessive toxicity has been reported with very large doses per fraction.9 This excessive toxicity prompted an ongoing radiation therapy oncology group (RTOG) dose escalation trial for patients with centrally located tumors. Therefore, the patient was electively treated with the starting dose as per the current dose escalation protocol. Thus far he has had resolution of his SVCS and represents the first documented case in the literature of utilizing SBRT for the treatment of SVCS.
4. Summary
Superior vena cava syndrome (SVCS) is a clinical syndrome that affects many patients during their course of cancer treatment, and radiotherapy is a major modality of therapy for many of these patients. Higher radiation doses per fraction have been associated with improved outcomes. SBRT may be ideal for select patients who present with SVCS.
Conflicts of interest
None declared.
Financial disclosure
None declared.
References
- 1.Rowell N.P., Gleeson F.V. Steroids, radiotherapy, chemotherapy and stents for superior vena caval obstruction in carcinoma of the bronchus: a systematic review. Clin Oncol. 2002;14:338–351. doi: 10.1053/clon.2002.0095. [DOI] [PubMed] [Google Scholar]
- 2.Kvale P.A., Selecky P.A., Prakash U.B.S. Palliative care in lung cancer. ACCP evidence-based clinical practice guidelines [2nd edition] Chest. 2007;132:368S–403S. doi: 10.1378/chest.07-1391. [DOI] [PubMed] [Google Scholar]
- 3.Schraufnegal D., Hill R., Leech J. Superior vena caval obstruction. Is it a medical emergency? Am J Med. 1981;70:1169–1174. doi: 10.1016/0002-9343(81)90823-8. [DOI] [PubMed] [Google Scholar]
- 4.Martins S.J., Pereira J.R. Clinical factors and prognosis in non-small cell lung cancer. Am J Clin Oncol. 1999;22:453. doi: 10.1097/00000421-199910000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong B.A., Perez C.A., Simpson J.R., Hederman M.A. Role of irradiation in the management of superior vena cava syndrome. Int J Radiat Oncol Biol Phys. 1987;13:531–539. doi: 10.1016/0360-3016(87)90068-x. [DOI] [PubMed] [Google Scholar]
- 6.Chen J.C., Bongard F., Klein S.R. A contemporary perspective on superior vena cava syndrome. Am J Surg. 1990;160:207. doi: 10.1016/s0002-9610(05)80308-3. [DOI] [PubMed] [Google Scholar]
- 7.Mose S., Stabik C., Eberlein K. Retrospective analysis of the superior vena cava syndrome in irradiated cancer patients. Anticancer Res. 2006;26:4933. [PubMed] [Google Scholar]
- 8.Timmerman R., Paulus R., Galvin J. Stereotactic body radiation therapy for inoperable early stage lung cancer. JAMA. 2010;303(11):1070–1076. doi: 10.1001/jama.2010.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Timmerman R., McGarry R., Yiannoutsos C. Excessive toxicity when treating central tumors in a phase II study of stereotactic body radiation therapy for medically inoperable early-stage lung cancer. JCO. 2008;24(30):4833–4839. doi: 10.1200/JCO.2006.07.5937. [DOI] [PubMed] [Google Scholar]


