Abstract
Study Design
Seventy-one children (23 boys and 48 girls, aged 6 to 18 year-old) with adolescent idiopathic scoliosis (AIS) between 11° and 62°, without braces, have been treated manually, only at the level of the neck.
Purpose
To ascertain that non-surgical straightening of AIS is possible (without brace).
Overview of Literature
So far no disease modifying treatment for AIS existed. Braces can only slow down worsening (and this can only be achieved if they are worn 23 hours a day). Surgery is not without important risks.
Methods
All patients have been treated exclusively with a manual therapy called Brachy-Myotherapy. This method treats spasmed (contractured) muscles by placing them in a shortening position according to a specific protocol.
Results
An average straightening of 8° of AIS was observed, with a maximum of 25°. 94% of cases improved, 67 out of 71. The worst prognosis was, the better results. The more advanced AIS was, the better the results.
Conclusions
A simple and reliable treatment of AIS is possible. AIS seems to be a compensation mechanism of the body, with the aim of keeping the ears, and thus the labyrinths, at a horizontal level for correct equilibrium. When lasting post-traumatic neck muscle contractures causing a permanent side-bending of the skull have been treated, this compensation mechanism becomes irrelevant and scoliosis tends to subside.
Keywords: Scoliosis treatment, Skeletal muscle hypertonicity, Contracture, Musculoskeletal disease, Spinal curvature
Introduction
Scolioses have been described for the first time by Galen in the second century AD, and it is interesting that this was done in his book "De moto musculorum."
Oddly however, the role of muscles is totally neglected in the etiology of scoliosis nowadays. Only a few researchers have considered the possibility of muscle involvement, but even then regarding it as a simple local reaction hypertonia to the curvature, without specifying the causes of scoliosis itself [1-5].
Thus scoliosis remains idiopathic, meaning that its cause is unknown, and obviously treatments can then only be symptomatic, with attempts to act on the consequence but not on the cause. For this reason, current treatments cannot be effective to correct scolioses or even to stop their progression seriously. Braces are considered to be efficient not if they straighten adolescent idiopathic scoliosis (AIS), but if they are able to only slow down its worsening by less than 5° to 10°. In fact, it is has not yet been established that evolution with braces is different from natural history [6,7]. 10% to 40% of patients with an angle of 20° to 30° wearing braces will undergo surgery, with high risks of complications and aftereffects [8].
Without treatment, the initial curvatures of less than 10 degrees rarely worsen (2%), and the curvatures of 10° to 20° will deteriorate in only 10% to 20% of cases. But those between 20° and 30° worsen in 70% to 80% of cases. Beyond 30%, there will be worsening in more than 90% of cases [9,10].
The patient's age and growth rate also affect prognosis: at Risser 0, the risk of progression of a scoliosis, even moderate, would be of 40% on average, 80% for a Cobb angle of 20°, and 100% for an angle of 30°.
Spontaneous improvement (straightening) is rare, and applies only to a few scolioses under 15°, in prepubertal period [9].
The fact is that there is a complete lack of progress in the area of AIS despite intensive research for more than 100 years. "If the current methods to study the aetiology of AIS continue to be applied, why should different results be expected when such intense, detailed research in the past has revealed so little?" [11].
Furthermore, according to the same author: "The goal for research into the etiology of AIS should be to find a cure (other than surgery) as soon as possible, preferably tomorrow-but, unfortunately, a cure remains a dream and does not even seem to be on the distant horizon".
We would like to show that the latter statement is no longer true, if we accept to change our way of thinking AIS.
Materials and Methods
Twenty general practitioners, 3 specialists in rehabilitation medicine, 1 pediatrician, and 14 physiotherapists have been treated in France, with Brachy-Myotherapy (BMT) only, 71 children and adolescents having scolioses with Cobb angles ranging between 11° and 62°.
BMT is a manual rehabilitation therapy. It aims to specifically treat lasting post-traumatic muscle spasms (contractures), which appear to be the basis of many joint diseases, whether acute or chronic. During treatment joints are placed in a position that allows maximum shortening of the dysfunctional muscles, according to a specific protocol, in order to put an end to the self-sustained reflex contraction. This method is purely passive, i.e., without participation of the patient; and since the therapist never uses force, the physiological amplitude of joints is never exceeded. BMT is a non-traumatic approach of musculoskeletal dysfunctions.
Muscle contractures (i.e., lasting spasms) are easy to diagnose, since they have specific symptoms: pain is triggered by palpation of the hypertonic muscles which are found hard, and tend to resist, sometimes painfully, to their passive stretching. Furthermore, they may distort the joints they govern, by pulling the bones in their direction.
Diagnosis also takes into account the spontaneous compensations of the body in relation to some contractures. Indeed, since a contracture distorts the position of a joint, it can cause chain reactions of hypertonic muscles, whether neighboring or remote, with the same consequences as for each contracture.
By treating the initial spasms, which are practically always located at the level of the neck, hypertonic compensations, now devoid of purpose, tend to disappear, along with their possible symptoms (pain, stiffness, and/or deformation).
Scoliosis seems to be a typical example of this process. This is why only the muscles of the neck were treated in this study; no other treatment whatsoever was performed at back or lumbar level.
1. Patients
There were 23 boys and 48 girls.
Only patients without braces have been included. The only therapy was therefore BMT, excluding any other approach, whether manual or other.
Inclusion criterion was idiopathic scoliosis of over 10°. Exclusion criteria were habit scolioses, scolioses of less than or equal to 10° (which are in fact often habit scolioses), non-idiopathic scoliosis (very rare in practice), and scoliosis with brace treatment.
-Six cases had an initial angle greater than or equal to 30° (expected worsening for nearly all cases).
-Nineteen cases had an initial angle between 20° and 29° (expected worsening in 75% of cases).
-The remaining 46 patients had an angle between 11 and 19° (worsening expected in only 15% of cases, but no spontaneous straightening expected either).
1) Age
2) Recruitment
This is an open multicenter survey, representative of what can be done in the general practitioner's or physiotherapist's practices. All patients included in this study were treated in town or country practices, never in a hospital. In general practice scoliosis patients are relatively rare, especially those over 20° without braces. For these reasons, each therapist could not produce results for many cases. On the other hand, the important number of therapists who participated in this study shows the reproducibility of the results.
A session of BMT was performed on average every 10 days. On average 14 sessions were performed (range, 2-48). BMT treatment has been continued, unless otherwise stated by the patient, either until the end of improvement (or the lack of it at the first control radiograph), or when Cobb angle had become of 10° or less. Treatments were generally quite short: 2 weeks to 16 months, on average 6 months. Patients were monitored by X-rays, one before the treatment and then every 3 to 6 months [13,14].
Results
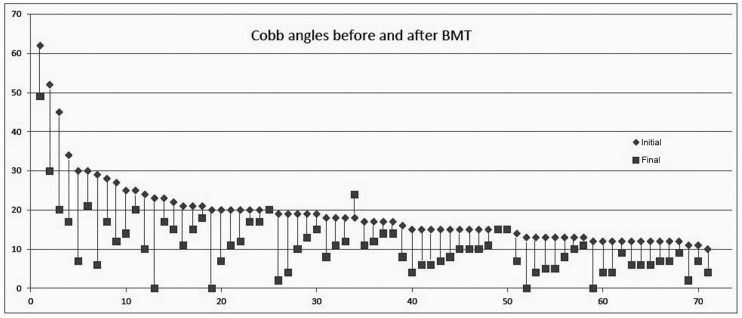
A straightening has been observed in 94% of cases, of an average 8° (maximum 25°) (Fig. 1).
Fig. 1.
Scoliosis angles before and after BMT (degrees). BMT, Brachy-Myotherapy.
Almost all radiologists provided only the Cobb angle of inclination, without mentioning the degrees of rotation, nor the angle of kyphosis or the Risser sign [15]. Therefore we could not include these data. However one should relativize these absences: several authors believe that the Risser sign is less accurate than the chronological age. Lonstein and Carlson [9] have shown that the average progression risk is nearly 70% at the age of 9, and diminishes steadily to 10% at the age of 15.
There is, of course, a 5° to 7° margin of error in Cobb angle measurements, but this can be neglected here, not only because of the average improvement of 8° and the 35 cases improved by more than 7° (half the patients of this study) but also because 10 patients (14%) improved of more than 14°, twice the most pessimistic margin of error. Furthermore, most patients had their radiographs before and after treatment commented by the same radiologist: even an error of 5 degrees is therefore highly improbable, not to mention one of 14°. Most of all, it should be kept in mind that all patients of this study were supposed to worsen, or at the best remain stable, none were expected to improve. However, nearly all of them did improve, whatever the initial Cobb angle was.
In other words, a spontaneous positive evolution of AIS is extremely rare, especially for the levels and ages that we have included in this study. Positive results are therefore sufficient enough to prove the effectiveness of the studied method, and also tend to prove the plausibility of the underlying etiological hypothesis.
Conventionally, prognosis depends on the initial Cobb angle. Therefore we will distinguish three groups in this study: initial scolioses over 30°, those between 20° and 29°, and those of 11° to 19°.
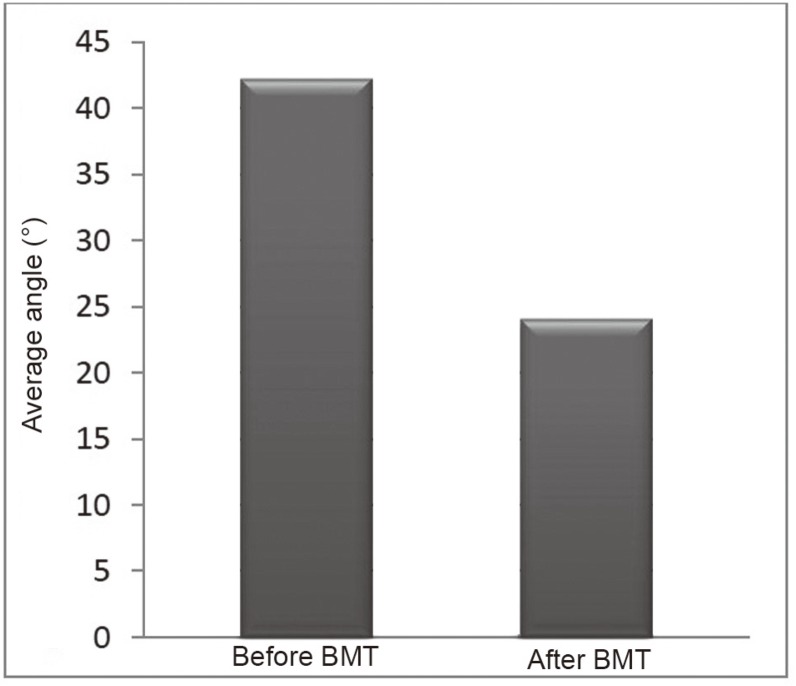
1) In the first group of 6 scolioses, initially of 30° or more (maximum 62°), traditionally having the worst prognosis (aggravation expected in nearly all cases), the average recovery was of 18° (43%), extremes 25° and 9° (Fig. 2). No worsening or even status quo was observed.
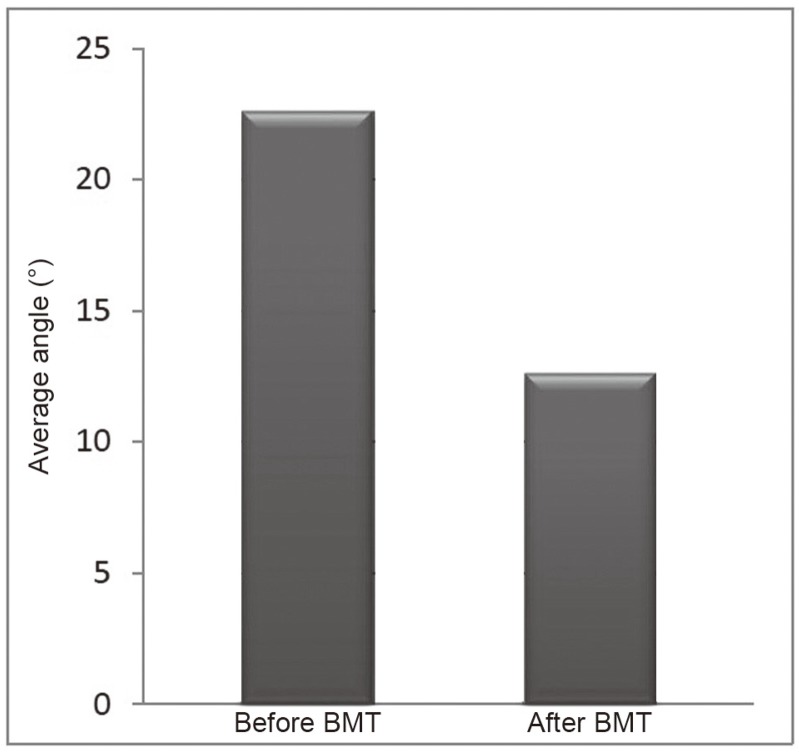
2) In the second group of 19 scolioses, initially of 20° to 29°, thus of traditionally of unfavorable prognosis (worsening expected in about 75% of cases), the average recovery was of 9° (44%), up to 23° (Fig. 3). No deterioration was observed, one single case simply remained stable (neither worsening nor improving, which in itself is already not so bad a result).
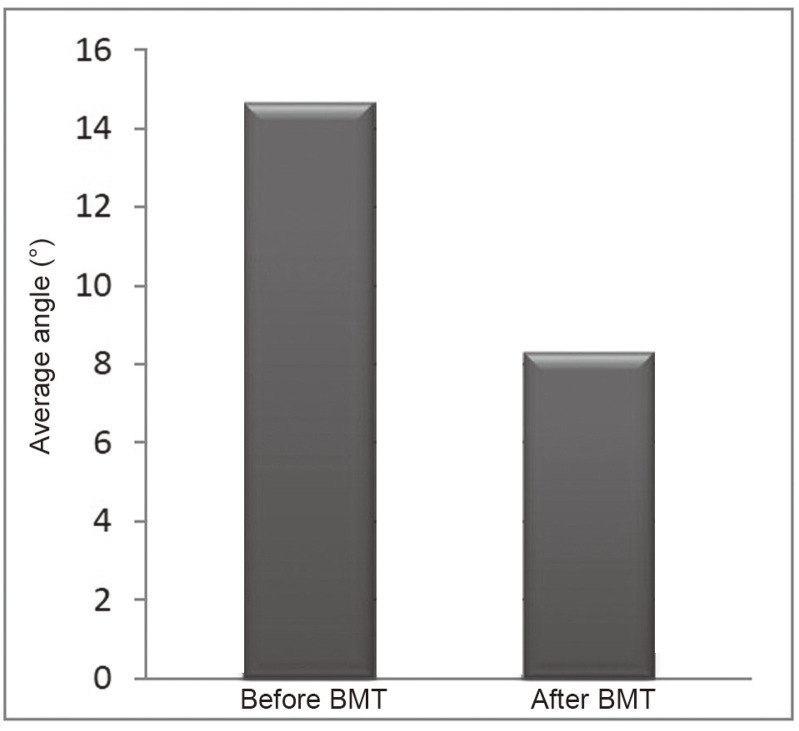
3) In the third group of 46 scolioses, initially between 11° and 19° (expected worsening in only 15% of cases, but no improvements expected), the average recovery was of 6° (maximum 17°) (Fig. 4). 37% of this group straightened by more than 7°. One aggravation (of 6°, in the range of what would have been a rather good result with a brace) was observed, and two cases remained stable.
Fig. 2.
Adolescent idiopathic scoliosis ≥30°: average angles before and after Brachy-Myotherapy treatment (BMT).
Fig. 3.
Adolescent idiopathic scoliosis 20° to 29°: average angles before and after Brachy-Myotherapy treatment (BMT).
Fig. 4.
Adolescent idiopathic scoliosis 11° to 19°: average angles before and after Brachy-Myotherapy treatment (BMT).
Among the total of 71 cases, there was thus only 1 aggravation, three nil effects (neither improving nor worsening), and 67 scolioses have straightened (94% of cases) with an average diminishment of the side-bending angle of 8°, up to 25°.
Thirty-nine patients out of 71 had less than 10° at the end of BMT treatment.
The more advanced the scoliosis was, that is to say the worst prognosis was, the more important the average gain was.
This was ascertained without any local treatment (dorsal and/or lumbar).
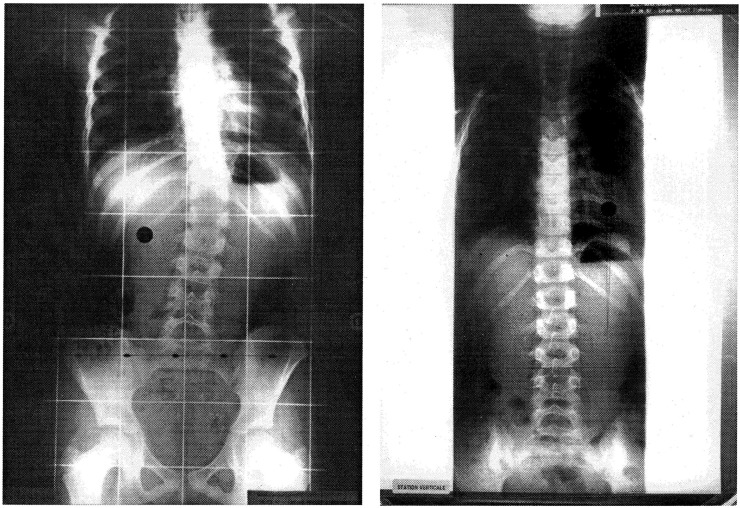
The radiographs of Fig. 5 show an example: a 6-year-old girl, Cobb angle of 19°, Risser 0 (very poor prognosis). Two months later, after 6 sessions of BMT: 2°. Straightening: 12°.
Fig. 5.
Six-year-old girl. March 19, 1997: 19° (Risser 0). Two months later (May 21, 1997): 2° (photo from A. Jamot).
It is worth recalling that the risk is greater for scolioses that begin before the age of 10. If we only keep the 5 cases in our study included in this age group (6-9 years, angles 18°-21°, average 19°), for which prognosis is typically very poor, we will find an average recovery of 13° (maximum 20°), thus well above the average of all ages in this study.
Altogether, the worse the initial conventional prognosis was, the better the results of the BMT treatment have been.
The aim of this study was to show what can be done with relatively short-time effects (usually less than a year); long-term effects will be the subject of another study. We can however mention that if BMT treatment is continued in a spaced manner until the end of growth, the results will be stable; improvements can increase with time for those that have not yet straightened to 10° or less during the first year (in this study more than 50% of patients had already achieved this).
It is also worth mentioning that patients with braces (for this reason not included in this study) do not respond to BMT treatments: worsening continues in all cases. Braces seem to be an obstacle to a disease-modifying therapy. Since we have shown that straightening is possible and easy with BMT, when it is known that this is not the case with brace treatments, it may be worthwhile changing our approach.
Discussion
1. Anatomy
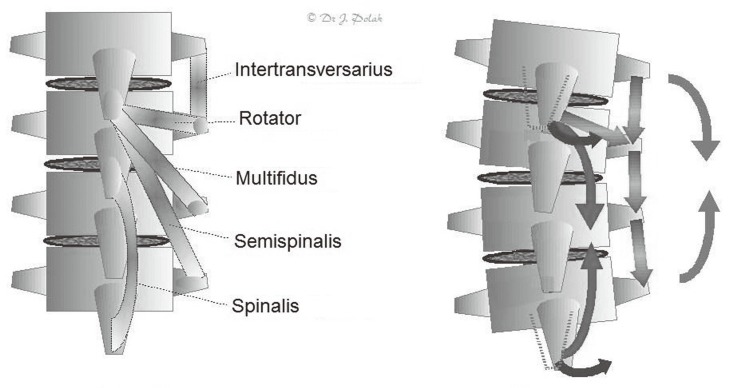
At the level of the thoracic vertebrae there are no anterior muscles. All muscles are on the back-side, commonly known as the transverso-spinal muscles. These are 5 kinds of short muscles, present on the whole spine at each vertebral level, linking spinous processes together, transverse processes together, and spinous processes to transverse processes of a lower level: the intertransversarius, rotator, multifidus, spinalis, and semispinalis muscles, all of them having only vertebral insertions. Their simultaneous one-sided contraction causes side bending, rotation of the spinous processes into the concavity, and extension of the thoracic spine: exactly the same deformation as scoliosis (Fig. 6).
Fig. 6.
The transversospinalis muscles and their one-sided contraction.
2. Etiological hypothesis
Since we were able to significantly straighten nearly 95% of AIS, some of them very advanced, without any local treatment, when scolioses seldom recover spontaneously, this means that their cause obviously is not located at the level of the back.
Postural imbalance disorders and proprioceptive dysfunctions have been noticed in several studies on AIS, relating to disturbances of oculomotor and/or vestibular reflexes [16-20]. Over 80% of children with AIS have a disorder of proprioception. Over 60% have a balance disorder related to vestibular dysfunctions.
An asymmetric position of the skull on the spine is found in 60% of scolioses. This can only be due to a persistent muscle contracture, which can follow, often in a remote way, an excessive obstetric traction on the skull, or a fall or a blow on the head, etc.
The horizontality of ears is necessary for reflex equilibration. The conservation of this factor seems to be a priority for the body, at all costs, so to speak. Asymmetries of the tone of neck muscles and resulting defects of the head position may require the person to permanently bend his spine to try to restore the natural horizontality of the ears. In some way the scoliotic child gives priority to the labyrinth over the spine.
The compensation tension can occur at the same contralateral cervical level, or at an underlying one. At the thoracic level of the spine there are only the transversospinal muscles. The compensation distortion, if located at this level, will be carried out in the direction of the resultant force vector: lateral bending, ipsilateral rotation, and extension.
An opposite side bending may occur afterwards at the lumbar level (by the underlying contralateral Transversospinal muscles), in order for the skull to remain vertically above the pelvis and the feet, for the sake of stability.
The persistent dorsal muscle hypertonia [1-5] can act as a spinal bowstring during pubertal growth, which would explain the increases of angle commonly observed during growth spurts. And, if there is pain, these contractures are also the cause of it.
Conclusions
Common sense tells us that only a lasting muscle contraction can twist a spine. In the case of scoliosis we may assume that if there is a durable side-bending of the neck and the skull due to lasting post-traumatic cervical muscle contractures, spinal compensation curves try to restore the cranial vestibular landmarks necessary for equilibrium, i.e. the horizontality of the ears and the labyrinths. The triple deformity of scoliosis would be due to the torsional orientation of the effector muscles. By treating the muscle contractures of the neck, the dorsal compensations become unnecessary, and the thoracic spine tends to recover to its normal shape.
Based on this hypothesis, 71 patients with AIS ranging from 11° to 62° have been treated with a manual therapy called BMT; this was carried out only at the level of the neck, without any treatment at the level of the scoliosis itself. The average straightening was 8° (up to 25°).
It is thus reasonable to think that the origin of AIS lies at the level of the neck, that its mechanisms are purely muscular, and that a simple disease modifying treatment is possible.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Cassidy JD, Brandell BR, Nykoliation JW, Wedge J. The role of paraspinal muscles in the pathogenesis of idiopathic scoliosis: a preliminary EMG study. J Can Chiropr Assoc. 1987;31:179–184. [Google Scholar]
- 2.Fidler MW, Jowett RL. Muscle imbalance in the aetiology of scoliosis. J Bone Joint Surg Br. 1976;58:200–201. doi: 10.1302/0301-620X.58B2.932082. [DOI] [PubMed] [Google Scholar]
- 3.Veldhuizen AG, Wever DJ, Webb PJ. The aetiology of idiopathic scoliosis: biomechanical and neuromuscular factors. Eur Spine J. 2000;9:178–184. doi: 10.1007/s005860000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zetterberg C, Bjork R, Ortengren R, Andersson GB. Electromyography of the paravertebral muscles in idiopathic scoliosis. Measurements of amplitude and spectral changes under load. Acta Orthop Scand. 1984;55:304–309. doi: 10.3109/17453678408992362. [DOI] [PubMed] [Google Scholar]
- 5.Zuk T. The role of spinal and abdominal muscles in the pathogenesis of scoliosis. J Bone Joint Surg Br. 1962;44:102–105. [Google Scholar]
- 6.Asher MA, Burton DC. Adolescent idiopathic scoliosis: natural history and long term treatment effects. Scoliosis. 2006;1:2. doi: 10.1186/1748-7161-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lenssinck ML, Frijlink AC, Berger MY, Bierman-Zeinstra SM, Verkerk K, Verhagen AP. Effect of bracing and other conservative interventions in the treatment of idiopathic scoliosis in adolescents: a systematic review of clinical trials. Phys Ther. 2005;85:1329–1339. [PubMed] [Google Scholar]
- 8.Weiss HR, Bess S, Wong MS, Patel V, Goodall D, Burger E. Adolescent idiopathic scoliosis-to operate or not? A debate article. Patient Saf Surg. 2008;2:25. doi: 10.1186/1754-9493-2-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am. 1984;66:1061–1071. [PubMed] [Google Scholar]
- 10.Rowe DE, Bernstein SM, Riddick MF, Adler F, Emans JB, Gardner-Bonneau D. A meta-analysis of the efficacy of non-operative treatments for idiopathic scoliosis. J Bone Joint Surg Am. 1997;79:664–674. doi: 10.2106/00004623-199705000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Bagnall KM. Using a synthesis of the research literature related to the aetiology of adolescent idiopathic scoliosis to provide ideas on future directions for success. Scoliosis. 2008;3:5. doi: 10.1186/1748-7161-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duval-Beaupère G, Lamireau T. Scoliosis at less than 30 degrees. Properties of the evolutivity (risk of progression) Spine (Phila Pa 1976) 1985;10:421–424. [PubMed] [Google Scholar]
- 13.Diard F, Chateil JF, Hauger O, Moinard M, Ducou-Lepointe H. Imagerie des scolioses de l'enfant et de l'adolescent. J Radiol. 2002;83:1117–1139. [PubMed] [Google Scholar]
- 14.Malfair D, Flemming AK, Dvorak MF, et al. Radiographic evaluation of scoliosis: review. AJR Am J Roentgenol. 2010;194:S8–S22. doi: 10.2214/AJR.07.7145. [DOI] [PubMed] [Google Scholar]
- 15.Risser JC. The Iliac apophysis; an invaluable sign in the management of scoliosis. Clin Orthop. 1958;11:111–119. [PubMed] [Google Scholar]
- 16.Beaulieu M, Toulotte C, Gatto L, et al. Postural imbalance in non-treated adolescent idiopathic scoliosis at different periods of progression. Eur Spine J. 2009;18:38–44. doi: 10.1007/s00586-008-0831-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lamantia M, Deutchman G, Indelacato J, Raykhman M. A retrospective study of thirty-six cases of vestibular hypofunction in adolescents with idiopathic scoliosis. Scoliosis. 2007;2:S37. [Google Scholar]
- 18.Lambert FM, Malinvaud D, Glaunes J, Bergot C, Straka H, Vidal PP. Vestibular asymmetry as the cause of idiopathic scoliosis: a possible answer from Xenopus. J Neurosci. 2009;29:12477–12483. doi: 10.1523/JNEUROSCI.2583-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manzoni D, Miele F. Vestibular mechanisms involved in idiopathic scoliosis. Arch Ital Biol. 2002;140:67–80. [PubMed] [Google Scholar]
- 20.Simoneau M, Lamothe V, Hutin E, Mercier P, Teasdale N, Blouin J. Evidence for cognitive vestibular integration impairment in idiopathic scoliosis patients. BMC Neurosci. 2009;10:102. doi: 10.1186/1471-2202-10-102. [DOI] [PMC free article] [PubMed] [Google Scholar]