Abstract
Mental health parity laws require insurers to extend comparable benefits for mental and physical health care. Proponents argue that by placing mental health services alongside physical health services, such laws can help ensure needed treatment and destigmatize mental illness. Opponents counter that such mandates are costly or unnecessary. The authors offer a sociological account of the diffusion and spatial distribution of state mental health parity laws. An event history analysis identifies four factors as especially important: diffusion of law, political ideology, the stability of mental health advocacy organizations and the relative health of state economies. Mental health parity is least likely to be established during times of high state unemployment and under the leadership of conservative state legislatures.
Keywords: mental health, mental health policy, mental health services
Most citizens of the United States acquire health care through employers. Although this employer-based system has typically covered most physical illnesses, mental health services have historically been specifically excluded or minimally covered (Frank and McGuire 2005). Mental health parity laws mandate that employers provide equal types of benefits for mental and physical illnesses (Mechanic and McAlpine 1999). An examination of the contested history of these laws brings to light the eroding boundary between mental and physical health; the shifting rights and obligations of government, business groups, and citizens; and the emerging social acceptance of mental illness and its treatment (Goffman 1963; Kershaw 2008; Link et al. 1999; Martin, Pescosolido, and Tuch 2000; McSween 2002; Scheff 1964).
States have imposed a variety of mental health parity mandates on employers since the 1980s (Caronna 2004), ranging from no mandates to comprehensive mandates. In an attempt to consolidate the patchwork of state parity laws, the U.S. Congress passed the Mental Health Parity Act (MHPA) of 1996. The MHPA was an important symbolic accomplishment to be sure, though it was too limited and attenuated to ensure mental health parity. Following its sunset in 2005, Congress once again passed federal mental health parity legislation, the Mental Health Parity and Addiction Equity Act of 2008 (effective July 2010), which more forcefully prevents employers from exempting patients with mental illness.
Given the infrequency of federal legislation and the weakness of the 1996 federal law, the battle for mental health parity was fiercely contested at the state level between 1980 and 2005. The purpose of this article is to understand and model the factors precipitating passage of these state mental health parity laws and to situate our findings within a broader explanation of legal and policy change. We use ideas from medical sociology, political sociology, and the sociology of law to understand variation in state mental health parity legislation between 1980 and 2005. Bridging these literatures, we draw on Amenta’s (1998) institutional politics theory to explain state passage of parity laws. From a political perspective, we consider government ideology, and from an institutional perspective, we consider economic pressures, organizational structures, and diffusion of law.
At the most basic level, mental health parity seeks to provide equality for people with a mental illness, allowing their continuous care. Beyond the economic and health care concerns associated with mental illness, such laws symbolically seek to “delabel” (Trice and Roman 1970) and destigmatize mental illness (Mechanic 2003). Parity legislation thus provides a window into the political and institutional conditions that helped tear down the wall between physical and mental health coverage, resulting in an increasing acceptance of, and even expectation for, equal mental health coverage.
BACKGROUND
In the United States, the state-level battle over employer coverage of mental health services followed significant shifts in health care reimbursement and mental health care in the United States. Driven in part by the expense of programs such as Medicare and Medicaid, the economic burden of medical care became a major concern of federal and state governments (Caronna 2004; McKinlay and Marceau 2005; Quadagno 2005). These economic concerns prompted health policy that used market mechanisms to contain costs in the 1970s and 1980s (Caronna 2004:50), such as the gradual introduction of health maintenance organizations (Mechanic 2004; Shi and Singh 2001; Tausig, Michello, and Subedi 1999). At the same time, advances in mental health treatment and the shift from hospital-based to community-based treatment contributed to a greater need for mental health service coverage (Joint Commission on Mental Illness and Health 1961; Mechanic and Rochefort 1990; Tausig et al. 1999).
Within this context of economic concerns about health care reimbursement and broader changes in the structure of mental health services, debates about mental health care reimbursement emerged. A fundamental rationale for mental health parity is the equality it promotes by providing fair access and the option of coverage for mental health treatments through employer-based health insurance plans (Mechanic 2003:1229). Beyond equality, fundamental economic forces are consistently at the forefront of debates about mental health parity, as with health care more generally.
Mental illnesses are frequently chronic, requiring long-term care, and individuals with mental illnesses run a high risk of having comorbidities that may require expensive long-term care (Mechanic 2003, 2004; Sturm and Pacula 1999). When offering health insurance to such populations at risk for incurring expenses, insurance providers consider two key economic forces: moral hazard and adverse selection (Frank, Koyanagi, and McGuire 1997). “Moral hazard” refers to situations in which increased coverage motivates individuals to demand more services, particularly as the cost associated with each service drops. Adverse selection takes place when individuals enroll in specific health plans because they anticipate needing specific types of coverage, resulting in a higher proportion of “high-risk” individuals in those plans. Employers and insurers are particularly sensitive to the problem of moral hazard, and there is some evidence that moral-hazard problems in mental health care are especially acute (Frank et al. 1997; Newhouse 1993). Yet evidence suggests that the introduction of managed behavioral health care was not associated with significant increases in expenses (Sturm 1997; Sturm, Zhang, and Schoenbaum 1999). For instance, Goldman, McCulloch, and Sturm (1998) found that although the number of employees using mental health services at a firm increased after managed behavioral care was introduced, more costly expenses were less likely to be incurred (e.g., inpatient admission).
Given these issues, legislators must balance calls for equality against calls for fiscal restraint. In the early 1980s, individual states began considering legislation mandating equal coverage for mental health care. Although this legislation had an important impact because it mandated continuous mental health care in employer-based health plans, previous federal legislation known as the 1974 Employee Retirement Income Security Act (ERISA) provided an exemption for large employers that self-insure. ERISA specifically provides self-insuring employers exemptions from state health insurance mandates such as mental health parity laws (Buchmueller et al. 2007).
Over the next decade, the increasing prevalence of state-level parity legislation, as well as the push for equitable coverage despite economic concerns, set the stage for debate about mental health parity at the national level. This debate began in the midst of President Clinton’s 1993 health care reform proposal, as mental health advocates and powerful state actors, notably Senator Pete Domenici and the late Senator Paul Wellstone, made the case for parity (Amenta and Poulsen 1996; Hausman 2002). The debate over mental health reform culminated in the first federal mental health law, the federal MHPA, albeit in a limited and attenuated form (U.S. Government Printing Office 1996):
In the case of a group health plan (or health insurance coverage offered in connection with such a plan) that provides both medical and surgical benefits and mental health benefits…. If the plan or coverage does not include an aggregate lifetime limit on substantially all medical and surgical benefits, the plan or coverage may not impose any aggregate lifetime limit on mental health benefits. (110 U.S. Statute 2945)
Beyond these stipulations, if plans imposed limits on coverage (e.g., annual limits on benefits) they were required to set equal limits for medical, surgical, and mental health benefits. Nevertheless, the fine print of the federal MHPA permitted exemptions for companies both large and small, and those plans that did offer mental health coverage had great flexibility to restrict coverage. Given these exemptions, at least three quarters of employer-sponsored health plans were still placing greater restrictions on mental or behavioral health coverage in 1997 (Buck et al. 1999). In essence, the federal law functioned as a symbolic expression rather than a mandate to provide care (Gitterman, Sturm, and Scheffler 2001; Otten 1998).
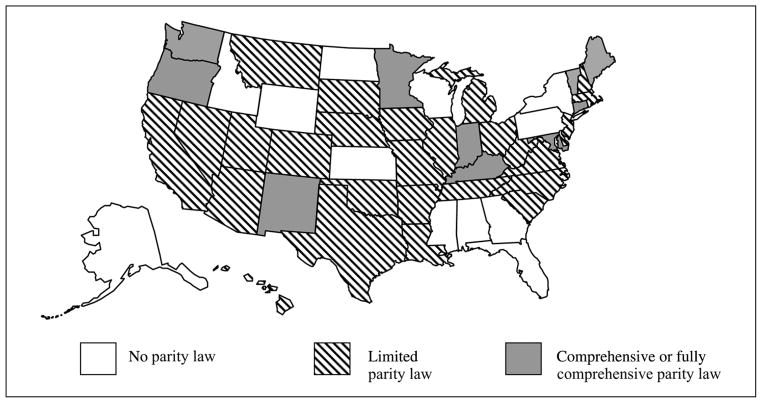
Following the national legislation, state-level mental health parity legislation also expanded in the 1990s but faced the same discord over employer exemptions, resulting in considerable variation in state mental health parity laws and the coverage they mandate. We focus our analysis on the years 1980 to 2005, examining data from the National Conference of State Legislatures (NCSL) as well as Mental Health America (MHA; formerly known as the National Mental Health Association). When the MHPA was allowed to sunset in 2005, most mental health policy advocates concentrated their attention on passing federal legislation, efforts that culminated in passage of the Mental Health Parity and Addiction Equity Act of 2008. This makes the period from 1980 to 2005 especially appropriate for a state-level analysis. Figure 1 shows the spatial distribution of mental health parity legislation during this period. By 2005, five states had parity laws that applied to treatment for mental health and substance abuse under private insurance: Maryland (1994), Minnesota (1995), Vermont (1997), Connecticut (1999), and Oregon (2005). In addition to these fully comprehensive laws, six states had passed comprehensive parity laws (Indiana, Kentucky, Maine, New Mexico, Rhode Island, and Washington) with narrowly defined limitations and exemptions. Twenty-seven states had passed limited parity laws that apply only to select populations, such as those with severe mental illnesses.
Figure 1.
Mental Health Parity State Mandates (2005)
Source: National Congress of State Legislatures and Mental Health America.
EXPLAINING STATE VARIATION IN MENTAL HEALTH PARITY LAWS
A Conceptual Model of Social Policy Reform and State Mental Health Parity
We next develop a basic conceptual model that uses institutional politics theory (Amenta 1998) to explain state passage of mental health parity laws. Designed to explain sources of government social provision, institutional politics theory aims to resolve differences between institutional and political theory (Amenta and Poulsen 1996:34) and delineate how they combine to influence social policy (Amenta 1998:19). Amenta (1998:19) contended that political systems that are underdemocratized or include party systems that are patronage oriented significantly hinder the passage of government social spending policies. Underdemocratized political systems are characterized by restrictive democratic processes, such as unfair voting or political assembly rules, and patronage-oriented party systems maintain power by rewarding their supporters with individual benefits. Conversely, reform-oriented regimes, defined as governments that are aligned with groups and constituencies that support spending, will promote social expenditures (Amenta 1998:19). Amenta and Poulsen (1996) used this theory to highlight the institutional and political conditions that promoted social spending in the United States following the New Deal. For instance, they identified voting rights as an important institutional factor that affected passage of Old-Age Assistance pensions. In a similar manner, they posited that political conditions, including prospending actors, play an equally crucial role in the passage of such programs.
Although institutional politics theory has yet to be applied to state mandates such as mental health parity laws, the theory offers an appropriate framework for examining the expansion of mental health coverage. In a manner similar to the state-level responses to the New Deal, states responded to the federal legislation based upon a combination of institutional and political conditions (Amenta 1998:170). Minnesota, for example, was among the first states to pass mental health parity legislation. During the late 1980s and early 1990s, this state exemplified a highly democratized political system led by a reform-oriented party system with a history of social spending support (Amenta and Poulsen 1996:40). In this political atmosphere, Minnesotans elected a powerful ally for mental health parity legislation, the late Senator Wellstone. With the help of Wellstone, a dynamic political actor, mental health parity legislation was brought to the national forefront in an example of vertical policy diffusion from the state to the national level (Shipan and Volden 2006).
To explain the passage of mental health parity laws among all states, we isolate specific institutional and political conditions salient for mental health legislation, as outlined in Figure 2. In so doing, our framework builds on institutional politics theory but is also based on theoretical perspectives from medical sociology, political sociology, and the sociology of law. From a political perspective, we identify government ideology, and from an institutional perspective, we identify economic pressures, organizational structures, and diffusion of law as important drivers of mental health parity legislation.
Figure 2.
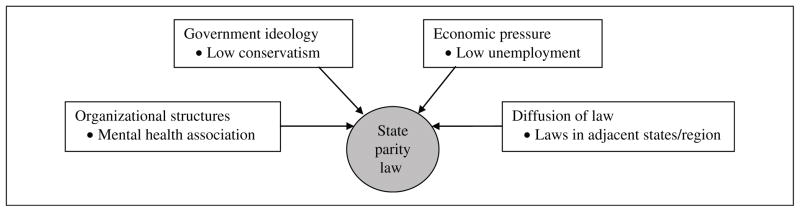
Conceptual Framework
Political Conditions
Government ideology
As with other state policies, debates about mental illness take place against the backdrop of partisan politics and state power (Erikson, Wright, and McIver 1993; Quadagno and Meyer 1989; Starr 2011). To understand the political conditions that promote social provision at the state level, Amenta and Poulsen (1996:37) drew from a social democratic model, anticipating that redistributive public policies would be most likely to pass when left-wing political parties are in office. They thus predicted greater state-level public spending on social provision under Democratic leadership.
We too hypothesize that mental health parity laws were more likely to pass under Democratic leadership. Following the era of federal involvement, the 1980s ushered in an era of conservative leadership that supported the application of market mechanisms to contain rising costs (Caronna 2004). Within a decade, however, physicians, politicians, and the public resisted this market-based approach to cost containment (Mechanic 2001), rejecting the rationing that had become associated with the introduction of managed care. By the early 1990s, the policy environment was primed for health reform that protected patient rights to equal coverage (Caronna 2004; Quadagno 2005; Wright, Erikson, and McIver 1987).
The fragmented U.S. system of government fosters a wide spectrum of state government ideologies and political environments, offering varying support for mental health parity legislation. We therefore do not expect that partisan power or affiliation alone will dictate policy formation at the state level. Above and beyond party affiliation, we anticipate that states with more conservative government ideologies (Berry et al. 1998; Erikson et al. 1993) and elected officials will be especially resistant to mental health parity laws.
Institutional Conditions
Economic pressures
Economic factors clearly affect the characteristics and distribution of employer-based health insurance (see, e.g., Cubbins and Parmer 2001). Insuring individuals with mental illnesses is potentially expensive, as they are more likely to require high-cost, long-term care (Mechanic 2003:1229–30). At the state level, there are conflicting objectives between the mental health care providers who supply their care and the corporations that insure them. In the simplest terms, providers want their care to be reimbursed, but insurance companies want to avoid insuring the potentially high-cost risk pool composed of individuals with mental illnesses.
These competing objectives clash at the state level when corporations and associations lobby individually and collectively against passage of mental health mandates (Mintz 1995; Mintz and Palmer 2000; Quadagno 2005). States are likely to be particularly sensitive to corporate and association resistance during bad economic times (Imershein, Rond, and Mathis 1992), when firms can argue that extending benefits could lead to job loss and higher unemployment. Therefore, states facing greater economic strain should be less likely to pass mental health parity laws.
Organizational structures
Our model of social policy also emphasizes the role of larger organizational structures, including interest groups and associations (Amenta, Bonastia, and Caren 2001; Caronna 2004; Quadagno 2005). Mental health advocacy groups have a vested interest in aiding passage of mental health parity laws. Although it is difficult to establish a causal relationship, previous evidence shows that voluntary associations can indeed influence policy formation (Skocpol et al. 1993). The National Alliance on Mental Illness (NAMI), founded in 1979, is the largest grassroots group dedicated to mental health advocacy, research, and education. NAMI advocates for inclusive health policy, such as mental health parity, but there has been significant variation in state NAMI representation over recent decades. We predict that the presence of a state-level NAMI association will be positively related to passage of state mental health parity legislation. Aside from the presence of a state-level NAMI association, we also anticipate that its stability and duration—the degree to which the association has become institutionalized—will affect the passage of parity laws.
On the other side of the debate for mandated mental health coverage, business associations, such as the National Business Group on Health (NBGH; formerly the Washington Business Group on Health) represent powerful employers that influence health policy at the national level (Mintz 1995). Along with the NBGH, the largest national business lobbying group, the U.S. Chamber of Commerce, strongly opposed mental health mandates in the 1990s (Wood 2005). Yet the NBGH and the Chamber of Commerce primarily represent the interests of firms at the national level; the strength of these lobbying groups may thus bear little relation to state-level mental health policy. Instead, we focus on the presence of self-insuring employers in each state that have greater economic motivation to prevent passage of state parity laws. Even though self-insuring firms are exempt from state-level legislation, most opposed any mental health parity legislation during the time period included in our analysis. Thus, although this is an indirect measure, we anticipate that the presence of Fortune 100 companies and a higher proportion of self-insuring firms in a state will have a negative influence on passage of mental health parity legislation.
Diffusion of law
Neoinstitutional models of legal diffusion suggest that legal change occurs in predictable spatial and historical patterns (Edelman 1990; Edelman, Uggen, and Erlanger 1999; Frank, Camp, and Boutcher 2010; Grattet, Jenness, and Curry 1998; Jenness 1999; McCammon et al. 2001). In their analysis of the homogenization of hate crime laws, for example, Grattet et al. (1998) noted that policy makers often have a limited understanding of “what constitutes optimal policy, especially in terms of acceptability to key constituencies” (p. 288). Their policy choices are thus contingent on the information and experience they can draw from other policy making bodies. At the state level, this transfer of information through social policy networks results in states mimicking policies adopted in other states (Berry and Berry 1990; Eyestone 1977; Grattet et al. 1998; Walker 1969).
We anticipate that state mental health parity laws will spread across time and space in a manner consistent with these models. First, states often follow federal leadership, particularly regarding equal opportunity legislation (Edelman 1990; Hill 1986). We hypothesize that states will react to the elevated importance of mental health parity legislative reform in the mid-1990s, and they will be more likely to pass mental health parity laws shortly after the 1996 federal MHPA. Second, changes to state laws generally cluster together in time; therefore, we expect that states will pass laws in quick succession. As Grattet et al. (1998:289) hypothesized, the likelihood of a state adopting legislation is time-specific and contingent on period effects. Finally, we anticipate regional clustering of parity laws, as states look to their neighbors for effective models (Berry and Berry 1990; Grattet et al. 1998). More specifically, we hypothesize that states will pass mental health parity laws if other states in close regional proximity have passed laws.
Beyond spatial proximity, regions also provide a proxy for “similar social and political conditions” (Grattet et al. 1998). Erikson et al. (1998) stipulated that a “theory of state electoral politics must take into account the wide variation in the ideological orientations of state political parties” (p. 731); quite simply, a Democratic state legislator in Mississippi may vote differently than a Democratic state legislator in Minnesota. We consider this regional variation in government ideology in our diffusion framework, and we hypothesize that states within the same region will pass similar laws (Behrens, Uggen, and Manza 2003; Berry and Berry 1990; Eyestone 1977).
On the basis of the four factors described—government ideology, organizational structures, economic pressures, and diffusion of law—we draw the following four sets of hypotheses:
-
Hypothesis 1
States with more conservative elected officials will be less likely to pass mental health parity laws.
-
Hypothesis 2a
States with mental health associations (NAMI), particularly well-established ones, will be more likely to pass mental health parity laws.
-
Hypothesis 2b
States with more Fortune 100 companies and/or higher percentages of firms that self-insure will be less likely to pass mental health parity laws.
-
Hypothesis 3
States will be less likely to pass mental health parity laws during times of high unemployment than times when unemployment is low.
-
Hypothesis 4a
States will be more likely to pass mental health parity laws following the federal MHPA of 1996.
-
Hypothesis 4b
States will be more likely to pass mental health parity laws if other states in their region passed parity laws.
DATA AND METHODS
Data on state mental health parity laws were coded using information from the NCSL and MHA for laws passed between 1980 and 2005. A table classifying the 2005 mental health parity laws, adapted from materials provided by MHA and the NCSL, is provided in the Appendix and mapped in Figure 1.1 To test our conceptual model (see Figure 2), we consider both the simple presence of parity laws and the extent to which they provide comprehensive coverage. Laws were coded at year of passage as “limited” or “comprehensive” based upon the type of services required or the exceptions allowed within each health plan. Comprehensive parity laws (identified as “best” or “good” by the MHA) apply to all or nearly all treatment of mental illness and substance abuse covered by private health plans. Limited parity laws apply to select groups only or provide partial protection for those with mental illnesses.
Between 1980 and 2005, only 11 states passed comprehensive mental health parity laws, whereas 29 states passed limited mental health parity laws. For our analysis, we included states passing comprehensive parity legislation in the total number of states passing (at least) a limited state mental health parity law. As the Appendix and the hazard function in Figure 3 show, most laws were passed in the late 1990s and early 2000s.2 Overall, 74 percent of states (38) had passed at least some form of parity law by the end of 2005. To test the hypotheses above, we conduct an event history analysis of factors influencing law passage for the period before the federal MHPA of 1996 and a parallel analysis for the period after the federal legislation.
Figure 3.
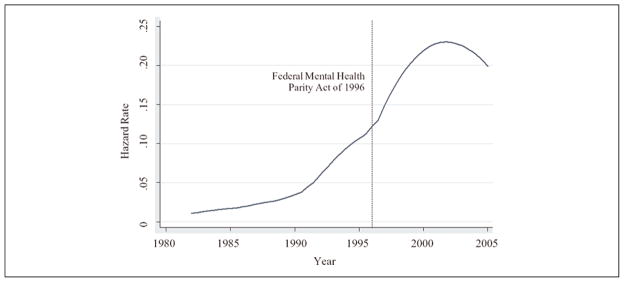
Smoothed Hazard Function Estimate for Time to Passage of Any Parity Law
To test the association between government ideology and parity legislation, we use a well-established measure of state government ideology from Berry et al. (1998:327–28), which is based on roll-call voting scores of state congressional delegations. These scores are then weighted by the balance of partisan strength within each state. We use the updated government ideology scores created by Berry et al. in their revised 1960 to 2006 government ideology series data. For the purposes of this article, we reverse-coded these ideology scores so that higher scores indicate more conservative state ideologies (on a scale ranging from 1 to 100), and we divided the resulting scores by 10 so that all scores represent a 10-point change in government ideology.
We operationalize state economic pressures using the state unemployment rate for each year. The data are taken from the U.S. Census Bureau’s Statistical Abstract series for 1980 to 2005, providing a time-varying index of the prevailing economic environment and strain present in each state.3
We include several measures of state-level organizational structures. We used the Encyclopedia of Associations: Regional, State and Local Organizations for the years 1996 to 2005 to determine whether states had NAMI associations in each year. States were coded 1 if they were home to NAMI associations in a given year and 0 otherwise. Annual state-level association information was not available prior to 1988, so we created a dichotomous measure to indicate when each state NAMI association was established for the earlier period between 1980 and 1995.4 As an indicator of the stability, duration, and solvency of the NAMI associations during the later period, we computed a measure of the years since a state-level association had been established, ranging from 0 to 22 years. If any state NAMI association was not solvent in a particular year, but was established in the following year, the count restarted at 0.
We also use a measure of the percentage of “private-sector establishments that offer health insurance that self-insure at least one plan” taken from the 1993 Medical Expenditure Panel Survey (U.S. Department of Health and Human Services 1996). The survey is not conducted annually, so we use the earliest available survey data from 1993 and apply the same proportion of self-insuring firms for all of the years in the analysis for the second period (1996–2005). Finally, we include a measure of the number of Fortune 100 companies in the state for each year, ranging from 0 to 22 firms per state.
With regard to the diffusion of law, we estimate the effects of both region and timing. We use a standard Census Bureau four-category region classification to represent the Northeast, Midwest, South, and West as separate indicator variables. As a measure of regional diffusion, we include a variable representing the percentage of states that have passed mental health parity laws in each of nine divisions (subcategories of regions) in each of the immediately preceding years between 1980 and 2005 (see, e.g., Grattet et al. 1998).
State-level analysis is well suited to assessing variation in health policy (e.g., Mintz and Palmer 2000). Unlike cross-sectional studies, we use an event history approach to model the time-varying factors associated with legal change (Allison 2010; Yamaguchi 1991). We estimate the likelihood of mental health parity law passage using a discrete-time logistic regression model:
In this equation, Piy represents the conditional probability of a mental health parity law being passed in state i during year y, given that a law has not already been passed in that state. Explanatory variables are represented as X1, X2, …, Xk, with time-varying covariates denoted by a y subscript. β represents the effect of the independent variables, and αy represents a set of constants corresponding to each year. In these models, time is specified in discrete intervals (years). The dependent variable indicates whether the event (passage of a mental health parity law) did or did not occur within a given interval for all units (states) at risk for the event. The data are analyzed in a “state-year” structure, with the outcome coded 1 for years in which a first parity law was passed and 0 otherwise. Once a state passes such a law, it is removed from the risk set and contributes no subsequent observations to the analysis. Because state legislation operates on yearly rather than continuous cycles, discrete-time methods have been especially well suited to studies of state-level legal change, including the passage of state hate-crime laws (Grattet et al. 1998), felon voting restrictions (Behrens et al. 2003), and worker compensation legislation (Pavalko 1989).
Discrete-time models require some method of accounting for duration dependency. The most typical specification involves temporal dummy variables, though other transformations often produce better fitting models (Box-Steffensmeier and Jones 2004). Following Allison (2010), we inspected the hazard distribution in Figure 3 and compared fit statistics for several specifications of time dependency, including individual year dummy variables, a linear trend, and a quadratic model with both the linear trend and its square. The best-fitting models for the first period and for our comprehensive parity models include the year term alone, but the best-fitting model for the second period includes both year and year-squared terms. We will first examine the duration structure of the data using a nonparametric hazard techniques, before turning to parsimonious multivariate models that assess the effects of government ideology, economic strain, associations, and legal diffusion.
RESULTS
In Figure 3, we show the hazard distribution for time to passage of any parity law. This plot illustrates how the national picture changes over time, as a reflection of both national- and state-level processes. The first seven laws were passed in the 1980s and were limited in scope, and the first comprehensive law was not passed until 1994. By 1996, a total of 14 states had passed some form of mental health parity legislation. Many states passed laws in the late 1990s, as indicated by the upward trend in the hazard distribution. The peak rate of passage occurs in the early 2000s but declines slightly in 2005. The original federal MHPA of 1996 was allowed to sunset in 2005, and mental health policy advocates had begun to focus their attention on passing new federal legislation.
Next, we consider the effects of the independent variables on the time until passage of these laws. Descriptive statistics for the time-varying and time-invariant independent variables are shown in Table 1. For all states from 1980 to 2005, the unemployment rate ranged from 2 percent to 18 percent, with an average rate of about 6 percent. The conservative ideology measure ranged from 0.21 to 10, with a mean of 5; approximately one third of all states had Republican-controlled legislatures, and about half had Republican governors. During the first period, about 70 percent of states had established NAMI organizations. Between 1996 and 2005, half the states had NAMI organizations, which had been in operation for an average of 2.13 years. The average percentage of private-sector establishments that self-insure at least one plan was 21 percent, and on average, states had about two Fortune 100 companies. The regional means reflect the proportion of state-years contributed by a given region in the analysis, prior to any adjustments for censoring (e.g., the 9 states in the northeastern region constitute 0.18 of the total observations).
Table 1.
Description of Variables
| Variable | Description | Mean or % | Minimum | Maximum | Expected Effect |
|---|---|---|---|---|---|
| Government ideology | |||||
| Conservative ideology a | Conservative state legislator ideology | 5.04 | 0.21 | 10.00 | − |
| Republican control | Republican control of both legislative houses | 0.28 | 0 | 1 | − |
| Republican governor | Republican governor | 0.52 | 0 | 1 | − |
| Economic pressures | |||||
| Unemployment rate | State unemployment rate | 5.93 | 2.20 | 18.00 | − |
| Organizational structures | |||||
| State NAMI association, period 1 | NAMI association at state level (1980–1995) | 0.69 | 0 | 1 | + |
| State NAMI association, period 2b | NAMI association at state level (1996–2005) | 0.50 | 0 | 1 | + |
| State years since NAMI association was establishedb | Years since NAMI association established | 2.13 | 0.00 | 22.00 | + |
| Fortune 100 companiesb | Number of Fortune 100 companies | 1.95 | 0.00 | 22.00 | − |
| Percentage self-insuringb | Percentage of private-sector establishments that offer health insurance that self-insure at least one plan | 21.01 | 6.70 | 34.30 | − |
| Diffusion of law | |||||
| States in region with law | Percentage in nine-category census region that have passed law | 29.08 | 0.00 | 100.00 | + |
| Northeast | Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, Vermont | 0.18 | 0 | 1 | + |
| South | Alabama, Arkansas, Delaware, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, West Virginia | 0.32 | 0 | 1 | − |
| West | Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, Wyoming | 0.26 | 0 | 1 | − |
| Midwest | Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, Wisconsin | 0.24 | 0 | 1 | + |
Note: NAMI = National Alliance on Mental Illness.
The conservative ideology measure is a continuous variable, where 0 equals the most liberal and 10 equals the most conservative. The other two government ideology variables are binary indicators, where 1 equals Republican control (of the governorship or the legislature) and 0 equals other. See text for further details.
Measures included in the analysis of the second period only (1996–2005).
Inspection of the hazard rate revealed a clear rising and falling pattern for the second period, and a comparison of the linear model with the quadratic suggested that the squared term is necessary to appropriately model the duration structure of passage of any parity law after 1996. For the first period, and analysis of comprehensive legislation during the second period, a linear specification of time provides the best fit to the data. All models provided a good fit relative to equations specifying time as a set of individual year dummy variables.
Although the statistical power to detect effects is limited by the small number of states passing laws, particularly comprehensive laws, we built parsimonious multivariate models to consider the effects of the most important predictors on passage of first mental health parity law. The sample size in these models is the total number of state-years (e.g., 50 states over 16 years in model 1 of Table 2 and 50 states over 10 years in models 2, 3a, and 3b) that have not yet passed a mental health parity law and are therefore at risk for passing such legislation. The smaller number of cases in model 2 relative to models 3a and 3b indicates that more states passed a law (limited or comprehensive) more quickly than they passed comprehensive laws. After a law has been passed, the state contributes no more observations or state-years to the analysis. Fewer states were thus at risk for passing limited laws (model 2) relative to comprehensive laws (models 3a and 3b) during much of the period from 1996 to 2005. On the basis of initial analyses considering each variable in turn, we selected the conservative government ideology measure (rather than an indicator of partisan control) to represent the effect of government ideology.5 Given that the number of events is always less than 50 in a state-level analysis of the time until a first law is passed, we estimate parsimonious models (i.e., fewer than 12 covariates).
Table 2.
Multivariate Predictors of First Mental Health Parity Law, before and after the Federal Mental Health Parity Act of 1996
| Variable | Any Limited, Comprehensive, or Fully Comprehensive Legislation
|
Comprehensive or Fully Comprehensive Legislation
|
||
|---|---|---|---|---|
| Period 1 (1980–1995)
|
Period 2 (1996–2005)
|
Period 2 (1996–2005)
|
||
| Model 1 exp(β) | Model 2 exp(β) | Model 3a exp(β) | Model 3b exp(β) | |
| Government ideology | ||||
| Conservative ideology | 0.85 | 0.80* | 0.63** | 0.57** |
| Economic pressures | ||||
| State unemployment rate | 1.08 | 0.53** | 0.67 | 0.61 |
| Organizational structures | ||||
| State NAMI organization present | 0.70 | — | 0.74 | — |
| State NAMI organization stability | — | 0.94 | — | 1.34** |
| Fortune 100 companies | — | 0.99 | 0.84 | 0.67 |
| Percentage self-insuring | — | 0.96 | 1.04 | 1.07 |
| Diffusion of law | ||||
| Percentage in region with law | 1.09*** | 1.05*** | 1.01 | 1.00 |
| Northeast (vs. Midwest) | 1.68 | 0.63 | 2.01 | 1.25 |
| South (vs. Midwest) | 0.88 | 1.18 | 0.34 | 0.27 |
| West (vs. Midwest) | 0.15* | 1.95 | 2.62 | 2.97 |
| Year | 0.99 | 1.27 | 1.01 | 1.02 |
| Year2 | — | 0.99 | — | — |
| Constant | 0.01** | 0.26 | 0.19 | 0.19 |
| χ2 | 28.03*** | 27.39*** | 11.14 | 17.16* |
| −2 log likelihood (df) | 102.07 (8) | 128.22 (11) | 60.40 (10) | 54.38 (10) |
| Events | 13 | 24 | 7 | 7 |
| Number of cases | 719 | 238 | 430 | 430 |
Note: NAMI = National Alliance on Mental Illness. The U.S. Census Bureau divides the four regions into nine divisions, which are used for the measures of diffusion of law. Models 1 and 2 predict the passage of any parity legislation, including limited or comprehensive laws. Models 3a and 3b predict the passage of comprehensive legislation only. The measure of NAMI organization stability indicates the number of years the state NAMI organization has been present. See text for further details.
p < .10,
p < .05, and
p < .01 (two tailed).
We first summarize multivariate predictors of any law passage, including comprehensive laws, for the pre-MHPA period in model 1 of Table 2. Odds ratios greater than 1.0 represent positive effects, and odds ratios less than 1.0 represent negative effects. During this period, only our measures of diffusion predicted parity legislation: The odds ratio of 1.09 for “percentage in census division with law” means that the estimated odds of passing a law rose by 9 percent for each corresponding percentage point increase in the rate of passage in neighboring states. Apart from these findings, however, the model fails to explain passage of parity laws during this early period. Our measures of government ideology, economic pressures, and organizational structures did not significantly predict when the 13 laws passed prior to the MHPA federal legislation.
For the post-MHPA period, government ideology, economic pressures, and diffusion all predicted law passage, as shown in model 2 of Table 2. Consistent with our conceptual model, states were significantly less likely to pass a mental health parity law during times of high unemployment. The odds ratio of 0.53 indicates that the estimated odds of passage drop by 47 percent with each percentage point increase in the unemployment rate. States characterized by a more conservative government ideology were also significantly less likely to pass any law after 1995, although providing a unit-change interpretation of this coefficient is less straightforward because of the metric. Our measures of organizational structures, however, did not significantly predict law passage, nor did we find differences by region. As with the pre-MHPA period, the percentage of states in a division that had passed a law remained a significant predictor of state law passage. In short, diffusion of law, economic pressure, and conservative government ideology emerge as statistically significant predictors of passage of mental health parity laws after the federal MHPA of 1996.
In the final two models of Table 2, we show multivariate predictors of comprehensive law passage (see models 3a and 3b). Only seven states had passed comprehensive laws, so the models become unstable when too many covariates are considered in the same equation. In contrast to the “any parity” analysis, we fail to detect a significant unemployment effect on passage of a comprehensive law. Rather, our measure of government ideology emerges as a powerful predictor of comprehensive laws: States led by politicians with more conservative government ideologies have been significantly less likely to pass these laws. In model 3b, our measure of the stability and duration of NAMI associations emerged as a significant predictor, with the estimated odds of passing a comprehensive law rising by 34 percent with each year since a state NAMI association was first established. Neither Fortune 100 companies nor the proportion of employers self-insuring was associated with passage of comprehensive legislation. Consistent with the geographic scattering of comprehensive parity states shown in Figure 1, we did not detect significant regional effects in these models. Net of our other measures, states with more conservative legislators were significantly less likely to pass comprehensive laws, but those with well-established NAMI associations were significantly more likely to pass them.
DISCUSSION
Over the past 50 years, there have been remarkable changes in how mental illnesses are treated in the United States. Building from theories of institutional politics (Amenta 1998; Amenta and Poulsen 1996), our aim in this study has been to understand and model the conditions that contributed to state mental health parity legislation. We hypothesized that a spectrum of political and institutional forces would influence state passage of these legislative mandates. Using discrete-time logistic regression event history models, we estimated the effects of government ideology, organizational structures, economic pressure, and diffusion of law. Our results generally support the basic hypotheses in our conceptual model of mental health social policy: Parity laws tended to pass in states characterized by less conservative ideology, low unemployment, long-standing advocacy organizations, and geographical proximity to states that had established parity. Yet the relative salience of these factors differed depending on the period and type of law.
Differentiating between states that passed any parity laws versus those that passed a more comprehensive mandate, as well as the period in which they were passed, reveals subtle but important distinctions. Prior to the passage of the federal legislation, the diffusion of laws within census divisions is the only significant predictor of any parity laws. This measure continues to influence legislation following the federal MHPA of 1996, but unemployment rates, government ideology among state legislators, and the presence of a mental health advocacy organization also emerged as significant predictors in the later period.
During the second period, lower unemployment rates were significantly associated with the passage of any type of parity legislation. From a practical perspective, the negative effect of economic pressure makes sense: States are less likely to prioritize mental health parity when there are pressing economic concerns on the public agenda. Corporate and association lobbying against state health mandates may also increase during times of economic strain, as business groups actively resist government mandates. For example, a U.S. Government Accountability Office (2000) survey indicated that employers made benefit changes after the federal MHPA as part of their cost containment efforts. Nevertheless, neither the number of Fortune 100 companies nor the percentage of establishments that self-insure is a statistically significant predictor of parity legislation.
Although states were significantly less likely to pass any parity laws during times of high unemployment, this economic pressure did not influence the likelihood they would pass more comprehensive legislation (nor did our regional measures of legal diffusion). Conservative government ideology and stable advocacy organizations emerged as the most salient predictors of comprehensive parity laws. The importance of government ideology for passage of these more stringent state parity laws supports our prediction that legislation was more likely to pass when left-wing political parties were in power. Although conservative ideology shows a marginal negative association with passage of general laws (limited or comprehensive) in the later period (p<.10), it emerges as a powerful and significant predictor of laws requiring more comprehensive coverage of mental illness treatment. Associations, such as NAMI, provided additional momentum for the passage of state-level comprehensive legislation. Over the years, though, these state-level NAMI associations were not always solvent, and the degree to which these were stable or well established—essentially the degree of institutionalization of each NAMI association—predicted passage of comprehensive parity legislation. On the other hand, neither the number of Fortune 100 companies nor the percentage of self-insuring companies was associated with the passage of any type of law. Our inability to detect such effects may be due to the indirect nature of these measures; we lack a direct indicator of the strength of business association lobbying against parity legislation.
Aside from economic pressures, government ideology, and organizational structures, the spatial distribution of the basic parity laws is at least partially consistent with institutional accounts of legal diffusion (Behrens et al. 2003; Edelman 1990; Frank et al. 2010; Grattet et al. 1998). We found evidence of regionalization when we considered the percentage of states in a division that had passed at least a limited parity law in the preceding year. Although the region indicators are not statistically significant in multivariate models predicting comprehensive parity legislation, northeastern states such as Connecticut and Vermont emerged as institutional leaders in mental health care reform in the 1990s (the midwestern state of Minnesota is a notable exception to this regional pattern). The plot of our hazard function also affirmed our hypothesis that states would be more likely to pass mental health parity laws, limited or comprehensive, following the federal MHPA of 1996. Although we cannot definitively determine the cause of this peak in state laws during the late 1990s and early 2000s, it may reflect a state-level effort to fill gaps in the federal legislation. Until recently, however, no state-level legislation was capable of overriding the ERISA exemption for firms that self-insure; thus, mental health advocates moved to pass additional federal legislation later in the 2000s.
Taken together, these effects reinforce our hypotheses, and the model proposed by Amenta (1998) and Amenta and Poulsen (1996), that both political and institutional factors influence passage of parity laws. At the beginning of the 1990s the health care policy environment was primed for legislation that protected patients’ rights (Quadagno 2005), and regional policy diffusion appears to be important in this early period. Once mental health parity emerged more prominently as a national issue (culminating in the MHPA of 1996), partisan political pressures appeared to play a bigger role, as indicated by the strong effect of conservative government ideology during the more recent period.
Although not included in our analysis, we would be remiss to neglect discussion of several key political actors, representing a variety of political ideologies, who paved the way for national parity legislation (Amenta and Poulsen 1996). Although our account emphasizes structural forces, individual legislators also cite more personal factors. The federal MHPA of 1996 was successfully brought to the forefront of health policy reform by Senator Domenici and Senator Wellstone. Upon Senator Wellstone’s untimely death, other powerful political figures took up the cause to pass federal legislation in the 2000s, including the late Senator Edward Kennedy and his son, Patrick Kennedy. The serious mental illness of close family members appeared to motivate several of these legislators to champion the cause of mental health parity at the federal level, regardless of their political ideologies (Barry, Huskamp, and Goldman 2010; McSween 2002).
Our overarching goal has been to advance substantive knowledge on the important question of mental health parity and to situate such knowledge within a broader explanation of policy change. There are some important limitations of the current analysis, including the relatively small number of states passing laws and the challenge of measuring institutional and political processes in a time-varying structural-level analysis. Although we have taken care to include covariates related to both our state-level predictors and passage of parity laws, omitted variable bias remains a concern in an observational study such as this one. For example, subsequent research would benefit from further consideration of factors such as health maintenance organization market penetration, a variable that was not available to us for individual states prior to 2002, or annual state-level data indexing the stigma associated with mental illness. Despite these limitations and potential omissions, we observe a consistent pattern of variation in mental health parity legislation from 1996 to 2005. States characterized by less conservative government ideologies, low unemployment, and neighboring states with parity laws were likely to pass general (limited or comprehensive) parity provisions. The most comprehensive laws requiring insurers to extend comparable benefits for mental and physical health were passed in states with less conservative ideology and well-established mental health advocacy organizations.
CONCLUSIONS
Although our analysis focuses on state legislation, our model suggests that shifting government ideology and partisan power may help explain the development of federal parity legislation between 1980 and 2005. On December 31, 2005, Congress allowed the federal MHPA of 1996 to sunset, with hopes of new federal mental health parity legislation on the horizon. During subsequent years, legislators in both the U.S. House of Representatives and Senate proposed new versions of federal mental health parity legislation. Led by Senator Domenici, a powerful Republican, Congress eventually found bipartisan support for the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008, which took effect for health plan years beginning on or after July 1, 2010. The law was passed immediately prior to the election of President Barack Obama and preceded the comprehensive Health Care and Education Reconciliation Act of 2010, signed into law on March 23, 2010 (Light 2011).6 Unlike the previous federal law, this most recent mental health parity legislation does not allow for ERISA exemptions for firms that self-insure, thus ensuring more comprehensive coverage for those with a mental illness.
Despite the recent focus on federal legislation, state parity law continues to evolve. A 2009 NAMI survey suggests both continued refinement and substantive changes to state mental health parity laws in Colorado (2007), Idaho (2006), North Carolina (2007), Ohio (2006), Oregon (2006), Washington (2007), and West Virginia (2007). In response to the current patchwork of state and federal law, Tovino (2011) proposed amendments that would conform the state laws to minimum federal requirements and expand the reach of state mental health parity law to encompass all health plans subject to state insurance regulation.
These recent changes and proposals should not obscure the contested history of state parity legislation prior to the 2008 federal law. Declared the “decade of the brain” by presidential proclamation (Bush 1990), the 1990s brought about substantial debate over health care reform and coverage of treatment for mental illnesses (Wolff 2002:791). Despite such attention, though, the decade did not bring about a level of equality in mental health reimbursement sufficient to “symbolically destigmatize” mental illness (Mechanic 2003). The most recent federal legislation represents a significant step toward providing parity, and it suggests an emerging national consensus about the need for equal mental and physical health coverage. If, as Mechanic (2003) argued, mental health parity laws symbolically undermine the stigma associated with mental illness, the issue of reimbursement for mental health services is significant for its symbolic declarative effects as well as its tangible public health policy impacts.
Acknowledgments
We would like to thank Cynthia Goff for her helpful insights about health care policy, as well as Kim Gardner, Andrew Halpern-Manners, Wesley Longhofer, Karen Lutfey, Donna McAlpine, Heather McLaughlin, John Robert Warren, and Suzy McElrath for helpful comments and other assistance. Support for this research was provided by a predoctoral National Research Service Award from the National Institute of Mental Health (T23-MH19893) to Dr. Hernandez and a Robert Wood Johnson Foundation Investigator Award in Health Policy Research to Dr. Uggen.
Appendix
Mental Health America Categorization of Parity Laws (1980–2005)
| Fully Comprehensive Parity Lawsa | Comprehensive Parity Lawsb | Limited Parity Lawsc | No Parity or Mandate Laws |
|---|---|---|---|
| Connecticut (1999) | Indiana (1999/2001/2003) | Arizona (1997/2001) | Alabama |
| Maryland (1994) | Kentucky (2000)d | Arkansas (1997/2001) | Alaska |
| Minnesota (1995) | Maine (1995/2004) | California (1974/1999) | Florida |
| Vermont (1997) | New Mexico (2000) | Colorado (1997) | Georgia |
| Oregon (2005) | Rhode Island (1994/2001) | Delaware (1998/2001) | Idaho |
| Washington (2005)d | Hawaii (1988/2004) | Kansas | |
| Illinois (2001) | Mississippi | ||
| Iowa (2005) | New York | ||
| Kentucky (1986) | North Dakota | ||
| Louisiana (1982/1999) | Pennsylvania | ||
| Massachusetts (2000) | Wisconsin | ||
| Michigan (1988) | Wyoming | ||
| Missouri (2004) | |||
| Montana (1999) | |||
| Nebraska (1999) | |||
| Nevada (1999) | |||
| New Hampshire (1994/2002) | |||
| New Jersey (1999/2002) | |||
| North Carolina (1991/1997) | |||
| Ohio (1985) | |||
| Oklahoma (1999) | |||
| South Carolina (2000/2005) | |||
| South Dakota (1998) | |||
| Tennessee (1998) | |||
| Texas (1991/1997) | |||
| Utah (2000) | |||
| Virginia (2004) | |||
| Washington (1987) | |||
| West Virginia (2004) |
Parity applies to all mental health and substance abuse disorders under private insurance plans. No exemptions.
Not quite comprehensive parity because of certain exemptions and/or limitations.
Parity applies only to select groups, such as those with severe mental illnesses or state and local employees, or protects against only certain types of discrimination.
State passed an earlier limited parity law and a later comprehensive parity law.
Footnotes
For the purposes of this article, we consider both “fully comprehensive” and “comprehensive” laws to be comprehensive mental health parity laws. The NCSL adopts a more complex categorization scheme but is largely consistent with the MHA classification. Our analysis is based on the more focused and intuitive MHA categorization for the period from 1980 to 2005. Although the grouping strategy was slightly different between the MHA and the NCSL, auxiliary analysis revealed that the results remained substantively the same. Two states, Kentucky and Washington, passed earlier limited parity laws and later comprehensive laws and are included in both sets of analyses.
All state-level mental health parity legislation was passed after 1980, except for an earlier, limited law in California, passed in 1974. Thus, California is left censored and hence excluded from analysis of limited parity laws, but it contributes observations to the comprehensive law analysis. When we include California in analysis of the period from 1970 to 2005, we find identical results, though we lack information on some covariates between 1970 and 1980.
We also considered a measure of logged gross domestic product by state (formerly gross state product) from the Census Bureau for each state in each year. However, the Bureau of Economic Analysis strongly cautions against using these data for time-series analysis between 1963 and 2006 because of changes in coding over this period.
The NAMI measure for the first period indicated when each association began but does not account for variation in association presence after it was established (e.g., because of insolvency of state associations). Using the Encyclopedia of Associations, the NAMI measure for the second period does account for such variation.
In our bivariate models (not shown), our measure of conservative government ideology significantly reduced the likelihood of passing any parity laws and comprehensive parity laws separately, but other measures of conservative ideology did not predict law passage. State presence of a NAMI association did not predict passage of laws, but the years since the NAMI association had been established did predict the passage of a comprehensive parity law (during the second period only). Our measures of the percentage of self-insuring firms and the number of Fortune 100 firms in a state were not associated with law passage. Although we did not find regional differences overall, we found that states were significantly more likely to pass a parity law if other states in their division had passed a law.
As of this writing, national health care reform remains the subject of fierce political debate (Jacobs and Skocpol 2010; Starr 2011). Consistent with our conceptual model and findings, Republican leadership is actively mobilizing against the Obama health care initiatives.
References
- Allison Paul D. Survival Analysis Using SAS®: A Practical Guide. 2. Cary, NC: SAS Institute; 2010. [Google Scholar]
- Amenta Edwin. Bold Relief: Institutional Politics and the Origins of Modern American Social Policy. Princeton, NJ: Princeton University Press; 1998. [Google Scholar]
- Amenta Edwin, Bonastia Chris, Caren Neal. U.S. Social Policy in Comparative and Historical Perspective: Concepts, Images, Arguments, and Research Strategies. Annual Review of Sociology. 2001;27:213–34. [Google Scholar]
- Amenta Edwin, Poulsen Jane D. Social Politics in Context: The Institutional Politics Theory and Social Spending at the End of the New Deal. Social Forces. 1996;75:33–61. [Google Scholar]
- Barry Colleen L, Huskamp Haiden A, Goldman Howard H. A Political History of Federal Mental Health and Addiction Insurance Parity. Milbank Quarterly. 2010;88:404–33. doi: 10.1111/j.1468-0009.2010.00605.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behrens Angela, Uggen Christopher, Manza Jeff. Ballot Manipulation and the ‘Menace of Negro Domination’: Racial Threat and Felon Disenfranchisement in the United States, 1850–2002. American Journal of Sociology. 2003;109:559–605. [Google Scholar]
- Berry Frances Stokes, Berry William D. State Lottery Adoptions as Policy Innovations: An Event History Analysis. American Political Science Review. 1990;84:395–415. [Google Scholar]
- Berry William D, Ringquist Evan J, Fording Richard C, Hanson Russell L. Measuring Citizen and Government Ideology in the American States, 1960–93. American Journal of Political Science. 1998;42:327–48. [Google Scholar]
- Box-Steffensmeier Janet M, Jones Bradford S. Analytical Methods for Social Research Series. Cambridge, UK: Cambridge University Press; 2004. Event History Modeling: A Guide for Social Scientists. [Google Scholar]
- Buchmueller Thomas C, Cooper Philip F, Jacobson Mireille, Zuvekas Samuel H. Parity for Whom? Exemptions and the Extent of State Mental Health Parity Legislation. Health Affairs. 2007;26:w483–87. doi: 10.1377/hlthaff.26.4.w483. [DOI] [PubMed] [Google Scholar]
- Buck Jeffrey A, Teich Judith L, Umland Beth, Stein Mitchell. Behavioral Health Benefits in Employer-sponsored Health Plans, 1997. Health Affairs. 1999;18:67–78. doi: 10.1377/hlthaff.18.2.67. [DOI] [PubMed] [Google Scholar]
- Bush George. Presidential Proclamation 6158. U.S. Senate and U.S. House of Representatives Joint Resolution to Designate the Decade Beginning January 1, 1990 as the ‘Decade of the Brain.’. House Joint Resolution 174/Senate Joint Resolution 173, Public Law 101-58 1990 [Google Scholar]
- Caronna Carol A. The Misalignment of Institutional ‘Pillars’: Consequences for the U.S. Health Care Field. Journal of Health and Social Behavior. 2004;45:45–58. [PubMed] [Google Scholar]
- Cubbins Lisa A, Parmer Penelope. Economic Change and Health Benefits: Structural Trends in Employer-based Health Insurance. Journal of Health and Social Behavior. 2002;42:45–63. [PubMed] [Google Scholar]
- Edelman Lauren, Uggen Christopher, Erlanger Howard. The Endogeneity of Legal Regulation: Grievance Procedures as Rational Myth. American Journal of Sociology. 1999;105:406–54. [Google Scholar]
- Edelman Lauren B. Legal Environments and Organizational Governance: The Expansion of Due Process in the American Workplace. American Journal of Sociology. 1990;95:1401–40. [Google Scholar]
- Erikson Robert S, Wright Gerald C, McIver John P. Statehouse Democracy. Cambridge, UK: Cambridge University Press; 1993. [Google Scholar]
- Eyestone Robert. Confusion, Diffusion, and Innovation. American Political Science Review. 1977;71:441–47. [Google Scholar]
- Frank David John, Camp Bayliss J, Boutcher Steven A. Worldwide Trends in the Criminal Regulation of Sex, 1945 to 2005. American Sociological Review. 2010;75:867–93. [Google Scholar]
- Frank Richard G, Koyanagi Chris, McGuire Thomas G. The Politics and Economics of Mental Health ’Parity’ Laws. Health Affairs. 1997;16(4):108–119. doi: 10.1377/hlthaff.16.4.108. [DOI] [PubMed] [Google Scholar]
- Frank Richard G, McGuire Thomas G. Integrating People with Mental Illness into Health Insurance and Social Services. In: Mechanic David, Rogut Lynn B, Cohen David C, Knickman James R., editors. Policy Challenges in Modern Health Care. New Brunswick, NJ: Rutgers University Press; 2005. pp. 223–37. [Google Scholar]
- Gitterman Daniel P, Sturm Roland, Scheffler Richard M. Toward Full Mental Health Policy and Beyond. Health Affairs. 2001;20:68–76. doi: 10.1377/hlthaff.20.4.68. [DOI] [PubMed] [Google Scholar]
- Goffman Erving. Stigma: Notes on the Management of Spoiled Identity. Englewood Cliffs, NJ: Prentice Hall; 1963. [Google Scholar]
- Goldman William, McCulloch Joyce, Sturm Roland. Costs and Use of Mental Health Services before and after Managed Care. Health Affairs. 1998;17(2):40–52. doi: 10.1377/hlthaff.17.2.40. [DOI] [PubMed] [Google Scholar]
- Grattet Ryken, Jenness Valerie, Curry Theodore R. The Homogenization and Differentiation of Hate Crime Law in the United States, 1978 to 1995: Innovation and Diffusion in the Criminalization of Bigotry. American Sociological Review. 1998;63:286–307. [Google Scholar]
- Hausman Ken. Plane Crash Takes Life of Congressional Ally. Psychiatric News. 2002;37:1. [Google Scholar]
- Hill Herbert. Black Labor and the American Legal System. Madison: University of Wisconsin Press; 1986. [Google Scholar]
- Imershein Allen, Rond Philip, Mathis Mary. Restructuring Patterns of Elite Dominance and the Formation of State Policy in Health Care. American Journal of Sociology. 1992;97:970–93. [Google Scholar]
- Jacobs Lawrence R, Skocpol Theda. Health Care Reform and American Politics: What Everyone Needs to Know. New York: Oxford University Press; 2010. [Google Scholar]
- Jenkins J Craig, Shumate Teri. Cowboy Capitalists and the Rise of the ‘New Right’: An Analysis of Contributors to Conservative Policy Formation Organizations. Social Problems. 1985;33:130–45. [Google Scholar]
- Jenness Valerie. Managing Difference and Making Legislation: Social Movements and the Racialization, Sexualization, and Gendering of Federal Hate Crime Law in the U.S. 1985–1998. Social Problems. 1999;46:548–71. [Google Scholar]
- Joint Commission on Mental Illness and Health. Action for Mental Health. New York: Basic Books; 1961. [Google Scholar]
- Kershaw Sarah. The Murky Politics of Mind-body. The New York Times. 2008 Mar 30;:1. Section WK. [Google Scholar]
- Light Donald W. Historical and Comparative Reflections on the U.S. National Health Insurance Reforms. Social Science and Medicine. 2011;72:129–32. doi: 10.1016/j.socscimed.2010.10.015. [DOI] [PubMed] [Google Scholar]
- Link Bruce G, Phelan Jo C, Bresnahan Michaeline, Stueve Ann, Pescosolido Bernice. Public Conceptions of Mental Illness: Labels, Causes, Dangerousness, and Social Distance. American Journal of Public Health. 1999;89:1328–33. doi: 10.2105/ajph.89.9.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin Jack K, Pescosolido Bernice A, Tuch Steven A. Of Fear and Loathing: The Role of ‘Disturbing Behavior,’ Labels, and Causal Attributions in Shaping Public Attitudes Toward People with Mental Illness. Journal of Health and Social Behavior. 2000;41:208–23. [Google Scholar]
- McCammon Holly J, Campbell Karen E, Granberg Ellen M, Mowery Christine. How Movements Win: Gendered Opportunity Structures and U.S. Woman’s Suffrage Movements, 1866 to 1919. American Sociological Review. 2001;66:49–70. [Google Scholar]
- McKinlay John B, Marceau Lisa D. The End of the Golden Age of Doctoring. In: Conrad Peter., editor. The Sociology of Health and Illness: Critical Perspectives. 7. New York: Worth; 2005. pp. 189–214. [Google Scholar]
- McSween Jean L. The Role of Group Interest, Identity, and Stigma in Determining Mental Health Policy Preferences. Journal of Health Politics, Policy and Law. 2002;27:773–800. doi: 10.1215/03616878-27-5-773. [DOI] [PubMed] [Google Scholar]
- Mechanic David. The Managed Care Backlash: Perceptions and Rhetoric in Health Care Policy and the Potential for Health Care Reform. Millbank Quarterly. 2001;79:35–54. doi: 10.1111/1468-0009.00195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechanic David. Policy Challenges in Improving Mental Health Services: Some Lessons from the Past. Psychiatric Services. 2003;54:1227–32. doi: 10.1176/appi.ps.54.9.1227. [DOI] [PubMed] [Google Scholar]
- Mechanic David. The Rise and Fall of Managed Care. Journal of Health and Social Behavior. 2004;45:76–86. [PubMed] [Google Scholar]
- Mechanic David, McAlpine Donna D. Mission Unfulfilled: Potholes on the Road to Mental Health Parity. Health Affairs. 1999;18:7–21. doi: 10.1377/hlthaff.18.5.7. [DOI] [PubMed] [Google Scholar]
- Mechanic David, Rochefort David A. Deinstitutionalization: An Appraisal of Reform. Annual Review of Sociology. 1990;16:301–27. [Google Scholar]
- Mintz Beth. Business Participation in Health Care Policy Reform: Factors Contributing to Collective Action within the Business Community. Social Problems. 1995;42:408–28. [Google Scholar]
- Mintz Beth, Palmer Donald. Business and Health Care Policy Reform in the 1980s: The 50 States. Social Problems. 2000;47:327–59. [PubMed] [Google Scholar]
- Newhouse Joseph P. Free for All? Lessons from the RAND Health Insurance Experiment. Cambridge, MA: Harvard University Press; 1993. [Google Scholar]
- Otten Alan L. Mental Health Parity: What Can It Accomplish in a Market Dominated by Managed Care? New York: Milbank Memorial Fund; 1998. [Google Scholar]
- Pavalko Eliza K. State Timing of Policy Adoption: The Case of Workmen’s Compensation in the United States, 1909–1929. American Journal of Sociology. 1989;95:592–615. [Google Scholar]
- Quadagno Jill. One Nation Uninsured: Why the US Has No National Health Insurance. New York: Oxford University Press; 2005. [Google Scholar]
- Quadagno Jill, Meyer Madonna Harrington. Organized Labor, State Structures, and Social Policy Development: A Case Study of Old Age Assistance in Ohio. Social Problems. 1989;36:181–96. [Google Scholar]
- Scheff Thomas J. The Societal Reaction to Deviance: Ascriptive Elements in the Psychiatric Screening of Mental Patients in a Midwestern State. Social Problems. 1964;11:401–13. [Google Scholar]
- Shi Leiyu, Singh Douglas A. Delivering Health Care in America. 2. Gaithersburg, MD: Aspen; 2001. [Google Scholar]
- Shipan Charles R, Volden Craig. Bottom-up Federalism: The Diffusion of Antismoking Policies from U.S. Cities to States. American Journal of Political Science. 2006;50:825–43. [Google Scholar]
- Skocpol Theda, Abend-Wein Marjorie, Howard Christopher, Lehmann Susan Goodrich. Women’s Associations and the Enactment of Mothers’ Pensions in the United States. American Political Science Review. 1993;87:686–701. [Google Scholar]
- Starr Paul. Remedy and Reaction: The Peculiar American Struggle over Health Care Reform. New Haven, CT: Yale; 2011. [Google Scholar]
- Sturm Roland. How Expensive is Unlimited Mental Health Care Coverage under Managed Care? JAMA. 1997;278:1522–37. [PubMed] [Google Scholar]
- Sturm Roland, Pacula Rosalie Liccardo. State Mental Health Parity Laws: Cause or Consequence of Differences in Use? Health Affairs. 1999;18:182–92. doi: 10.1377/hlthaff.18.5.182. [DOI] [PubMed] [Google Scholar]
- Sturm Roland, Zhang Weiying, Schoenbaum Michael. How Expensive Are Unlimited Substance Abuse Benefits under Managed Care? Journal of Behavioral Health Services and Research. 1999;26:203–10. doi: 10.1007/BF02287491. [DOI] [PubMed] [Google Scholar]
- Tausig Mark, Michello Janet, Subedi Sree. A Sociology of Mental Illness. Upper Saddle River, NJ: Prentice Hall; 1999. [Google Scholar]
- Tovino Stacey A. Reforming State Mental Health Parity Law. Houston Journal of Health Law & Policy. 2011;11:455–504. [Google Scholar]
- Trice Harrison M, Roman Paul M. Delabeling, Relabeling, and Alcoholics Anonymous. Social Problems. 1971;17:538–46. [Google Scholar]
- U.S. Department of Health and Human Services. Medical Expenditure Panel Survey. Tables of Private-sector Data by Firm Size and State. Washington, DC: U.S. Government Printing Office; 1996. [Google Scholar]
- U.S. Government Accountability Office. “Mental Health Parity Act: Despite New Federal Standards, Mental Health Benefits Remain Limited.” GAO Report HEHS-00-95. Washington, DC: U.S. Government Accountability Office; 2000. [Google Scholar]
- U.S. Government Printing Office. Departments of Veterans Affairs and Housing and Urban Development, and Independent Agencies Appropriations Act, 1997. Public Law 104–204. 1996 Retrieved November 11, 2010 ( http://www.gpo.gov/fdsys/pkg/PLAW-104publ204/pdf/PLAW-104publ204.pdf)
- Walker Jack L. The Diffusion of Innovations among the American States. American Political Science Review. 1969;63:880–99. [Google Scholar]
- Wood Elijah Patton. Policy Matters: Critical Issues in Health Care Access. Washington, DC: National Conference of State Legislatures; 2005. Children and Mental Health Parity. [Google Scholar]
- Wolff Nancy. Risk, Response, and Mental Health Policy: Learning from the Experience of the United Kingdom. Journal of Health Politics, Policy and Law. 2002;27:801–32. doi: 10.1215/03616878-27-5-801. [DOI] [PubMed] [Google Scholar]
- Wright Gerald C, Erikson Robert S, McIver John P. Public Opinion and Policy Liberalism in the United States. American Journal of Political Science. 1987;31:980–1001. [Google Scholar]
- Yamaguchi Kazuo. Event History Analysis. Newbury Park, CA: Sage; 1991. [Google Scholar]