Summary
Ocular fundus examination is a fundamental component of the neurologic examination. Finding papilledema in headache patients or retinal arterial emboli in stroke patients can be extremely useful. Although examination of the ocular fundus with a direct ophthalmoscope is an important skill for all neurologists, it is rarely and unreliably performed. Nonmydriatic ocular fundus photography, which allows direct visualization of high-quality photographs of the ocular fundus, has been recently proposed for screening neurologic patients in urgent care settings such as emergency departments. This new technology has many potential applications in neurology, including e-transmission of images for remote interpretation.
Ocular fundus examination is a fundamental component of the physical examination and is particularly important in neurology. In acute settings, finding papilledema in headache patients or retinal arterial emboli in stroke patients will potentially change patient management.
Non-ophthalmologists usually use a direct ophthalmoscope to examine the ocular fundus. However, there is ample evidence in the literature that direct ophthalmoscopy is technically difficult and allows only a partial view of the ocular fundus, often resulting in misdiagnoses and explaining why very few practicing health care providers carry and use an ophthalmoscope nowadays.1 Advances in technology have allowed for the acquisition of high-quality digital photographs of the ocular fundus, even without pupillary dilation. Nonmydriatic fundus photographs have been recently proposed as a promising alternative to direct ophthalmoscopy for systematic screening of neurologic patients by non-ophthalmologists in the emergency department (ED).2 These digital nonmydriatic ocular fundus cameras have become more affordable, are easy to use, and are now found in various non-ophthalmology settings such as EDs and primary care or neurologists' offices. A better understanding of this new technology and its potential applications in neurology will help neurologists decide whether such cameras should become part of neurology offices or urgent care centers.
Applications of nonmydriatic photography in acute neurologic settings
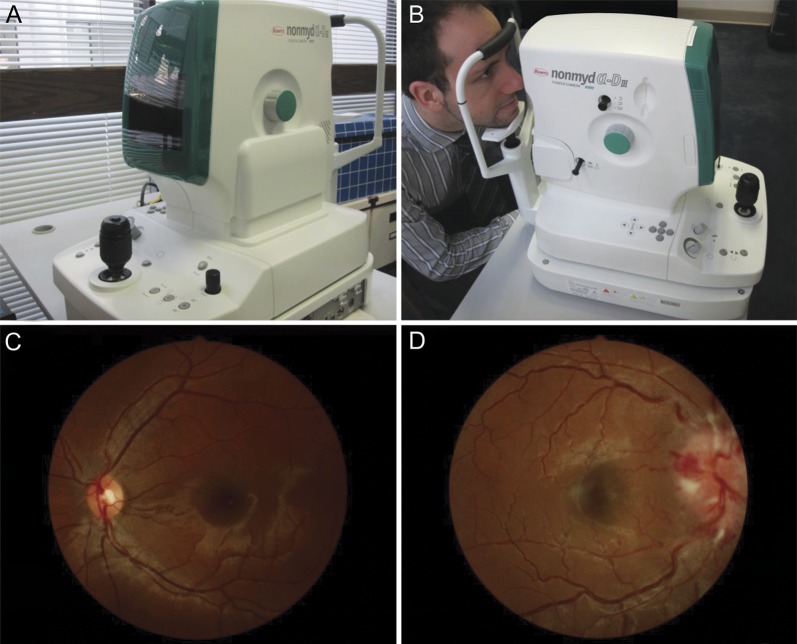
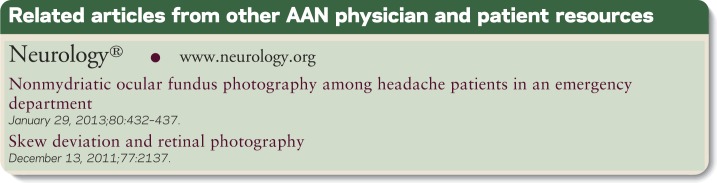
Nonmydriatic retinal cameras are commonly used by ophthalmic professionals. These devices provide a high-quality 45° angle of view of the back of the eye without pharmacologic dilation of the pupils (figure, A–C). They are easy to use, even by non-ophthalmic personnel. Such nonmydriatic cameras are commonly used to screen and monitor chronic retinal or optic nerve diseases, such as glaucoma, diabetic retinopathy, and age-related macular degeneration, but applications in acute medical conditions with particular relevance to neurology have emerged.2,3
Figure. Nonmydriatic fundus photography.
(A, B) External aspect of the camera. (C, D) Examples of ocular fundus photographs from the FOTO-ED study. (C) Normal fundus. (D) Severe optic disc swelling secondary to intracranial hypertension.
The FOTO-ED (Fundus photography vs Ophthalmoscopy Trial Outcomes in the Emergency Department) study assessed nonmydriatic ocular fundus photography for the evaluation of patients presenting to the ED with headaches, visual changes, focal neurologic deficits, or diastolic blood pressure ≥120 mm Hg. This study found that acutely relevant ocular fundus abnormalities (abnormalities that would change the patient's disposition or acute management) were present in 13% of the enrolled patients.2 Early diagnosis of these abnormalities is critical as they often reflect vision- or life-threatening conditions and should alter the patients' management in the ED. For example, optic disc edema related to papilledema from raised intracranial pressure (figure, D) was found in 2.4% of patients who came to the ED for isolated headaches.3 Early recognition of papilledema is important, as severe visual loss occurs in 10% of patients with typical idiopathic intracranial hypertension and in all patients with a fulminant course.4 Unfortunately, nonrecognition of papilledema in headache patients has also become a common cause of legal actions, further emphasizing the need for neurologists to be able to reliably examine the ocular fundus. Similarly, grade III/IV hypertensive retinopathy is a marker of end-organ damage and can differentiate less serious hypertensive urgencies from life-threatening hypertensive emergencies,5 in which stroke and hypertensive encephalopathy occur in 45% of cases.6 Systematic ocular fundus photographs in patients with selected complaints presenting to the ED or the neurologist's office would undoubtedly result in improved patient care.
Feasibility of nonmydriatic retinal photography
Whether in the fast-paced ED setting or in a busy neurologic practice, one of the major concerns is disrupting the flow of patients by adding extra “tests.” The simplicity of nonmydriatic fundus cameras allows non-physician staff to obtain high-quality images after only 15–30 minutes of training.7 In the FOTO-ED study, nurses and patients found fundus photographs easy and comfortable; it took less than 5 minutes for nurses to obtain ocular fundus photographs of both eyes in the triage room. While the FOTO-ED study focused on adults, improving ocular fundus examination in children in the ED is also a concern, since 18.2% of patients presenting to the ED in the US are younger than 16 years old, among whom more than half are younger than 5. One study (not designed specifically for emergency care) found that good quality nonmydriatic fundus photographs could be obtained in children 3 years of age or older.8 Nevertheless, one limitation of tabletop nonmydriatic fundus cameras for patients of all ages is that they require a cooperative patient who is able to sit upright; however, handheld models that are somewhat more challenging to use and that have smaller fields of view are available.
The cost-effectiveness of nonmydriatic ocular fundus photography has not been evaluated in the ED or specific neurologic settings and is difficult to measure because there is substantial heterogeneity in the underlying conditions that present with ocular fundus abnormalities and a wide range of visual and medical outcomes. However, the cost-effectiveness of nonmydriatic photography screening has been demonstrated in sight-threatening conditions with similar or lower frequencies of relevant findings than those seen in the ED (e.g., diabetic retinopathy screening).9,10 This cost-effectiveness would be expected to extend at least to the high-acuity ED environment, and further technological improvements should enhance imaging capability while decreasing cost.
Ability of non-ophthalmologist physicians to read fundus photographs
An advantage of digital ocular fundus photographs is that they can be immediately integrated into the patient's electronic medical record. Phase II of the FOTO-ED study11 showed that ED physicians reviewed 68% of the ocular fundus photographs made available to them in their patients' electronic medical records (compared to only 14% of ED physicians documenting the use of a direct ophthalmoscope in phase I of the FOTO-ED study2). One of the major findings of the FOTO-ED study is that none of the ocular fundus abnormalities were correctly identified by the ED physicians using the direct ophthalmoscope in phase I of the study,2 whereas 46% of the ocular fundus abnormalities were correctly identified by untrained ED physicians on fundus photographs in phase II of the study.11 These results suggest that removing the technical obstacle of the ophthalmoscope would not only encourage non-ophthalmologists to examine the ocular fundus but would also greatly increase their ability to identify obvious abnormalities involving the optic nerve and the back of the eye. Developing specific training on interpreting fundus images for non-ophthalmologists should only lead to further improvement.
Applications in telemedicine
Although reading ocular fundus photographs is much easier than trying to examine the fundus through an ophthalmoscope, occasional support from an expert can be critical. A major advantage of digital ocular fundus photographs is their ability to be easily e-transmitted for remote interpretation, expanding the concept of “teleneurology” commonly applied to acute stroke care. These remotely transmitted photographs can even be interpreted by an ophthalmologist “on the road” using a smartphone or a tablet.12 However, as with any use of telemedicine, very important issues need to be addressed, including confidentiality of image transfer, privacy, medico-legal protection of the interpreter, and billing for interpretation of the photographs. Regulations vary from state to state in the US and are evolving rapidly with the expansion of telemedicine.
CONCLUSION
Nonmydriatic ocular fundus photography provides reliable and high-quality images of the ocular fundus. The technical aspects can be delegated to non-physician staff, and medical interpretation can be performed by non-ophthalmologists for a key subset of relevant fundus abnormalities that have vision- or life-threatening implications. While there remain substantial challenges to widespread deployment of e-transmission of ocular fundus photographs for patient care, nonmydriatic fundus photography has the potential to replace the ophthalmoscope in the neurologist's office and to improve neurologic care.
STUDY FUNDING
Supported in part by an unrestricted departmental grant (Department of Ophthalmology) from Research to Prevent Blindness, Inc., New York, and by NIH/NEI core grant P30-EY06360 (Department of Ophthalmology).
DISCLOSURES
S. Bidot receives research support from Berthe Fouassier's Foundation (Paris, France) and Philippe Foundation (New York, NY). B. Bruce serves as a consultant for Kaiser Permanente of Georgia for the CDC Vaccine Safety Datalink; receives research support from Teva Pharmaceuticals, Pfizer, Novartis, and the NIH; and was a recipient of the Practice Research Fellowship. N. Newman serves as an associate editor for the Journal of Neuro-Ophthalmology, on the editorial board of the Journal of the Neurological Sciences, and as executive editor of the American Journal of Ophthalmology; receives publishing royalties for Neuro-Ophthalmology Illustrated (Thieme, 2009), Walsh & Hoyt's Clinical Neuro-Ophthalmology The Essentials, 1st and 2nd editions (Lippincott Williams & Wilkins, 1999, 2008), Walsh & Hoyt's Clinical Neuro-Ophthalmology, 5th and 6th editions (Lippincott Williams & Wilkins, 1998, 2005), and Blue Books of Neurology: Neuro-Ophthalmology (Butterworth Heinemann Elsevier, 2008); serves as a consultant for Santhera Pharma, Trius Pharma, and Anabasis; received the Research to Prevent Blindness Lew R. Wasserman Merit Award; and has provided expert testimony on the topic of papilledema. V. Biousse serves on the editorial boards of the American Journal of Ophthalmology and the Journal of Neuro-ophthalmology; receives publishing royalties for Walsh and Hoyt's Clinical Neuro-Ophthalmology (Williams and Wilkins) and Neuro-Ophthalmology Illustrated (Thieme); and receives research support from Anabasis and Research to Prevent Blindness. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
REFERENCES
- 1.Benbassat J, Polak BC, Javitt JC. Objectives of teaching direct ophthalmoscopy to medical students. Acta Ophthalmol 2012;90:503–507. [DOI] [PubMed] [Google Scholar]
- 2.Bruce BB, Lamirel C, Wright DW, et al. Nonmydriatic ocular fundus photography in the emergency department. N Engl J Med 2011;364:387–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thulasi P, Fraser CL, Biousse V, Wright DW, Newman NJ, Bruce BB. Nonmydriatic ocular fundus photography among headache patients in an emergency department. Neurology 2013;80:432–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thambisetty M, Lavin PJ, Newman NJ, Biousse V. Fulminant idiopathic intracranial hypertension. Neurology 2007;68:229–232. [DOI] [PubMed] [Google Scholar]
- 5.Pérez MA, Bruce BB, Newman NJ, Biousse V. The use of retinal photography in nonophthalmic settings and its potential for neurology. Neurologist 2012;18:350–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Phillips RA, Greenblatt J, Krakoff LR. Hypertensive emergencies: diagnosis and management. Prog Cardiovasc Dis 2002;45:33–48. [DOI] [PubMed] [Google Scholar]
- 7.Bruce BB, Lamirel C, Biousse V, et al. Feasibility of nonmydriatic ocular fundus photography in the emergency department: phase I of the FOTO-ED study. Acad Emerg Med 2011;18:928–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Toffoli D, Bruce BB, Lamirel C, Henderson AD, Newman NJ, Biousse V. Feasibility and quality of nonmydriatic fundus photography in children. J AAPOS 2011;15:567–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones S, Edwards RT. Diabetic retinopathy screening: a systematic review of the economic evidence. Diabet Med 2010;27:249–256. [DOI] [PubMed] [Google Scholar]
- 10.Younis N, Broadbent DM, Harding SP, Vora JP. Incidence of sight- threatening retinopathy in Type 1 diabetes in a systematic screening programme. Diabet Med 2003;20:758–765. [DOI] [PubMed] [Google Scholar]
- 11.Bruce BB, Thulasi P, Fraser CL, et al. Diagnostic accuracy and use of nonmydriatic ocular fundus photography by emergency physicians: phase II of the FOTO-ED study. Ann Emerg Med 2013;62:28–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lamirel C, Bruce BB, Wright DW, Newman NJ, Biousse V. Nonmydriatic digital ocular fundus photography on the iPhone 3G: the FOTO-ED study. Arch Ophthalmol 2012;130:939–940. [DOI] [PMC free article] [PubMed] [Google Scholar]