Abstract
Leiomyosarcoma is a malignant mesenchymal neoplasm deriving from the smooth muscle cells. Primary hepatic leiomyosarcoma is very rare. Its onset is always during middle and old age. Herein, we present a case of primary hepatic leiomyosarcoma in a 5-month-old girl who may be the youngest patient reported in the known published English literature.
Keywords: Infant, liver, primary, neoplasm, leiomyosarcoma
Introduction
Leiomyosarcoma is rare in the liver. Metastatic hepatic leiomyosarcoma is more common than primary lesions and usually spread from the gastrointestinal tract, genitourinary apparatus, and retroperitoneum (1). Primary hepatic leiomyosarcoma may derive from smooth muscle cells of the intrahepatic vascular structures, bile ducts or ligamentum teres (1,2). Patients commonly have non-specific clinical symptoms such as pain, anorexia, and vomiting. Primary hepatic leiomyosarcoma is extremely infrequent in the pediatric population. Early diagnosis is challenging for clinical practitioners and radiologists. Imaging studies offer earlier detection, tumor localization and characterization as well as extent for making appropriate treatment strategies.
Case report
A 5-month-old girl with an uneventful birth history was brought to our pediatric hospital for fever, nausea, vomiting, and a poor appetite.
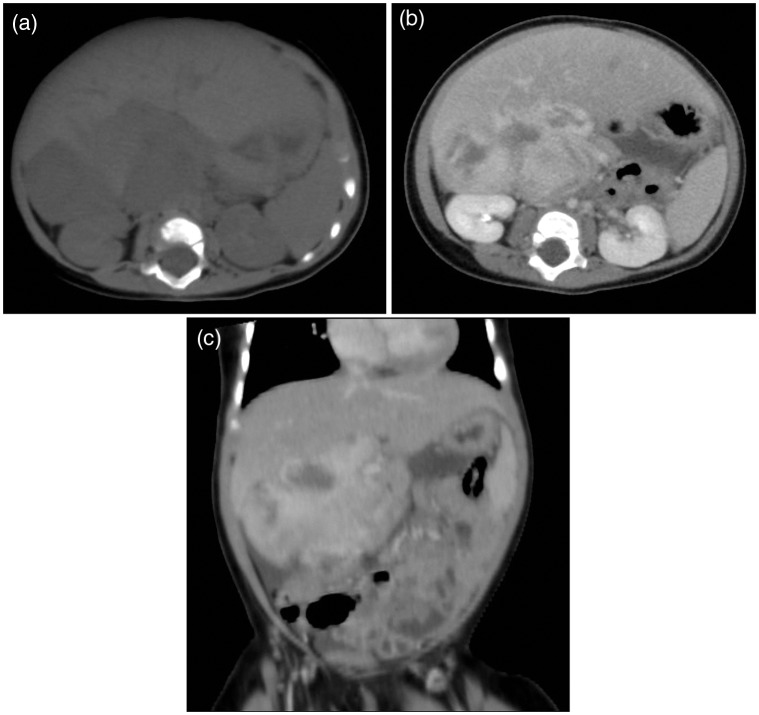
During hospitalization, hepatomegaly was found by a physical examination. The biochemical data were within normal limits. An abdominal radiograph displayed increased opacity at the right upper quadrant, raising concern of hepatomegaly (Fig. 1). Abdominal ultrasonography demonstrated a huge heteroechogenic mass abutting the inferior aspect of the liver. Computed tomography (CT) scan of the liver disclosed a large soft tissue mass measuring about 4.4 × 5.0 × 6.5 cm in size arising from the inferior aspect of the right lobe. On unenhanced images (Fig. 2a), the tumor appeared with heterogeneous hypodensity without notable calcifications. The mass enhanced heterogeneously and intensely after contrast medium injection (Ultravist ®; Bayer Schering Pharma AG, Berlin, Germany; 300 mgI/mL, injection volume 30 mL at a rate of 1.5 mL/s) with areas of low attenuation, suggesting necrosis or hemorrhage (Fig. 2b and c). The tumor margin was partially demarcated with mass effect to the inferior vena cava but no overt regional lymphadenopathy was found. Further imaging studies including brain and chest CT scans, as well as nuclear medicine whole-body bone scan showed no evidence of remote metastasis. Serologic investigations including hepatitis B surface antigen, antibody of hepatitis C virus, alpha-fetoprotein, and beta-human chorionic gonadotropin were all negative.
Fig. 1.

Plain abdominal film revealed increased opacity over the right upper abdomen, raising concern of hepatomegaly.
Fig. 2.
CT features of primary hepatic leiomyosarcoma. (a) Unenhanced axial CT scan of the liver revealed a large, partial demarcated and heterogeneous low attenuation mass arising from the inferior part of the right lobe of the liver without notable calcification seen. (b) Contrast-enhanced axial and (c) coronal CT scan in the venous phase showed the mass enhancing heterogeneously and intensely with areas of necrosis or hemorrhage and having mass effect to adjacent right kidney and bowel loops.
Biopsy was performed and the pathological examination uncovered a spindle cell type rhabdomyosarcoma. She was then treated with chemotherapy for 4 months but no tumor size regression was seen. Exploratory laparotomy with partial hepatectomy was then performed and disclosed a large tumor mass arising from segment VI of the liver. Histopathology confirmed the diagnosis of hepatic leiomyosarcoma. After operation, adjuvant chemotherapy was given for 6 months and the patient has now been free from tumor for 4 years.
Discussion
In previous reports, primary hepatic leiomyosarcoma is rare and usually derives from the alimentary tract, uterus, retroperitoneum, and lungs (1). The possibility of metastatic hepatic leiomyosarcoma should be excluded before making the diagnosis of a primary lesion. Primary hepatic leiomyosarcoma may originate from the smooth muscles of the intrahepatic vessels or biliary structures or ligamentum teres (1,2).
The mean age of diagnosis is 58 years (3) while pediatric cases are very rare and <1% has been documented in published English literature. Hepatic leiomyosarcoma has been described to occur in children afflicted with acquired immunodeficiency syndrome (4), Epstein-Barr virus infection (5), and other forms of immunosuppression (1). Surendrababu et al. have reported about a 1-year-old boy with primary hepatic leiomyosarcoma without any pre-existing disease (6). Our little girl was also quite healthy before the outbreak of symptoms without any predisposing pathologies of immunodeficiency.
Owing to vague clinical symptoms, such as abdominal pain, anorexia, body weight loss, and a lack of specific serologic markers, histological confirmation is necessary to make the diagnosis of primary hepatic leiomyosarcoma. The major clinical signs of primary hepatic leiomyosarcoma include tenderness over the upper abdomen, right upper abdominal mass, and hepatomegaly. Most patients do not have liver cirrhosis or other hepatic disorders (7). Liver function tests and alpha-fetoprotein values are often within normal limits (1). The majority of the cases described have originated from the right liver lobe (8) and our patient’s mass was also situated in the same location.
Imaging findings are non-characteristic. Two kinds of appearance have been illustrated on CT scans: a cystic mass with an enhancing wall imitating hydatid cyst or abscess (1) or a large, demarcated, heterogeneous hypodense mass with peripheral and internal enhancement as well as liquescent necrosis (1,7). Magnetic resonance imaging (MRI) may demonstrate hypointensity on T1-weighted images and heterogeneous hyperintensity on T2-weighted images with sometimes encapsulation (7). Our patient’s tumor showed a large, well-circumscribed solid mass with intense and heterogeneous enhancement that was partly necrotic but no obvious capsule was seen. Based upon imaging features and age, initial differential diagnosis included hepatoblastoma, rhabdomyosarcoma, abscess, and metastasis from neuroblastoma. However, further studies could not reveal any sign of a primary tumor.
Microscopic features of primary hepatic leiomyosarcoma include spindle-shaped cells with intersecting bundles. Immunochemistry is positive for desmin, vimentin, and smooth muscle actin but negative for keratin and S-100 protein (3).
Standard therapeutic strategy for this tumor has not been well established due to its rareness. Nevertheless, experimental cancer treatment including surgical resection combined with chemotherapy and radiotherapy (1) is generally being followed.
In conclusion, when a large, demarcated, and heterogeneous hypervascular hepatic mass with liquescent necrosis or hemorrhage is found even in an infant, malignancy should be highly suspected. We must keep in mind the tentative differential diagnosis of primary hepatic leiomyosarcoma despite of its rarity. Estimating imaging characteristics and tumor extent in detail will be beneficial for making a proper evaluation and management.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1. Shivathirthan N, Kita J, Iso Y, et al. Primary hepatic leiomyosarcoma: case report and literature review. World J Gastrointest Oncol 2011; 3: 148–152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yamaguchi J, Azuma T, Fujioka H, et al. Leiomyosarcoma occurring in the ligamentum teres of the liver: a case report and a review of seven reported cases. Hepatogastroenterology 1996; 43: 1051–1056 [PubMed] [Google Scholar]
- 3. Shamseddine A, Faraj W, Mukherji D, et al. Unusually young age distribution of primary hepatic leiomyosarcoma: case series and review of the adult literature. World J Surg Oncol 2010; 8: 56–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Levin TL, Adam HM, van Hoeven KH, et al. Hepatic spindle cell tumors in HIV-positive children. Pediatr Radiol 1994; 24: 78–79 [DOI] [PubMed] [Google Scholar]
- 5. Brichard B, Smets F, Sokal E, et al. Unusual evolution of an Epstein-Barr virus-associated leiomyosarcoma occurring after liver transplantation. Pediatr Transplant 2001; 5: 365–369 [DOI] [PubMed] [Google Scholar]
- 6. Surendrababu NR, Rao A, Samuel R. Primary hepatic leiomyosarcoma in an infant. Pediatr Radiol 2006; 36: 366–366 [DOI] [PubMed] [Google Scholar]
- 7. Yu RS, Chen Y, Jiang B, et al. Primary hepatic sarcomas: CT findings. Eur Radiol 2008; 18: 2196–2205 [DOI] [PubMed] [Google Scholar]
- 8. Ferrozzi F, Bova D, Zangrandi A, et al. Primary liver leiomyosarcoma: CT appearance. Abdom Imaging 1996; 21: 157–160 [DOI] [PubMed] [Google Scholar]