Abstract
Background
Avascular necrosis (AVN) refers to the death of osteocytes and osteoblasts. Sites such as the femoral head, the head of the humerus and the mandibula with restricted access to local blood supply are particularly vulnerable to osteonecrosis.
A combination of several factors is responsible for ischaemia and is associated with AVN: corticosteroids, alcohol abuse, Cushing's syndrome, SLE, systemic vasculitis, RA, scleroderma, haemoglobinopathies, radiotherapy. Management is based on proper diagnosis and treatment – conservative, pharmacological or surgical.
Radiotherapy has become an integral part of the therapeutic programme of cancer patients. However, early and late after-effects of irradiation still constitute a significant issue in clinical practice.
Aim
The aim of this report is to present two cases of acetabular protrusion and femoral head deformities after a therapeutic pelvic irradiation and draw physicians’ attention to that clinical problem which continues to be underestimated.
Materials and methods
This report documents two cases of acetabular protrusion and femoral head deformities after a therapeutic pelvic radiation.
Results
Avascular necrosis (AVN) constitutes a severe and challenging long-term complication in radiation oncology.
Conclusion
It is necessary to take into account bone structures among organ at risk (OAR) involved in irradiation fields. The detailed analysis of the dose distribution and the use of collimators allow to decrease the total dose to OAR.
An adequate management, early diagnosis and prompt, proper treatment may protect patients from long-term morbidities.
Keywords: Osteoradionecrosis, Aseptic necrosis, Avascular necrosis, Radiotherapy
1. Background
Nowadays, radiotherapy has become an integral part of the therapeutic program of cancer patients. It represents a highly effective and curative treatment modality for cervical cancer, urinary bladder, prostate and rectum. Modern irradiation planning techniques enable very accurate dose distribution and precise beam delivery. Rapid advance in radiobiology and physics have had a great impact on understanding normal tissue toxicities. However, early and late effects of irradiation still constitute significant issue in clinical practice. One of the most severe and challenging long-term complication in radiotherapy is osteonecrosis, also called aseptic necrosis, ischemic necrosis or avascular necrosis (AVN).
This report documents extensive asymmetric bone abnormalities with an acetabular protrusion and femoral head deformities, after a therapeutic pelvic radiation.
There is no particular safe dose or tolerance dose. The probability of radiation induced changes in bone (osteitis, fracture) depends on many factors, such as dose per fraction, total dose, dose intensity and irradiated volume. Tolerance doses (TD5/5–TD50/5), which represent the dose of radiation that could cause no more than 5% and 50% severe complication rate within 5 years after irradiation, range from 20 to 30 Gy and 65 to 70 Gy for single and fractionated dose, respectively. As the volume of irradiated bone or cartilage decreases, the dose to produce 5% or 50% complications increases. Bone structure, its location and patient's age are also of great relevance.2,5,18
Avascular necrosis (AVN) refers to the death of osteocytes and osteoblasts. There are at least two postulated factors responsible for AVN. The cellular component depletion caused directly by radiation and the local ischemia resulting from radiotherapy-induced microvascular damage. The Rubin & Cassaret theory explains the effect of irradiation on microvasculature as a result of a slow vascular leakage of the protein-rich fluid leading to fibrosis caused by the accumulation of fibroblasts and macrophages.19 Particularly vulnerable to ischemic necrosis are the femoral head, the femoral condyles, the head of the humerus, the capitulum and the proximal parts of the scaphoid and talus.13,16 Located in the most distant parts of the bone's vascular territories, these organs have restricted access to local blood vessels. The whole process may be caused by different clinical situations, such as disturbance of the local blood supply, venous stasis, intra-vascular thrombosis and compression of capillaries by marrow swelling or a combination of several of these factors.14 Various clinical conditions are associated with increased risk of AVN. They include corticosteroid administration, alcohol abuse, Cushing's syndrome, Systemic Lupus Erythematosus (SLE), systemic vasculitis, scleroderma, polymyositis, dermatomyositis, haemoglobinopathies, radiotherapy and fractured neck of the femur.1,3,4,9
2. Aim
The aim of this report is to present two cases of acetabular protrusion and femoral head deformities after a therapeutic pelvic irradiation and draw physicians’ attention to that clinical problem which continues to be underestimated.
3. Materials and methods
3.1. Case 1
A 65-year-old woman diagnosed with cervical cancer, stage T2N1M0 was treated with radical hysterectomy and postoperative radiotherapy in May 1995. Irradiation was delivered using a cobalt 60 unit with gamma rays. Total dose of 44 Gy was delivered in 2 Gy per fraction using four field (box technique), 5 days a week. The exact dose distribution within the pelvis is not available, as a two-dimensional planning technique was used at that time. Nine years after therapy, the patient started to feel pain in her right hip and the inguinal region. The pain intensified with movement. A radiograph showed significant thinning of the bony structure in the right femoral head. Bone metastases were excluded by a bone scan which did not reveal any increase in the uptake at the right hip joint. The patient was treated with anti-inflammatory medications. Eight months later she was qualified to orthopedic operation and underwent curettage of the joint with bone graft in May 2005. Pathological examination revealed focal osteonecrosis. Although, the probability of radiation-induced AVN with dose below 50 Gy is very low, about 5% within 5 years after irradiation, a combination of several additional factors such as long-term corticosteroid therapy, bone degeneration or chemotherapy could be responsible for ischemia and bone necrosis.1,3,5,18
3.2. Case 2
A 70-year-old man suffered from urinary bladder, urotheliale carcinoma, stage T2N0M0. In 1993, the patient was treated with radiotherapy, delivered with 20 MV photons, to the total dose of 66 Gy in 2 Gy per fraction, one fraction per day, five days per week. The four-field ‘box’ technique was performed.
The patient remained asymptomatic for 3 years after treatment, without musculoskeletal symptoms. The first symptom of bone damage was a pathological fracture of the left femur's cervix. A radiograph revealed the fracture, mottled the appearance of the femoral head, osteosclerosis and cyst formations. The patient underwent a total hip arthroplasty. Pathological examination confirmed osteonecrosis. Dose volume histogram analysis showed that more than 60% volume of irradiated tissues, including both femoral heads, were irradiated with 40–54 Gy, but only 6% of femoral heads volume received dose above 48 Gy. Frontal and transversal dose distributions of the treatment are shown in Fig. 1.
Fig. 1.
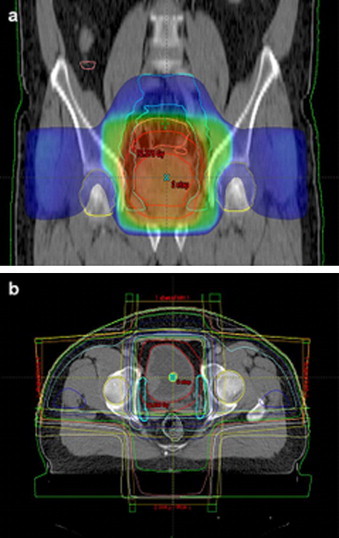
Dose distribution of irradiated urinary bladder cancer patient. (a) Frontal plane. (b) Transversal plane. The isodose 60 Gy is located out of the region of the femoral heads.
4. Results
In this study, two cases of AVN of the femoral head after pelvic radiotherapy were presented. So far, there have been few cases recognized and diagnosed, hence AVN still remains poorly defined and is an underestimated problem in oncology. In both cases, these osseous abnormalities are thought to be late consequences of the previous pelvis irradiation.6–8 Several radiographic staging systems are currently available. According to the international classification of the femoral head osteonecrosis (Association Research Circulation Osseus [ARCO]) and Ficat classification, both patients were classified as stage II AVN.2,10,17
5. Conclusion
The biological long term side effects of radiotherapy depend on many factors, but the pathologic features are consistent.2 The dose volume histogram analysis of the bladder cancer patient showed that mean dose in the region of both femoral heads did not exceed acceptable dose of 50 Gy. Four-field “box” technique has been a routine procedure used in treatment of genitourinary cancers for many years and in majority of cancer centers it is performed until now.11,12 In recent years, an increase in genitourinary cancer cases has been reported, which leads to a higher number of patients treated with pelvic radiotherapy.13 Osteonecrosis constitutes a very difficult diagnostic problem in long-term survivors, as the symptoms often appear many years after radiotherapy and patients do not associate them with past treatment.
Medical management includes avoidance of weight bearing, the use of crutches and nonsteroidal anti-inflammatory agents in early stages. Treatment of osteonecrosis is often unsuccessful and nonsurgical procedures are very limited. Analgesics can be used to minimize pain and inflammation in patients who cannot be qualified for surgery for medical or other reasons. Physiotherapy plays a significant role in bringing motion back and improving gait. The basic treatment of osteonecrosis is surgery. Currently, there are many procedures available. The choice is based on preoperative staging. Core decompression and cortical bone grafting are usually indicated in early stages. The trapdoor and allograft procedures are indicated for Ficat II or III stages. Osteotomies are performed for stages II and III. Arthrodesis and arthroplasty are used primarily for stages III and IV.1,15
Although AVN seems to be a very rare side-effect of radiotherapy, clinicians must not forget about this complication, as it may lead to severe functional impairment in patients who often have been cured of cancer. An early diagnosis and proper treatment may protect patients from long-term morbidities.
Conflict of interest statement
None declared.
Acknowledgements
The author wishes to acknowledge the help of Ms. Krystyna Trela and Mr. Jerzy Wydmański in data collection and for constructive criticisms of an earlier version of this paper.
References
- 1.Biswas T.K., Biswas S. Avascular necrosis in rheumatology practice. Reports from meetings. APLAR J Rheumatol. 2004;7(2):175–178. [Google Scholar]
- 2.Sawicka-Żukowska M., Krawczuk-Rybak M., Muszyńska-Rosłan K. Osteonecrosis—underestimated problem of children oncology. Pol Merk Lek. 2006 XXI: 123, 291. [PubMed] [Google Scholar]
- 3.Yang S.-H., Yang R.-S., Tai C.-L. Septic arthritis of the hip joint in cervical cancer patients after radiotherapy: three cases reports. J Surg. 2001;9(2):41–45. doi: 10.1177/230949900100900209. [DOI] [PubMed] [Google Scholar]
- 4.Herman I.L., Beth S.E. Radiotherapy changes of the pediatric hip. AJR. 1981;137:585–586. doi: 10.2214/ajr.137.3.585. [DOI] [PubMed] [Google Scholar]
- 5.Massin P., Duparc J. Total hip replacement in irradiated hips A retrospectice study of 71 cases. J Bone Joint Surg. 1995;77-B(6) [PubMed] [Google Scholar]
- 6.Hall F.M., Mauch P.M., Levene M.B., Goldstein M.A. Protrusio acetabuli following pelvic irradiation. AJR. 1979;132:291–293. doi: 10.2214/ajr.132.2.291. [DOI] [PubMed] [Google Scholar]
- 7.Dickie C.I., Parent A.L., Griffin A.M. Bone fractures following external beam radiotherapy and limb-preservation surgery for lower extremity soft tissue sarcoma: relationship to irradiated bone length, volume, tumor location and dose. Int Radiat Oncol Biol Phys. 2009 doi: 10.1016/j.ijrobp.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 8.Micha J.P., Goldstein B.H., Rettenmaier M.A., Cailloutte J.T., Fee M.J., Brown J.V., III Pelvic radiation necrosis and osteomyelitis following chemoradiation for advanced stage vulvar and cervical carcinoma. Gynecol Oncol. 2006;101:349–352. doi: 10.1016/j.ygyno.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 9.Lyons A., Ghazali N. Osteoradionecrosis of the jaws: current understending of its pathophysiology and treatment. Br J Oral Maxillofacial Surg. 2008;46:653–660. doi: 10.1016/j.bjoms.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 10.Herman M.P., Kopetz S., Bhosale P.R. Sacral insufficiency fractures after preoperative chemoradiation for rectal cancer: incidence, risk factors and clinical course. Int J Radiat Oncol Biol Phys. 2009:1–6. doi: 10.1016/j.ijrobp.2008.08.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dalinka M.K., Edeiken J., Barnett Finkelstein J. Complications of radiation therapy: adult bone. Semin Roengenol. 1974;IX(1) doi: 10.1016/0037-198x(74)90007-8. [DOI] [PubMed] [Google Scholar]
- 12.Fangliu G.U. Changing constituents of genitourinary cancer in recent 50 years in Beijing. Chin Med J. 2003;116(9):1391–1393. [PubMed] [Google Scholar]
- 13.Cushner M.A., Friedman R.J. Osteonecrosis of the humeral head. J Am Acad Orthop Surg. 1997;5(November (6)):339–346. doi: 10.5435/00124635-199711000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Pavelka K. Osteonecrosis. Clin Reumatol. 2000;14(2):399–414. doi: 10.1053/berh.2000.0072. [DOI] [PubMed] [Google Scholar]
- 15.Levine M., Rajadhyaksha A., Mont M. Osteonecrosis, hip. Orthopedic Surg. 2009 eMedicine Journal. [Google Scholar]
- 16.Ficat R.P. Idiopathic bone necrosis of the femoral head early diagnosis and treatment. J Bone Joint Surg [Br] 1985;67(January (1)):3–9. doi: 10.1302/0301-620X.67B1.3155745. [DOI] [PubMed] [Google Scholar]
- 17.ARCO Committee on Terminology and Staging . Schoutens pathologic conditions. Plenum Press; New York, NY: 1993. The ARCO perspective for reaching one uniform staging system for osteonecrosis. p. 375–80. [Google Scholar]
- 18.Perez C.A., Halperin H.C., Brady L.W. Princ Pract Radiat Oncol. 2007:157. [Google Scholar]
- 19.Krishnan E.C., Krishnan L., Botteron G.W., Dean R.D., Jewell W.R. Effect of irradiation on microvasculature: a quantitative study. Cancer Detect Prev. 1987;10(1–2):121–127. javascript:PopUpMenu2_Set(Menu3568005) [PubMed] [Google Scholar]


