Abstract
Despite major advances in medicine and public health during the past few decades, disparities in health and health care persist. Racial/ethnic minority groups in the United States are at disproportionate risk of being uninsured, lacking access to care, and experiencing worse health outcomes from preventable and treatable conditions. As reducing these disparities has become a national priority, insight into the social determinants of health has become increasingly important. This article offers a rationale for increasing the diversity and cultural competency of the health and health-care workforce, and describes key strategies led by the U.S. Department of Health and Human Services' Office of Minority Health to promote cultural competency in the health-care system and strengthen community-level approaches to improving health and health care for all.
The U.S. population faces many health challenges, including rising health-care costs, the need for a strong public health workforce, and persistent disparities among racial/ethnic minority groups and underserved populations. Despite major medical advances, critical threats to U.S. public health remain. In particular, the looming workforce shortages in medicine, nursing, laboratory sciences, and environmental health present serious threats to protecting the health of individuals, families, and communities, especially those who are most vulnerable and least able to help themselves.1 Compounding this issue, national data indicate that, compared with the general population, racial/ethnic minority populations have poorer health outcomes from preventable and treatable diseases, such as cardiovascular disease, cancer, asthma, and human immunodeficiency virus/acquired immunodeficiency syndrome than those in the majority.2,3 Additionally, there is a growing body of evidence documenting the differences in access to health care, the quality of care, and health measures, including life expectancy and infant mortality, among these groups.4–6 Public health experts ascertain that the social environment in which people live, learn, work, and play contributes to disparities and is among the most important determinants of health throughout the course of life.7
Increasingly, the idea that health is determined by factors outside the traditional health-care setting has become a recognized approach to improving public health and addressing health disparities.8 The social determinants of health (SDH)—including such factors as housing quality, access to healthy foods, and education—emphasize the importance of considering nonclinical conditions when providing quality care within the health-care system.9 Racial/ethnic minoritiy groups experience adverse SDH and are also disproportionately represented among the uninsured. The Institute of Medicine report “Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care” showed that racial/ethnic disparities in health care do exist.10 Key recommendations from this landmark study described the need to increase the proportion of underrepresented minority groups in the health-care workforce, integrate cross-cultural education into health-care training, and advance research efforts to identify sources of disparities and promising interventions.
Reflecting the national recognition and importance of workforce diversity and SDH in the reduction of racial/ethnic disparities, the U.S. Department of Health and Human Services (HHS) launched the HHS Action Plan to Reduce Racial and Ethnic Health Disparities (hereafter, HHS Disparities Action Plan),11 the most comprehensive federal commitment to date to reduce health disparities, which builds on the foundation of the Patient Protection and Affordable Care Act.12 The HHS Disparities Action Plan advances five major goals: (1) transforming health care; (2) strengthening the infrastructure and workforce of the nation's health and human services; (3) advancing the health, safety, and well-being of the American people; (4) advancing scientific knowledge and innovation; and (5) increasing the efficiency, transparency, and accountability of HHS programs.
Strengthening the nation's health by improving the diversity of the health and human services workforce calls for a multipronged approach that adopts an understanding of SDH, applies community-level engagement as a core principle, and emphasizes cultural and linguistic competency in health and health care. Considering this approach, this article highlights two of several HHS Office of Minority Health strategies that align with the HHS Disparities Action Plan, bridging workforce diversity and SDH to address disparity reduction efforts: (1) prioritizing cultural competence of health-care providers and systems to better serve patients with diverse cultural, social, and linguistic backgrounds; and (2) supporting initiatives that increase diversity within the workforce and promote community-based models to improve access to and quality of health care for all.
PROMOTING CULTURAL COMPETENCY TRAINING: A SAMPLE CASE
As the U.S. population becomes more diverse, pursuing the goal of cultural competence in the workforce and health-care system emerges as a leading strategy in reducing disparities.13 Cultural competency, defined as the ability of health-care providers to function effectively in the context of cultural differences, has been shown to improve the quality of health care received by racial/ethnic minority groups.14 For example, a culturally competent approach establishes ways to address communication barriers with people of limited English proficiency or low health literacy. Racial/ethnic diversity in the health-care workforce, a type of organizational cultural competence,15 has also been well correlated with the delivery of quality care to minority populations. Increasing underrepresented groups within the health-care workforce supports the diversity of values and beliefs of the entire population and heightens cultural awareness in health-care service delivery.
Strengthening the nation's workforce by improving cultural competency and increasing diversity is an important part of the HHS Disparities Action Plan. Education, training, and development of the workforce—including both professionals and lay community health workers—are essential in meeting the health and service needs of communities of color. U.S. government agencies, academic institutions, and private organizations provide the educational resources and disseminate information to enable health-care providers to acquire and apply cultural competency skills for the benefit of the patients and communities they serve.
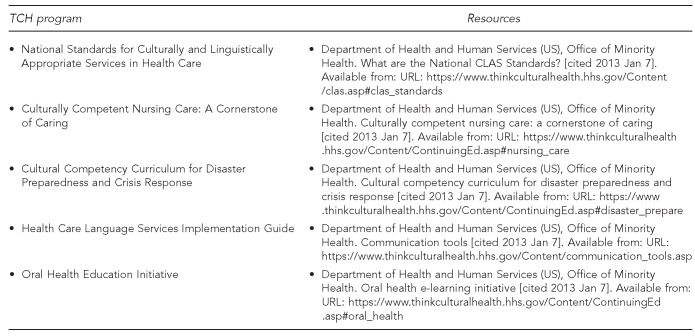
In addition, the HHS Office of Minority Health developed Think Cultural Health,16 a resource center that offers users the ability to earn continuing education credits in cultural competency through online training. Think Cultural Health was designed as a resource to improve quality of care through cultural and linguistic competencies and provides continuing education programs accredited for a variety of health-care providers (Figure). Model programs included on the Think Cultural Health website provide education and training, using case studies, pre- and posttests, and self-assessment exercises. The programs embed the principles outlined in the National Standards for Culturally and Linguistically Appropriate Services in Health Care (hereafter, CLAS Standards).17
Figure.
Think Cultural Health programs and resources: U.S. Department of Health and Human Services, Office of Minority Health
TCH = Think Cultural Health
For example, Culturally Competent Nursing Modules (CCNM) is one of the model programs that health-care providers, such as nurses and social workers, are using through Think Cultural Health (Table). The CCNM training curricula enables providers to improve self-awareness and adopt best practices when navigating the cultural attitudes, beliefs, and behaviors that influence the care and services they deliver. Through case studies that highlight potential cross-cultural scenarios in their day-to-day practices, the program emphasizes cultural and linguistic competency at every point of contact. Using the CLAS Standards as a framework, the modules also offer an overview of guidelines for providing language-access services in health-care settings and promoting strategies for integrating cultural competence into health-care organizations. This resource is one example of emerging tools available to help the health-care workforce develop the skills and knowledge necessary for providing services to an increasingly diverse nation.
Table.
Number of registrants in the Culturally Competent Nursing Care: A Cornerstone of Caring program, by certificate type: U.S. Department of Health and Human Services, Office of Minority Health, Think Cultural Health
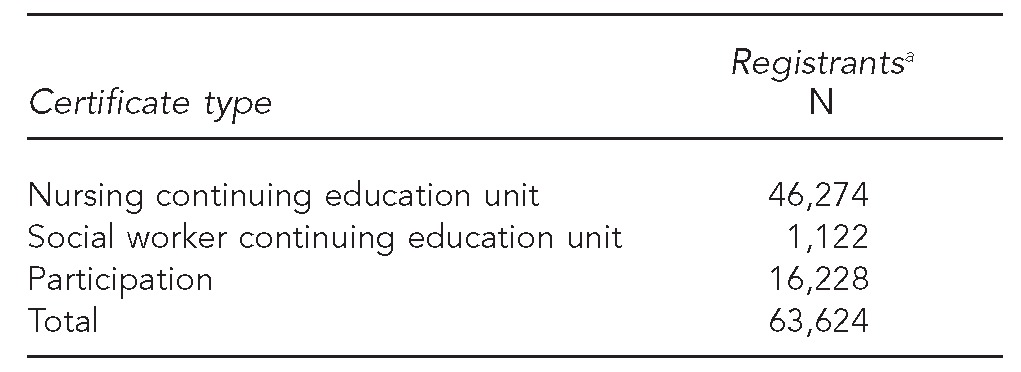
aNumber of registrants as of January 7, 2013
HHS PROMOTORES DE SALUD INITIATIVE: A COMMUNITY HEALTH WORKFORCE MODEL
A growing number of evidence-based initiatives apply community-level approaches to improve health and health care and reduce health disparities. The Promotores de Salud initiative, led by the HHS Office of Minority Health, promotes the increased engagement of promotores de salud (also known as community health workers) in health education, outreach, and access to health care for racial/ethnic populations and their communities.18 These promotores de salud are defined as “volunteer community members and paid frontline public health workers who are trusted members of and/or have an unusually close understanding of the community served.” Community health workers are identified as trusted community members who can provide the needed support to address SDH at the community level. Evidence of the promotores model has shown improvement in health-care access and outcomes and enhancement in quality of life for people in poor, underserved, and minority communities.19–21 Bringing together multiple partners, including federal, community, and advocacy organizations, the initiative is poised to expand the use of promotores and community health workers as an integral part of the workforce to promote health education, prevention, and other targeted efforts for populations experiencing health disparities. The initiative includes a National Promotores de Salud Steering Committee and supporting and linking promotores networks across the nation. The HHS Promotores de Salud initiative recognizes the role promotores and community health workers play in identifying and developing solutions to the health challenges faced by minority communities.
CONCLUSION
The unprecedented strain on health-care resources demands a coordinated national response to improving the health of all Americans. Progress toward reducing health disparities will involve support for community-based strategies, enhanced the understanding of SDH, and increased diversity of the health-care workforce. Examples of this recognition on the national level are evident with initiatives such as Healthy People 2020,9 the National Prevention Strategy,22 and the National Partnership for Action to End Health Disparities.23 The coordinated efforts to address disparities take into account strategies and actions that build on community infrastructure and an increasingly diverse and culturally competent workforce. It is with these types of investments that our nation will achieve the vision of “a nation free of health and health-care disparities.”11
Footnotes
The authors thank Julia Lam of the U.S. Department of Health and Human Services (HHS), Office of Minority Health, for her review and insightful comments on drafts of this manuscript.
The views expressed in this article are those of the authors and do not necessarily represent those of HHS.
REFERENCES
- 1.Institute of Medicine, Committee on Assuring the Health of the Public in the 21st Century. The future of the public's health in the 21st century. Washington: National Academies Press; 2002. [Google Scholar]
- 2.CDC health disparities and inequalities report—United States, 2011. MMWR Surveill Summ. 2011;(60 Suppl):1–114. [PubMed] [Google Scholar]
- 3.Mead H, Cartwright-Smith L, Jones K, Ramos C, Woods K, Siegel B. Racial and ethnic disparities in U.S. health care: a chartbook. New York: The Commonwealth Fund; 2008. [Google Scholar]
- 4.Department of Health and Human Services (US), Agency for Healthcare Research and Quality. National healthcare disparities report, 2011. Rockville (MD): AHRQ; 2012. [Google Scholar]
- 5.Cooper LA, Hill MN, Powe NR. Designing and evaluating interventions to eliminate racial and ethnic disparities in health care. J Gen Intern Med. 2002;17:477–86. doi: 10.1046/j.1525-1497.2002.10633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chin MH, Walters AE, Cook SC, Huang ES. Interventions to reduce racial and ethnic disparities in health care. Med Care Res Rev. 2007;64(5 Suppl):7S–28S. doi: 10.1177/1077558707305413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Satcher D. Eliminating racial and ethnic disparities in health: the role of the ten leading health indicators. J Natl Med Assoc. 2000;92:315–8. [PMC free article] [PubMed] [Google Scholar]
- 8.Williams DR, Costa MV, Odunlami AO, Mohammed SA. Moving upstream: how interventions that address the social determinants of health can improve health and reduce disparities. J Public Health Manag Pract. 2008;(14 Suppl):S8–17. doi: 10.1097/01.PHH.0000338382.36695.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Department of Health and Human Services (US) Healthy people 2020. 2020 topics and objectives: social determinants of health [cited 2013 Jan 11] Available from: URL: http://www.healthypeople.gov/2020/default.aspx.
- 10.Smedley BD, Stith AY, Nelson AR, editors. Institute of Medicine, Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Board on Health Sciences Policy. Unequal treatment: confronting racial and ethnic disparities in health care. Washington: National Academies Press; 2003. [PubMed] [Google Scholar]
- 11.Department of Health and Human Services (US) HHS action plan to reduce racial and ethnic disparities: a nation free of disparities in health and health care. Washington: HHS; 2011. [Google Scholar]
- 12. Pub. L. No. 111-148, 124 Stat. 119 (March 23, 2010) [Google Scholar]
- 13.Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong O., 2nd Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003;118:293–302. doi: 10.1016/S0033-3549(04)50253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Institute of Medicine, Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington: National Academies Press; 2001. [Google Scholar]
- 15.Betancourt JR. Improving quality and achieving equity: the role of cultural competence in reducing racial and ethnic health disparities in health care. New York: The Commonwealth Fund; 2006. [Google Scholar]
- 16.Department of Health and Human Services (US), Office of Minority Health. About Think Cultural Health (TCH) [cited 2013 Jan 4] Available from: URL: https://www.thinkculturalhealth.hhs.gov.
- 17.Department of Health and Human Services (US), Office of Minority Health. National standards for culturally and linguistically appropriate services in health care. Washington: HHS; 2001. [Google Scholar]
- 18.Department of Health and Human Services (US), Office of Minority Health. HHS promotores de salud initiative [cited 2012 Dec 21] Available from: URL: http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlid=207.
- 19.Department of Health and Human Services (US), Health Resources and Services Administration, Bureau of Health Professions. Community health workers national workforce study. Rockville (MD): HRSA; 2007. [Google Scholar]
- 20.Swider SM. Outcome effectiveness of community health workers: an integrative literature review. Public Health Nurs. 2002;19:11–20. doi: 10.1046/j.1525-1446.2002.19003.x. [DOI] [PubMed] [Google Scholar]
- 21.Rosenthal EL, Brownstein JN, Rush CH, Hirsch GR, Willaert AM, Scott JR, et al. Community health workers: part of the solution. Health Aff (Millwood) 2010;29:1338–42. doi: 10.1377/hlthaff.2010.0081. [DOI] [PubMed] [Google Scholar]
- 22.National Prevention Council (US) National prevention strategy: America's plan for better health and wellness. Washington: Department of Health and Human Services (US), Office of the Surgeon General; 2011. [Google Scholar]
- 23.National Partnership for Action to End Health Disparities. National stakeholder strategy for achieving health equity. Rockville (MD): Department of Health and Human Services (US), Office of Minority Health; 2011. [Google Scholar]