Abstract
We report an extremely rare case of wandering spleen (WS) complicated with gastric volvulus and intestinal non-rotation in a male adult. A 22-year-old man who had been previously treated for Wilson disease was admitted with severe abdominal pain. Radiological findings showed WS in the midline of the pelvic area. The stomach was mesenteroaxially twisted and intestinal non-rotation was observed. Radiology results did not show any evidence of splenic or gastrointestinal (GI) infarction. Elective emergency laparoscopy confirmed WS and intestinal non-rotation; however, gastric volvulus was not observed. It was suspected that the stomach had untwisted when gastric and laparoscopic tubes were inserted. Surgery is strongly recommended for WS because of the high risk of serious complications; however, some asymptomatic adult patients are still treated conservatively, such as the patient in this study. The present case is reported with reference to the literature.
Keywords: Abdomen/GI, CT, mesentery, adults and pediatrics, congenital, connective tissue disorders
Introduction
Wandering spleen (WS) is an uncommon disease characterized by excessive mobility and displacement of the spleen from its normal position. Gastric volvulus is defined as gastric torsion of >180° along either the organoaxial (long) or mesenteroaxial (short) axis. Intestinal non-rotation is a subtype of malrotation, which is a congenital abnormal positioning of the bowel. WS mainly affects children and women of reproductive age; however, occurrence in men is rare. Surgery is strongly recommended for WS because of the high risk of serious complications if left untreated (1). Complication with gastric volvulus is occasionally reported (2 –6), and WS with malrotation is extremely rare.
Case report
The patient was a 22-year-old man who had undergone treatment for neurological-type Wilson disease at the age of 13 years. The disease was well controlled with medication. The patient was admitted for sudden abdominal pain; however, he claimed that he had been experiencing abdominal pain since childhood. On examination, the abdomen was tender; however, no mass was detected. Laboratory data were non-specific.
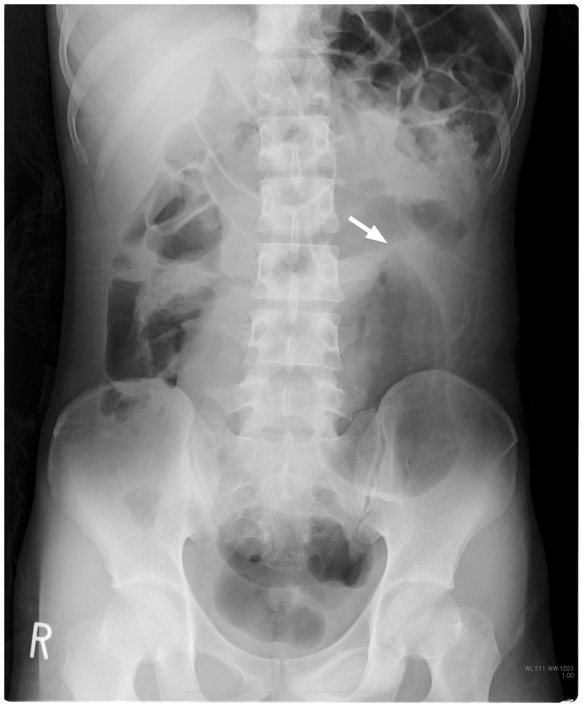
Plain abdominal radiography revealed an enlarged stomach in the left lower abdomen (Fig. 1). Computed tomography (CT) demonstrated a normal-sized spleen in the midline of the pelvic region (Fig. 2). The ascending colon had shifted under the left diaphragm, and the small intestine was in the right lower abdominal cavity. The stomach was below the colon and had twisted mesenteroaxially. The distal inferior vena cava and superior mesenteric vein ran to the left of the aorta and superior mesenteric artery, respectively (Fig. 2).
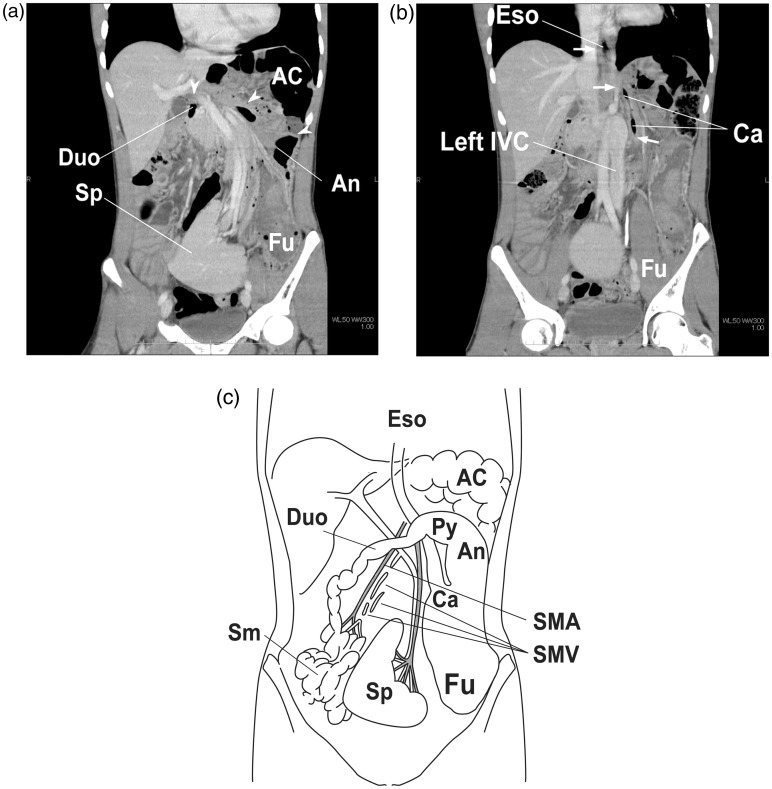
Fig. 1.
Plain abdominal radiography. A pre-laparoscopic image. An enlarged stomach is observed in the left lower abdomen. The upper third of the stomach appears beak shaped in a superior direction (short white arrow).
Fig. 2.
Coronal view of a contrast-enhanced computed tomographic image of the abdomen. (a) The spleen (Sp) is positioned in the midline of the pelvic area. The splenic parenchyma appears homogeneous. The ascending colon (AC) has shifted under the left diaphragm. The small intestine (Sm) appears in the right lower abdominal cavity. The stomach is twisted mesenteroaxially, with the antrum (An) positioned higher than the fundus (Fu). The white arrow heads show the connection from the shifted pylorus to the duodenum. (b) A slice obtained further posterior in the same series as (a). The white arrows show the connection from the shifted fundus of the stomach (Fu) to the cardia (Ca) and esophagus (Eso). The lower inferior vena cava (IVC) runs to the left of the aorta. (c) The schema of the wandering spleen, gastric volvulus, and intestinal malrotation in the presented case. AC, ascending colon; An, antrum of stomach; Ca, cardia; Duo, duodenum; Eso, esophagus; Fu, fundus of stomach; Py, pylorus; Sm, small intestine; Sp, spleen.
On the basis of these findings, WS with gastric volvulus and intestinal non-rotation was diagnosed. On contrast-enhanced CT, the splenic parenchyma was homogenous attenuation, suggesting the absence of splenic infarction. There was no evidence of ischemia or infarction of the gastrointestinal tract.
Abdominal pain reduced with the passage of a nasogastric tube. Elective emergency laparoscopy was then performed. WS and intestinal non-rotation were confirmed by laparoscopy. All supportive splenic ligaments were absent. The upper and lower colons were not fixed and shared the mesentery with the small intestine. The stomach was greatly enlarged; however, gastric volvulus was not observed. It was suspected that the stomach had untwisted when gastric and laparoscopic tubes were inserted. The laparoscopic wound was closed without surgical intervention. Requirement of further surgery was explained to the patient; however, the patient declined undergoing surgery because his symptoms improved after emergency laparoscopy. The patient has not experienced abdominal pain for 6 months.
Discussion
Although WS, gastric volvulus, and intestinal malrotation, including non-rotation, are uncommon and can occur independently, the three entities share a common congenital etiology: anomalous intraperitoneal visceral attachment originating from the dorsal mesentery. Both acquired and congenital mechanisms for WS are known. The former mainly occurs in multiparous women as a result of hormonal changes (7), whereas the latter is explained as the failure of fusion of the dorsal mesentery with the posterior body during fetal development (2). This failure leads to incomplete formation of splenic supporting ligaments. The same mechanism explains the etiology of gastric volvulus, which results in the absence of gastrophrenic and gastrosplenic ligaments. The dorsal mesentery is also a key toward initiation of embryological intestinal rotation (8). The problem of malrotation is seen not only in the malpositioning but also in malfixation of the bowel and mesentery (9), as seen in the present case.
The complication of WS and gastric volvulus is reported occasionally (2 –6,10 –18). Of the 32 cases recorded, 28 cases were in the pediatric population, three cases were unknown, and only one case was in an adult (17). Mesenteroaxial volvulus is more frequent than organoaxial volvulus (8 cases vs. 1 case), a ratio that is similar to that of the types of gastric volvulus in general. The complication of WS by non-rotation or any type of malrotation is reported relatively less frequently than that by gastric volvulus, of which there is only one case in the pediatric population (16). In that case, gastric volvulus was also present as seen in the present case. The complication of malrotation is less common because it probably involves a more primitive stage of dorsal mesenteric development.
Splenopexy is the most commonly recommended treatment for WS (5,6,11,19). Splenectomy should be avoided because of the risk of postsplenectomic sepsis and the physiological importance of the spleen, unless unavoidable because of complications. Gastropexy is usually the treatment of choice when gastric volvulus is present (11,14,20). In contrast, the treatment for malrotation in adults is still controversial when there is no herniation or if it is found incidentally on CT (21).
In the present case, conservative therapy was selected because of the absence of potentially fatal complications and the patient’s refusal for further surgery. To the best of our knowledge, there are no reports of long-term follow-up of non-surgical WS. However, conservative therapy may be inappropriate even for asymptomatic adult patients (19). Allen and Andrews reported that 66% of patients with acute WS demonstrated no symptoms prior to occurrence of life-threatening complications (22). Although our patient has experienced an uneventful recovery for 6 months since he was discharged, splenopexy should have been performed at the time of initial laparoscopy.
We investigated the possibility that Wilson disease, the patient’s initial condition, could be the secondary cause of WS or other abnormalities of intraperitoneal visceral attachments; however, no such relationship was found.
In conclusion, we report an extremely unusual case of WS complicated by gastric volvulus and intestinal nonrotation in an adult. These three entities share a common congenital abnormality originating from the development of the dorsal mesentery. Life-threatening complications in WS are unpredictable; therefore, the need for surgery should be highlighted.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1. Buehner M, Baker MS. The wandering spleen. Surg Gynecol Obstet 1992; 175: 373–387 [PubMed] [Google Scholar]
- 2. Okazaki T, Ohata R, Miyano G, et al. Laparoscopic splenopexy and gastropexy for wandering spleen associated with gastric volvulus. Pediatr Surg Int 2010; 26: 1053–1055 [DOI] [PubMed] [Google Scholar]
- 3. Liu HT, Lau KK. Wandering spleen: an unusual association with gastric volvulus. Am J Roentgenol 2007; 188: W328–W330 [DOI] [PubMed] [Google Scholar]
- 4. Pelizzo G, Lembo MA, Franchella A, et al. Gastric volvulus associated with congenital diaphragmatic hernia, wandering spleen, and intrathoracic left kidney: CT findings. Abdom Imaging 2001; 26: 306–308 [DOI] [PubMed] [Google Scholar]
- 5. Garcia JA, Garcia-Fernandez M, Romance A, et al. Wandering spleen and gastric volvulus. Pediatr Radiol 1994; 24: 535–536 [DOI] [PubMed] [Google Scholar]
- 6. Spector JM, Chappell J. Gastric volvulus associated with wandering spleen in a child. J Pediatr Surg 2000; 35: 641–642 [DOI] [PubMed] [Google Scholar]
- 7. Robinson AP. Wandering spleen: case report and review. Mt Sinai J Med 1988; 55: 428–434 [PubMed] [Google Scholar]
- 8. Martin V, Shaw-Smith C. Review of genetic factors in intestinal malrotation. Pediatr Surg Int 2010; 26: 769–781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Polavarapu HV, Fassler SA, Zebley MD. Intestinal nonrotation in an adult. Am Surg 2011; 77: E260–E261 [PubMed] [Google Scholar]
- 10. Honna T, Kamii Y, Tsuchida Y. Idiopathic gastric volvulus in infancy and childhood. J Pediatr Surg 1990; 25: 707–710 [DOI] [PubMed] [Google Scholar]
- 11. Uc A, Kao SC, Sanders KD, et al. Gastric volvulus and wandering spleen. Am J Gastroenterol 1998; 93: 1146–1148 [DOI] [PubMed] [Google Scholar]
- 12. Zivkovic SM. Sutureless “button and hole” splenopexy. Pediatr Surg Int 1998; 13: 220–222 [DOI] [PubMed] [Google Scholar]
- 13. Tashjian DB, Moriarty KP. Re: “Gastric volvulus associated with wandering spleen in a child”. J Pediatr Surg 2001; 36: 1468–1468 [DOI] [PubMed] [Google Scholar]
- 14. Qazi A, Awadalla S. Wandering spleen: a rare cause of mesenteroaxial gastric volvulus. Pediatr Surg Int 2004; 20: 878–880 [DOI] [PubMed] [Google Scholar]
- 15. Lin CH, Wu SF, Lin WC, et al. Wandering spleen with torsion and gastric volvulus. J Formos Med Assoc 2005; 104: 755–758 [PubMed] [Google Scholar]
- 16. Saxena AK, van Tuil C, Groszek-Terwei I, et al. Torsion of a wandering spleen with stomach volvulus and nonrotation: extraperitoneal pocket splenopexy. Surgery 2005; 137: 265–265 [DOI] [PubMed] [Google Scholar]
- 17. Matsushima K, Kayo M, Hachiman H, et al. Laparoscopic repair of gastric volvulus associated with wandering spleen in an adult: report of a case. Surg Today 2006; 36: 843–845 [DOI] [PubMed] [Google Scholar]
- 18. Francois-Fiquet C, Belouadah M, Chauvet P, et al. Laparoscopic gastropexy for the treatment of gastric volvulus associated with wandering spleen. J Laparoendosc Adv Surg Tech A 2009; 19(Suppl. 1): S137–S139 [DOI] [PubMed] [Google Scholar]
- 19. Soleimani M, Mehrabi A, Kashfi A, et al. Surgical treatment of patients with wandering spleen: report of six cases with a review of the literature. Surg Today 2007; 37: 261–269 [DOI] [PubMed] [Google Scholar]
- 20. Ghosh S, Palmer KR. Double percutaneous endoscopic gastrostomy fixation: an effective treatment for recurrent gastric volvulus. Am J Gastroenterol 1993; 88: 1271–1272 [PubMed] [Google Scholar]
- 21. Dilley AV, Pereira J, Shi EC, et al. The radiologist says malrotation: does the surgeon operate?. Pediatr Surg Int 2000; 16: 45–49 [DOI] [PubMed] [Google Scholar]
- 22. Allen KB, Andrews G. Pediatric wandering spleen–the case for splenopexy: review of 35 reported cases in the literature. J Pediatr Surg 1989; 24: 432–435 [DOI] [PubMed] [Google Scholar]