Abstract
National efforts have focused on improving adolescent substance use disorder (SUD) treatment outcomes, yet improvements remain modest. Because adolescents are noteworthy for heterogeneity in their clinical profiles, treatment might be enhanced by the identification of clinical subgroups for which interventions could be more effectively tailored. Some of these subgroups, such as those based on abstinence motivation, substance involvement, and psychiatric status are promising candidates. This study examined the unique predictive utility of adolescents’ primary reason for alcohol and other drug use. Adolescent outpatients (N=109; 27% female, aged 14–19) were assessed at treatment intake on their reason for substance use, as well as demographic, substance use, and clinical variables, and re-assessed at 3, 6, and 12 months. Reason for use fell into two broad domains: using to enhance a positive state (positive reinforcement [PR]; 47% of youth) and using to cope with a negative state (negative reinforcement [NR] 53% of youth). Compared to PR patients, NR patients were significantly more substance-involved, reported more psychological distress, and had a more extensive treatment history. Importantly, NR patients showed a significant treatment response whereas PR patients showed no improvement. PR/NR status also uniquely predicted treatment response and outcome independent of a variety of other predictors including abstinence motivation, self-efficacy, coping, and prior treatment. Adolescents’ primary reason for substance use may provide unique clinical information that could inform treatment planning and patient-treatment matching.
Keywords: Adolescents, Addiction treatment, Substance use disorder, phenotype, reasons for substance use
Adolescents’ misuse of drugs and alcohol has been recognized as a top public health problem in the United States (The National Center on Addiction and Substance Abuse [CASA] at Columbia, 2011). While not all adolescents who use alcohol or drugs will go on to have long-term problems, the significant risks associated with alcohol and other drug use during this developmental period warrants early intervention. For the more substance-involved adolescents that receive formal treatment services, relapses are common (Brown & Ramo, 2006; Ramo and Brown, 2008; Kaminer, Burleson, & Burke, 2008; Sussman, Skara, Ames, 2008) and those who resume use following treatment appear to be at increased risk of returning to pretreatment levels of use within six to twelve months (Burleson, Kaminer, & Burke, 2012; Godley, Godley, Dennis, Funk, & Passetti, 2007). Recent clinical efforts have been focused on improving the quality and effectiveness of adolescent outpatient treatment and expanding continuing care efforts, yet outcome improvements have been modest (Kelly & White, 2010; Knudsen, Ducharme, Roman, & Johnson, 2008; Sussman et al., 2008).
One major treatment challenge among youth samples is that adolescents with substance use disorder (SUD) are noteworthy for heterogeneity in their clinical profiles, particularly regarding problem recognition and motivation for abstinence (Kuntsche, Knibbe, Engels, & Gmel, 2010; Tims, Dennis, Hamilton, Buchan, & Diamond, 2002; Titus, Godley, & White, 2007). Consequently, commonly used skills-based group interventions may not address the needs of many young people enrolled in treatment, as they focus on skill-building when many have no intention or desire to use the skills. As such, treatment engagement and outcomes might be enhanced by the identification of homogeneous clinical subgroups for which interventions could be more efficiently tailored (Goodman, Perterson-Badali, & Henderson, 2011
Predictors of treatment response
Multiple research studies have identified a number of objective and subjective individual factors that predict treatment response and are related to substance use outcomes and relapse (Anderson, Ramo, & Brown, 2006; Ramo and Brown, 2008; Chung & Maisto, 2006; Kelly, Dow, Yeterian, Kahler, 2010; Sussman et al., 2008; Wei, Heckman, Gay, & Weeks, 2011). Some objective predictors have included prior treatment experiences, criminal justice system involvement, and psychiatric comorbidity; subjective factors have included perceived substance involvement and impairment, motivation for abstinence, self-efficacy, and coping skills (Anderson et al., 2006; Dennis, Scott, Funk, & Foss, 2005, Godley, et al., 2007; Kelly et al, 2010; Sussman et al., 2008). Importantly, just as adolescents entering treatment have varying levels of motivation for abstinence, coping skills, and abstinence self-efficacy, as well as unique substance use histories, they may also report different reasons for their substance use. Such reasons are often a focus of functional analysis which forms the basis of most cognitive-behavioral therapies for SUD (Godley et al., 2001; Webb, Scudder, Kaminer, Kadden, 2002), but such reasons have seldom been examined as potential predictors of treatment response and outcome.
Reason for substance use
According to the National Institute of Drug Abuse (NIDA) there are four main reasons why people misuse substances: 1) to feel good, 2) to feel better, 3) to do better, and 4) out of curiosity or because others are doing it (NIDA, 2008). The predominant reason why adolescents report using alcohol or other drugs may have important clinical implications. Thus far, the research on this construct has identified taxonomies and correlations of reason for use (Cooper et al, 1995; Kuntsche et al., 2010; Titus et al., 2006), how reasons for use may change over the life course (Patrick et al, 2011a) and predict later problems (Patrick et al, 2011b) and relapse precursors (Ramo and Brown, 2008), but has not examined how reasons for use relate to treatment outcomes. Kuntsche and colleagues (2010) examined alcohol use motives among high-risk adolescents, from which two broad groups emerged: “enhancement drinkers” and “coping drinkers”. Characteristics of “enhancement drinkers” denoted use for positive reinforcement, including drinking to get high or because they liked it, whereas characteristics of “coping drinkers” denoted use for negative reinforcement, including in order to forget problems or when experiencing negative affect, such as depression or anxiety. Similarly, in earlier work based on this type of affect regulation paradigm wherein alcohol is used to modulate emotional experience, Cooper and colleagues (1995) tested multivariable models in two general population samples (one adolescent and one adult) to examine the antecedents and consequences of negative reinforcement drinking (i.e., to cope) versus positive reinforcement drinking (i.e., to enhance a positive state). They found that negative, but not positive, reinforcement drinking was associated with drinking problems. A longitudinal study by Patrick and colleagues (Patrick et al, 2011b) found that both positive and negative reasons for use at age 18 predicted use at age 35, but that negative (coping motives) were more related to heavier use and alcohol use disorder symptoms at age 35. Building on this research, the current study used a similar framework to categorize reasons for alcohol as well as other drug use in an adolescent clinical sample in order to examine whether such a distinction has clinical utility in treatment populations.
Reasons for use as a marker of addiction stage or phenotype
These two broad domains of reasons for substance use (i.e., positive and negative reinforcement) also map on to Koob’s theoretical model of the addiction cycle (Koob, 2004). This model proposes that addiction has aspects of impulse control difficulties (e.g. tension/arousal leading to impulsive acts leading to pleasure or gratification and guilt) and compulsive disorders (e.g. to alleviate anxiety/stress leading to cognitive preoccupation and compulsive use). Koob (2004) posits that the natural progression of addiction is marked by the shift from the impulsive (i.e. positive reinforcement) to the compulsive (i.e. negative reinforcement). As such, if reasons for use fall into categories of positive and negative reinforcement, it could provide support for these different stages of the addiction process. Alternatively, such categories of reasons for use may represent stable phenotypes of the disorder. Thus, adolescents’ reasons for using substances may potentially reflect two qualitatively different constructs: 1) the stages in the substance use disorder cycle or 2) specific substance use disorder phenotypes. In either case, practitioners would be able to identify different subgroups that may have clinical matching utility.
Some prior research has explored reasons why individuals use substances, but no research to date has examined how adolescents’ predominant reason for substance use influences treatment response and outcomes. Whether an adolescent is using broadly for positive reinforcement (PR; e.g., “to feel good”) or for negative reinforcement (NR; e.g., “to feel better” by reducing negative affect) reasons may play an important role in treatment planning, similar to that of other variables, such as the degree of recovery motivation, abstinence self-efficacy, and abstinence focused coping skills youth may report at treatment entry. If an individual’s primary reason for use relates to treatment response and outcome and adds unique predictive information to an individual’s clinical profile beyond that of already identified predictors, then obtaining the reason could have clinical utility and help tailor treatments more efficiently and effectively (Engel and MacGowan, 2009).
Study Aims
The purpose of the current study is to examine whether adolescents’ reasons for using substances can help discriminate subgroups of youth that may respond differentially to SUD outpatient treatment and to examine whether knowledge of this variable adds independent, clinically useful, information regarding adolescents’ treatment outcomes. To this end, our specific aims were threefold: 1) to identify homogeneous subgroups of patients with similar predominant reasons for alcohol/drug use; 2) to examine whether, and in what ways, these subgroups (based on their predominant reason for use) differ systematically on demographic, prior treatment, and other clinical and outcome variables; and, 3) to test whether knowledge of this sub-grouping variable provides unique clinical information in predicting treatment response and longer-term outcome post discharge.
Method
Participants
Of the 178 adolescents who presented for treatment during the enrollment period, 160 (90%) were eligible to participate. Of these, 95% (n = 152) agreed to be contacted by study staff and 127 (79.4%) enrolled (see Kelly & Urbanoski, 2012 for more details). In order to be included in the study sample, participants had to have valid data for the target variable (i.e., reason for use). If the participant gave an ambiguous response (n = 8) or if no response was given (n = 10), the participant was not included in the final study sample (n = 18). Consequently, participants in the current analysis were 109 adolescents taken from the initial sample of 127 adolescents. The study sample was 75.2% male, 87.2% White, and was on average 16.6 years (SD = 1.2; range 14–19) old at the time of study entry, and was generally representative of the sample from which it was drawn. At baseline, most participants were living at home with at least one parent (93.5%), enrolled in school (75.2%), not employed (55.9%), and justice system involved (51.4%). Of those who were not currently in school (n = 39), 41.0% were not in school for an alcohol/drug-related reason.
Seventy percent of participants reported that drugs (including marijuana) were the major substance that caused them to enter the current treatment program, while 16% reported alcohol, and 14% reported both drugs and alcohol. The majority of participants reported entering the current treatment program either because their parent(s) wanted them to (41.3%), court/probation officer required it (23.0%), or treatment provider (e.g., therapist, inpatient facility) recommended it (26.6%); the remaining 9.1% reporting other reasons. Marijuana was the most commonly reported drug of choice at baseline (70.6%), followed by alcohol (10.1%), narcotics (10.1%), cocaine/amphetamines (4.2%), sedatives (3.2%), and hallucinogens (1.8%).
Treatment Facility and Representativeness
Participants were recruited from a private, for-profit SUD treatment facility in the Northeastern U.S. Patients in the program were expected to complete a 12 week/90 day tenure with a requirement to attend at least one group session per week of 90 minutes duration. A minority also received some individual sessions. Most (71%) completed 12 weeks of treatment; 21% completed 8 or fewer weeks of treatment. The mean number of sessions attended during outpatient treatment was 11.5 (SD = 6.2; Median = 11; range 0–44). Treatment was abstinence-focused and based on an eclectic model that combines cognitive-behavior therapy (CBT), motivational enhancement therapy (MET), and 12-Step approaches. One clinical director also completed the Drug and Alcohol Program Treatment Inventory (DAPTI; Swindle, Peterson, Paradise, & Moos, 1995), an 80-item survey designed to assess the goals and activities of SUD treatment programs within eight theoretical orientations (e.g., 12-Step, Cognitive-Behavioral) based on program goals and activities. This program scored the highest on Cognitive-Behavioral orientation (17/24), and the lowest on 12-Step orientation (1/24).
The current facility appears nationally representative of the majority of adolescent SUD treatment organizations in terms of the level of care (standard outpatient), mode of treatment (group, individual, and family therapy), theoretical model (mixed/eclectic), intensity of service delivery (1–2 groups per week), and continuing care approaches (Knudsen et al., 2008). For additional details, please see Kelly et al. (2010).
Measures
Prior treatment
At intake, data regarding prior treatment were collected using the Background Information Form (BIF; Brown, Vik, & Creamer, 1989). Participants were asked about their prior lifetime history of SUD treatment, including inpatient/residential programs (whether or not they had been in an inpatient or residential program), outpatient programs (total length in weeks), and individual sessions with a mental health professional (number of sessions).
Lifetime substance use and disorders
At intake, a modified version of the Customary Drinking and Drug Use Record (CDDR; Brown et al, 1998) was used. This assessed DSM-IV SUD criteria, lifetime substance use history, including age at first use, age at first regular use, and total number of times used, for alcohol, nicotine, marijuana, hallucinogens, cocaine/crack, amphetamines/methamphetamine, barbiturates, sedatives/tranquilizers, heroin and other opiates, steroids, inhalants, and other drugs. The vast majority of the current sample (93.6%) met past year criteria for an SUD (71% for dependence on at least one substance) with 25.7% meeting criteria for marijuana abuse (without dependence), 58.7% for marijuana dependence, 27.5% for alcohol abuse (without dependence), 30.3% for alcohol dependence, 2.8% for opiate abuse (without dependence), and 11.9% for opiate dependence. The original CDDR has been shown to have good internal consistency, test-retest and inter-rater reliability, as well as convergent and discriminant validity with adolescent inpatients (Brown et al., 1998).
Psychiatric co-morbidity and clinical symptoms
At intake, participants completed the Computerized Diagnostic Interview Schedule for Children, version IV (C-DISC-IV; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000). The C-DISC-IV measured the presence of ten Axis-I diagnoses over the past year, including: social phobia, panic disorder, agoraphobia, obsessive compulsive disorder, eating disorders, major depression, mania, attention deficit/hyperactivity, oppositional defiant disorder, and conduct disorder. Approximately 63.3% of the current sample met DSM-IV criteria for one or more conditions, with the most common being conduct disorder (44.4%), major depressive episode (18.3%), oppositional defiant disorder (19.4%), and attention deficit hyperactivity disorder (11.1%).
Youth also completed the Brief Symptom Inventory (BSI; Derogatis & Melisaratos, 1983) a 53-item measure of past week psychological symptoms across nine subscales with response options for each item ranging from 0 (“Not at all”) to 4 (“Extremely”). For the purposes of this study, the Global Severity Index (GSI) was used. Internal consistency in the current sample was high (Cronbach’s α = .93).
Past 90-day substance use and criminal justice system involvement
At all time points, the psychometrically validated Timeline Follow-Back (TLFB; Sobell & Sobell, 1992; Dennis, Funk, Godley et al, 2004) and Form-90 (Miller & Del Boca, 1994; Scheurich, Muller, Anghelescu et al, 2005) were used in conjunction to examine substance use and treatment experiences in the past 90 days, including AA/NA attendance. Participants also used the calendar to assist with estimates of substance use frequency and timing. From these measures, percent days abstinent (PDA) was calculated by dividing the number of days of no alcohol/drug use (excluding nicotine) by the total number of days in the time period and multiplying by 100.
Substance use problem severity during the past 90 days was measured using the Personal involvement scale (PIS) taken from the Personal Experiences Inventory (PEI; Winters & Kenly, 1989). Possible responses to each of the 29 substance problems ranged from 0 (“Never”) to 3 (“Often”). Internal consistency of this 29-item measure in the current sample was high (Cronbach’s α = .94). Substance-related consequences in the past 90 days were measured using the 50-item Inventory of Drug Use Consequences (InDUC-2R; Tonigan & Miller, 2002). Possible responses for each item ranged from 0 (“never”) to 3 (“Daily or almost daily”). Internal consistency for the total score used in the current sample was high (Cronbach’s α= .96).
At intake, participants were also asked if they were currently involved in the criminal justice system during the past year. Responses included 1) no; 2) yes, awaiting a court hearing; 3) yes, on probation; 4) yes, on parole, and 5) yes, other. These were subsequently dichotomized in to two categories: no (coded 0) or yes (coded 1).
Abstinence motivation, abstinence self-efficacy, and abstinence-focused coping
Abstinence motivation: At intake, participants were asked to separately rate the importance of not drinking alcohol or using drugs over the next 90 days on a 10-point scale ranging from 1 (not at all important) to 10 (very important). Abstinence self-efficacy: participants were asked to separately rate the likelihood that they would stop drinking alcohol or stop using drugs in the next 90 days on a 10-point scale ranging from 1 (definitely won’t stop) to 10 (stop for sure). Coping was assessed with the Adolescent Relapse Coping Questionnaire (ARCQ; Myers & Brown, 1990), a 27-item self-report measure that assesses coping responses to high-risk relapse situations for adolescents (e.g. offered substances by a peer) with possible response options ranging from 1 (“Definitely would not think or do”) to 7 (“Definitely would think or do”) Abstinence-focused coping was assessed using the abstinence-focused coping subscale from this measure, which possessed high internal consistency for this sample (Cronbach’s α =.85).
Biological verification of self-report
Biological verification of self-reported abstinence was conducted using Intercept Oral Fluid Drug Test kits, which test saliva for the presence of seven substances (amphetamines, methamphetamines/MDMA, benzodiazepines, cannabinoids, cocaine, opiates, and phencyclidine) using an Oral 7 Panel screen. Saliva samples were analyzed independently at Kroll Laboratory Specialists, Inc. At follow-up assessments, if youth reported abstinence from substances (excluding alcohol and nicotine) in the past 3 months, they were asked to provide a saliva sample. At any timepoint, only one individual had a saliva test positive for drugs that was inconsistent with a self-report of abstinence. This occurred at the 6 month follow up and this datum for this case was removed from the analyses.
Reasons for use
At intake, the Background Information Form (BIF; Brown et al., 1989) was used to ask adolescents if they thought they had a problem with alcohol or drugs (separately). If participants reported having either an alcohol or drug problem (n = 69), they were asked “what would you say is the major reason for your drinking/drug problem.” If participants reported not having a problem (n = 40), they were asked “what would you say is the major reason for your drinking/drug use.” Responses were placed into one of the eight available response options by the research interviewers. These included: “enhanced positive state (e.g. get high/stoned for pleasure)”, “boredom”, “peer pressure”, “habit”, “family problems”, “school problems”, “stress/personal problems”, and “family history of drug/alcohol abuse”. Using to enhance a positive state (e.g. get high/stoned for pleasure) was coded as using for “positive reinforcement” (the PR group; coded 0) and all other responses except for a family history of drug/alcohol use disorder were coded as using for negative reinforcement (NR; coded 1). No participants reported a family history of substance use as a reason. There was also an “other” category where patients could state another reason for use not on the checklist. This occurred in eight cases. This was recorded verbatim and then coded into one of the categories (i.e., PR or NR) for the purposes of the current study. Three raters independently categorized all seven of the original checklist items above as well as the eight open-ended item responses into the PR/NR sub-categories. Fleiss Kappa statistics were computed (which correct for chance agreement) given the categorical nature of the data and having more than two raters (three in this study). There was a high rate of concordance among raters (Fleiss Kappa = .73; “substantial reliability”; Landis and Koch, 1977).
Participants were allowed to report multiple responses, however, if a youth reported both a PR and an NR reason they were excluded from this analysis (n=10; resulting in a total sample for the current study of 109. These 10 were not shown to be different from the remaining sample on demographic or clinical variables; ps>.13). As noted in the results below, some youth reported more than one NR reason (but this would not alter their NR grouping status)
Procedure
Participants completed the baseline assessment at the treatment facility or at the study staff’s office as close as possible to their treatment start date, followed by a 3, 6, and 12-month follow-up assessment 90, 180, and 360 days after their treatment start date, respectively. On average, participants completed their baseline assessment within 10.6 days (SD = 12.4) of their due date, the 3-month assessment within 7.3 days (SD = 7.8), the 6-month within 8.8 days (SD = 8.1), and 12-month within 12.1 days (SD = 15.9) of the due date. Follow-up rates were 91.3% at 3 months, 84.3% at 6 months, and 87.4% at 12 months. For full procedure details, please refer to Kelly et al. (2010).
Participants were paid by check at the end of each assessment: $50 for both the baseline and 12-month assessments and $40 for both the 3- and 6-month assessments. Participants who completed only part of an assessment received partial payment for the portion that they completed.
Missing data
Although completely missing assessment time points was infrequent, we ran a longitudinal binary Generalized Estimating Equation (GEE) model, where the dependent variable was missing (vs. not) at each time point to find any systematic relationships between intake variables and subsequent missing data. Using demographic indicators and treatment, psychiatric, and severity indicators (16 in all), we found no significant baseline predictors (probably given the small number missing limiting power) other than time, indicating an increasing trend for being missing over time. There were 7, 10, and 15 missing PDA assessments at the 3m, 6m, and 12m, interview, respectively. PR/NR status was not associated with missing any of the follow ups.
In terms of missing individual items on particular scales, if more than 50% of items were missing for a participant on a given scale, no score was computed and was coded as missing. On the ARCQ Abstinence-focused coping scale, this occurred for 2–5% of the sample across subscales. On the BSI-GSI scale, this occurred for 2% of the sample. When less than 50% of items were missing, a weighted mean scale score was used (e.g., if 9 out 10 items were available on a scale, the average of the 9 items was used instead of 10). On the ARCQ Abstinence-focused coping scale, this occurred for between 2–6 % of individuals across subscales. On the BIS-GSI, this did not occur. There were no other missing data. All scaled scores used in the current analyses were completed at baseline only and are not impacted by attrition.
Data Analysis Plan
The data analysis plan consisted of two main steps. 1) Distribution and comparison of PR/NR status, and 2) PR/NR status in relation to outcome and its unique ability to predict outcome.
1) Distribution and comparison of PR/NR status
We first examined the proportion of patients that reported using predominantly for positive (PR) versus negative reinforcing (NR) reasons and then compared these groups on demographic, clinical, and substance use variables. We then computed bivariate correlations to test for significant associations between PR/NR status and demographic, clinical, and substance use variables, including whether or not the reason for use was related to the main outcome variable (i.e. PDA; percent days abstinent) at each of the four assessment time points (0m, 3m, 6m, 12m). We ran Pearson and Spearman correlations to assess for possible skew amongst variables. The magnitude and significance of the variables using the two correlational approaches did not differ, thus we report the Spearman coefficients.
2) PR/NR status in relation to outcome and PR/NR status’ unique ability to predict outcome
First, we computed descriptive statistics comparing the PR and NR groups on PDA outcomes as well as between-subjects and auto-correlation adjusted within-person Cohen’s d to estimate standardized effect sizes. PDA at 3-, 6-, and 12-month follow-ups was normally distributed and did not require transformation. Next, in order to control for other treatment outcome predictors in order to examine the unique effects of PR/NR group status on PDA over time, we screened for significant predictor variables using correlational analyses (e.g., demographics, prior treatment, motivation for abstinence). Significant predictors of outcome were then controlled in the outcome analyses.
Finally, in order to test for the effect of PR/NR group status differences on PDA, we fitted polynomial time trends across follow-ups with SAS Proc MIXED, where PDA was the dependent variable, and month (with values 0, 3, 6, and 12) and group membership (PR/NR status) were the independent variables. We considered both linear and quadratic trends, because we expected to see an immediate positive and then decaying treatment effect on PDA and employed an unstructured covariance model. To test whether or not group membership was a unique predictor independent of other factors typically related to PDA, we fitted the same model, but this time included factors that predicted PDA over time as covariates.
Results
Distribution and Comparison of PR/NR Status
Participants were allowed to endorse more than one reason for their substance use. Most participants (81.7%) only gave one response, 15.6% gave 2 responses, and 2.7% gave 3 or 4 responses. If someone reported more than one reason that fell into both categories they were excluded from the current analyses (N=10). The reasons reported for drinking and using drugs were enhanced positive state (48.3%), stress/personal problems (24.2 %), boredom (9.2%), peer pressure (3.3%), habit (5.0%), family problems (3.3%), and other responses (6.7%). Examples of “other” responses include: “hard to turn down (NR)”, “not to escape problems (PR)”, “common place in private school (not included)”, and “helps eliminate stutter (NR).” Of the 109 participants included in the analysis, 46.8% were coded as using for positive reinforcement (PR) and 53.2% were coded as using for negative reinforcement (NR).
Comparison of PR/NR Status in relation to baseline variables
Comparative analyses of the two groups on baseline characteristics revealed there were no significant differences at intake between the PR and NR groups for age, gender, ethnicity, school enrollment, the presence of any Axis I diagnosis, motivation for abstinence, lifetime 12-step attendance, prior outpatient treatment, or the diagnosis of an externalizing disorder (ps> .08). However, as shown in Table 1, the NR group had a greater number of comorbid Axis I disorders than the PR group. Also, the NR group was more likely than PR group to meet for diagnostic criteria for an internalizing Axis I disorder, and reported a significantly greater amount of psychiatric distress as measured by the GSI scale from the BSI. Additionally, those in the NR group were more likely to report they thought they had a problem with alcohol/drugs, had a higher degree of substance use problems and consequences, more prior inpatient and SUD individual treatment sessions and prior 90-day 12-step meeting attendance, and had higher abstinence self-efficacy and coping.
Table 1.
Baseline clinical and substance-related variables across positive (PR) and negative reinforcement (NR) groups and tests of association
| Domain | Variable | Total (N = 109) | PR (n = 51) | NR (n = 58) | Test between PR and NR | p |
|---|---|---|---|---|---|---|
| Clinical | Any axis I diagnosis | 63 % | 41 % | 59 % | χ2 = 2.91 | .090 |
| Any Internalizing diagnosis | 38 % | 22 % | 73 % | χ2 = 10.52 | .000 | |
| Any Externalizing diagnosis | 52 % | 42 % | 58 % | χ2 = 1.05 | .310 | |
| # of Axis I disorders (M, SD) | 1.32 (1.59) | 0.84 (0.99) | 1.86 (1.87) | F=12.17 | .000 | |
| Global Severity Index (GSI) (M, SD) | 1.06 (0.77) | 0.84 (.61) | 1.26 (.84) | F= 8.47 | .004 | |
|
| ||||||
| Clinical SUD-related | PIS (% above threshold) | 52 % | 36 % | 64 % | χ2 = 5.73 | .017 |
| Perceived problem with alcohol/drugs | 63 % | 30 % | 70 % | χ2 = 20.20 | .000 | |
| Substance use consequences | 4.56 (2.80) | 3.89 (2.61) | 5.15 (2.79) | F= 5.66 | .019 | |
|
| ||||||
| SUD Treatment | Prior outpatient treatment | 28 % | 26 % | 31 % | χ2 = .410 | .522 |
| Prior inpatient treatment | 28 % | 12 % | 43 % | χ2 = 13.10 | .000 | |
| Prior SUD professional sessions | 27 % | 16 % | 36 % | χ2 = 5.85 | .013 | |
| Lifetime 12-step attendance | 42 (n=46) | 34 % | 47 % | χ2 = .962 | .327 | |
| Past 90 day 12-step attendance | 28 % | 16 % | 38 % | χ2 = 6.73 | .009 | |
|
| ||||||
| SUD-related process measures | Motivation for abstinence (M, SD) | 6.90 (3.28) | 6.37 (3.40) | 7.42 (3.11) | F= 3.15 | .079 |
| Abstinence self-efficacy (M, SD) | 6.82 (3.26) | 6.08 (3.37) | 7.48 (3.04) | F= 5.22 | .024 | |
| Abstinence-focused coping (M, SD) | 3.14 (1.35) | 2.64(1.22) | 3.57 (1.32) | F= 14.28 | .000 | |
# of Axis I disorders: the number of diagnoses met for out of 8 possible Axis I disorders. Most common Axis I internalizing disorders were major depression, obsessive-and compulsive disorder; most common externalizing were conduct disorder and attention deficit disorder. GSI: a higher number represents greater severity. Substance use consequences: higher number denotes more substance related consequence. Motivation for abstinence and abstinence self-efficacy: higher number denotes greater motivation for abstinence and greater self-efficacy for abstinence. Abstinence-focused coping: higher number denotes greater use of abstinence-focused coping skills. Remaining variables are reported as % yes.
PR/NR status in relation to outcome
Table 2 shows the means and standard deviations of the PR and NR groups across time with the between-subjects standardized effect sizes computed. Between-group differences at 3 and 6-month follow-up were found to be in the medium effect size range whereas between-group differences at 0m and 12m were negligible (Cohen, 1988).
Table 2.
Percent days abstinent at each follow-up time point by PR/NR status and between-group effect sizes estimates (Cohen’s d)
| PR group (M, SD) | NR group (M, SD) | Test | Sig | Cohen’s d | Interpretation of effect size | |
|---|---|---|---|---|---|---|
| 0-month | 43.9 (33.1) | 47.9 (35.9) | t(107)= −.588 | .558 | 0.116 | Negligible |
| 3-month | 47.7 (33.4) | 61.8 (34.9) | t(100)= −2.08 | .040 | 0.413 | Medium |
| 6-month | 40.8 (34.2) | 57.0 (38.4) | t(97)= −2.21 | .029 | 0.446 | Medium |
| 12-month | 43.5 (36.9) | 47.8 (32.6) | t(92)= −.602 | .549 | 0.124 | Negligible |
PR=Positive Reinforcement group; NR=negative reinforcement group; M= mean; SD= standard deviation. Sig= statistical significance level.
In order to test the unique predictive utility of PR/NR status in relation to treatment response and outcome, we examined a number of potential pre-treatment and baseline predictors of PDA using bivariate Spearman Rank order correlation analyses in order to control for these variables in the longitudinal polynomial mixed models. Pretreatment variables examined were: (a) demographics (age, gender, ethnicity), (b) prior treatment and mutual-help experiences (inpatient, outpatient, individual professional therapy sessions, lifetime and past-90 day 12-step attendance), (c) substance use severity (perceived problem with substances; degree of substance involvement and consequences), and psychiatric diagnoses (internalizing and externalizing); and (d) criminal justice involvement status. Baseline variables examined were substance use problem recognition, motivation for abstinence, abstinence self-efficacy, and abstinence-focused coping.
Age, gender, ethnicity, and criminal justice system involvement were unrelated to PDA at any follow-up (ps >.13). Additionally, substance involvement and severity, substance use problem recognition, and the presence of any Axis I diagnosis were unrelated to PDA (ps> .12). In total, seven variables were significantly associated with PDA at follow-up: prior outpatient treatment, prior inpatient treatment, lifetime and past 90-day AA/NA participation, motivation for abstinence, abstinence self-efficacy, and abstinence-focused coping. Table 3 reports the bivariate magnitude and significance level of these associations. Due to a high degree of collinearity between lifetime and past 90 day 12-step attendance at 0m (r=.72), lifetime 12-step attendance was dropped from the final model analyses and past 90 day 12-step attendance was retained as this was a stronger and more consistent predictor of outcome over time. The six significant predictor variables (plus PR/NR group status) were included in the prospective mixed polynomial model.
Table 3.
Spearman’s correlation coefficients of control variables with percent days abstinent during follow-ups (N=109)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Prior outpatient Tx | - | |||||||||||
| 2. Prior inpatient Tx | .414** | - | ||||||||||
| 3. Lifetime 12-step attendance | .491** | .491** | - | |||||||||
| 4. 90-day 12-step attendance | .477** | .522** | .721** | - | ||||||||
| 5. Motivation for abstinence | .102 | .246** | .097 | .227* | - | |||||||
| 6. Abstinence self-efficacy | .216* | .245* | .211* | .331** | .545** | - | ||||||
| 7. Abstinence-focused coping | .215* | .327** | .255** | .306** | .390** | .313** | - | |||||
| 8. PR/NR status | .061 | .347** | .094 | .249** | .173 | .213* | .362** | - | ||||
| 9. PDA 0-month | .263** | .413** | .268** | .501** | .176 | .312** | .230* | .075 | - | |||
| 10. PDA 3-month | .262** | .208* | .280** | .278** | .282** | .378** | .319** | .224* | .446** | - | ||
| 11. PDA 6-month | .131 | .186 | .161 | .200* | .160 | .220* | .220* | .212* | .33** | .686** | - | |
| 12. PDA 12-month | .127 | .078 | .087 | .232* | −.041 | .033 | .074 | .070 | .238* | .379** | .647** | - |
p < .05
p < .01; PDA = Percent days abstinent from any substance; 12-step attendance = 0 (no) and 1 (yes); Motivation = 1 (Not important to be abstinent) to 10 (Very important to be abstinent); Self-efficacy = 1 (very unlikely to use) to 10 (very likely to use); Abstinence-focused coping = high score related to more abstinence focused coping skills; PR/NR status: 0 (negative reinforcement; NR) and 1 (positive reinforcement; PR). Tx=treatment.
Table 4 shows the results from the longitudinal mixed model polynomial trend analyses. The linear interaction effect was not significant (t= 1.68, p=.09), but the quadratic interaction effect of PR/NR group status over time was marginally significant (t=-1.95, p=.05; Table 4 top). Univariate follow up tests revealed that during outpatient treatment (3m follow-up) and 3-months following (6m follow-up), the NR group had significantly greater PDA than those in the PR group (ps<.04).
Table 4.
Prospective Linear mixed model results (N=109) of the effect of: a) PR/NR status on PDA over time (above); and, b) PR/NR status on PDA over time co-varying for all variables that significantly predicted outcomes at treatment intake (below)
| Variable | B | SE | df | t | p |
|---|---|---|---|---|---|
| Intercept | 44.222 | 4.892 | 107 | 9.04 | 0.000 |
| PR/NR status | 3.953 | 6.707 | 107 | 0.59 | 0.557 |
| Time | −0.265 | 1.539 | 290 | −0.17 | 0.864 |
| Time (quadratic) | 0.018 | 0.112 | 290 | 0.16 | 0.872 |
| Time* PR/NR status | 3.597 | 2.142 | 290 | 1.68 | 0.094 |
| Time (quadratic)* PR/NR status | −0.304 | 0.156 | 290 | −1.95 | 0.052 |
| Variable | B | SE | df | t | p |
|---|---|---|---|---|---|
| Intercept | 31.812 | 7.415 | 97 | 4.29 | 0.000 |
| PR/NR status | −5.738 | 6.249 | 97 | −0.92 | 0.361 |
| Time | −1.180 | 1.620 | 287 | −0.73 | 0.468 |
| Time (quadratic) | 0.081 | 0.116 | 287 | 0.70 | 0.487 |
| Time* PR/NR status | 3.867 | 2.247 | 287 | 1.72 | 0.088 |
| Time (quadratic)* PR/NR status | −0.322 | 0.160 | 287 | −2.01 | 0.047 |
| Prior outpatient treatment | 4.154 | 5.848 | 97 | 0.71 | 0.479 |
| Prior inpatient treatment | 4.603 | 6.259 | 97 | 0.74 | 0.464 |
| Past 90 days 12-step attendance | 21.774 | 6.380 | 97 | 3.41 | 0.001 |
| Motivation for abstinence | −0.231 | 0.862 | 97 | −0.27 | 0.789 |
| Abstinence self-efficacy | 0.809 | 0.889 | 97 | 0.91 | 0.365 |
| Abstinence-focused coping | 2.177 | 1.974 | 97 | 1.10 | 0.273 |
PR=Positive Reinforcement group; NR=negative reinforcement group; M= mean; SE= standard error; df= degrees of freedom; B=standardized partial beta coefficient; p= probability/significance level
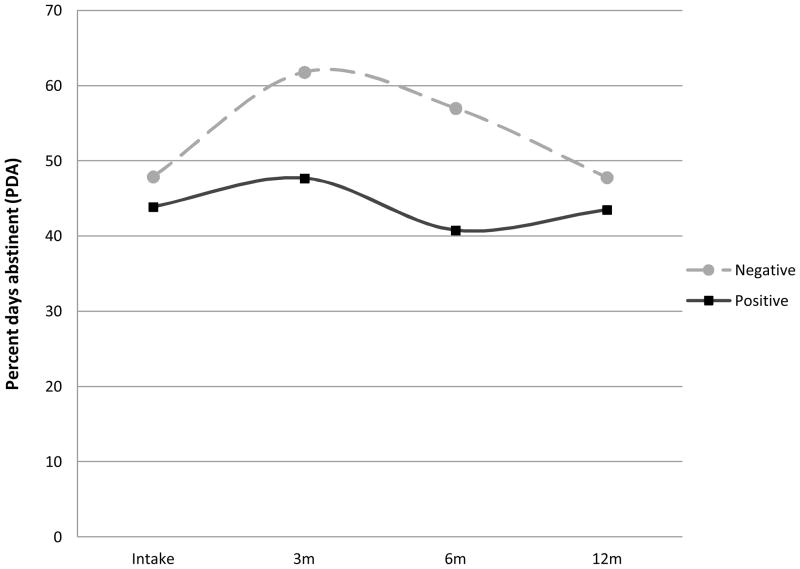
The NR group had a significant within-group increase in PDA (from intake to 3-month follow-up, which was sustained at 6 month follow-up, but converged by the 12-month follow-up (see Figure 1). Standardized effect size calculations revealed the auto-correlation-adjusted within-group differences at 3m follow-up to be in the medium effect size range (Cohen’s d = .330; Cohen, 1988). In contrast, the PR group showed no significant within-group change in relation to PDA during and directly following treatment.
Figure 1.
Treatment response and outcome by predominant reason for use category (Positive Reinforcement or Negative Reinforcement) among adolescent outpatients
Unique predictive utility of PR/NR status
Table 4 (bottom) shows the results of the full model test. There was not an independent linear interaction effect × time observed (t=1.72, p=.09) but the quadratic effect was statistically significant (t=−2.01, p<.05) with an interaction effect of PR/NR group status on outcome over time (see table 4, and figure 1). The only other significant predictor of outcome over time was 12-step attendance in the 90 days prior to treatment entry (t=3.41, p=.001).
Discussion
Findings from this study revealed there was an approximately equal distribution of adolescent outpatients reporting a PR and NR predominant reason for their drinking/drug use/problem. These subgroups did not differ on demographic variables, but were found to differ on several clinical variables with the NR subgroup generally exhibiting a higher density of psychopathology (i.e., more internalizing disorders) and a more severe substance use profile compared to the PR subgroup. Of note, the PR subgroup showed no significant benefit from outpatient treatment whereas the NR group showed a significant and positive treatment response in the medium effect size range that emerged during treatment and was sustained up to 6 months post-treatment. Furthermore, reason for use provided modest but uniquely predictive clinical outcome information independent of several other important traditional clinical indicators. In keeping with prior research that investigated psychological motives for alcohol use (e.g., Cooper et al, 1995; Patrick et al, 2011a; 2011b), results suggest adolescents’ predominant reason for using alcohol and other substances may provide clinically useful information about likely treatment response that could help clinicians tailor treatment efforts more effectively.
As mentioned, the NR group differed in their clinical profile at treatment intake exhibiting a more severe clinical profile on the whole. It is possible that this subgroup of patients is further along in the course of addiction having moved from a positively reinforcing “impulsive” stage to a more negatively reinforcing “compulsive” stage (Koob, 2004). Alternatively, this subgroup may represent a qualitatively different and more stable phenotypic subtype of individual that appears to use predominantly “to feel better” (NIDA, 2008). Although addiction typologies have been examined in general population (e.g., Moss, Chen, & Yi, 2007) and clinical (Babor et al, 1992; Cloningner, Sigvardsson, Gilligan, & von Knorring, 1988; Hesselbrock & Hesselbrock, 2006; Jellinek, 1960; Silkworth, 2001) samples, these have been cross-sectional. Longitudinal studies are needed to determine to what extent typological subgroups based on predominant reasons for use continue to differ quantitatively rather than qualitatively when followed over time (Patrick et al, 2011b).
Of note, those in the NR group were more likely to perceive they had a problem with alcohol or drugs, as compared to those in the PR group. However, while PR/NR status was related to outcome, recognition of having a problem with alcohol or other drugs was not. As such, this suggests there is something potentially unique about this PR/NR distinction.
Of practical clinical significance, adolescents’ reported reason for using alcohol or other drugs at treatment entry may indicate their likely treatment response to standard, group-oriented, skills-based treatment, which is the most common form of treatment delivered in typical community settings (Knudsen et al, 2008). Importantly, of the seven variables examined in the theoretically and empirically specified model shown initially to predict PDA over time, only the interaction of PR/NR status (modeled as a quadratic effect) with time and 12-step attendance in the 90 days prior to treatment intake contributed significantly to the full model predicting PDA. As alluded to by Engle and McGowan (2009), given the fact that the PR group showed no treatment response whereas the NR group showed a marked positive response (Figure 1), and PR/NR group status uniquely predicted treatment outcome, variables such as this may be useful in delineating more homogeneous subgroups that could benefit from different treatment approaches. Specifically, skills based CBT oriented treatment (which was delivered at this treatment site), may be a better fit for NR patients whereas a more focused and targeted motivational enhancement type interventions may produce a better response among PR youth in order to enhance this group’s problem recognition, perceived risk levels, and motivation for recovery. This important finding warrants additional research.
Another clinical consideration is the effect that mixing these two types of patients together in one group, specifically the impact on overall group treatment response. The nationally representative survey of 154 adolescent SUD treatment programs by Knudsen et al. (2008) found that the majority of treatment programs for adolescents are group-based, low intensity, and outpatient. If about half of treated adolescents are using for positive reinforcement, there could be an increased risk of iatrogenic effects. Specifically, if individuals perceive a lack of fit or witness “glorification” of drug use, this could weaken group engagement and cohesion, diminishing overall therapeutic gains.
Finally, although there were marked differences between PR and NR patients at 3 and 6 month follow-ups, this outcome difference diminished by 12 month follow-up. In keeping with a chronic care model of addiction recovery management (Godley et al, 2007; White, 2008; Kelly & White, 2010), this finding suggests that NR youth would benefit from ongoing treatment and recovery support services in order to maintain the higher rates of abstinence and recovery achieved during and shortly after outpatient care.
Limitations
Generalizations from this study should be made cautiously in light of some limitations. Predominant reasons for use were chosen from a provided list of potential reasons rather than self-generated in an open format. Although there was an “other” category present on this list, the existing documented reasons may have constricted the free generation of additional reasons. Also, two types of questions regarding reason for use were asked, depending on whether the youth believed they did or did not have a substance use problem; differences in the wording of these questions may have influenced provided reasons. Also, reasons were not examined by substance. Future research with larger samples should examine how reasons for use might differ along these or other lines (e.g., primary substance). Although the treatment program featured in this study was typical in format, content, focus, and service intensity of adolescent SUD outpatient treatment programs throughout the United States, it is still only a single program and the sample was moderate in size, mostly White, predominantly male, and reported mostly marijuana as their primary substance. Replications are needed to confirm the theoretical and clinical utility of this PR/NR status variable.
Conclusion
The increased emphasis on developing and implementing evidence-based treatments for adolescent SUD has been impressive and, during the past 10 years, the field overall has made significant progress. Despite this, adolescent treatment gains have been modest. Part of the challenge in treating adolescents is that they are characterized by broad heterogeneity in such variables as recovery motivation, degree of substance involvement and impairment, and psychiatric co-morbidities. However, for both logistical and healthcare cost and reimbursement reasons, most treatment is delivered in group format (Knudsen et al, 2008) making specific tailoring to the needs of important patient subgroups more challenging. Greater heterogeneity may mean that any single group-based treatment approach (e.g., skills-based interventions) may not cater effectively to the diverse range of needs of adolescents presenting for treatment.
Findings from this study suggest, however, that adolescents’ predominant reason for using substances at treatment entry is conceptually related to important theories of addiction development (e.g., Koob, 2004) and typologies, and also may provide face valid information that may have clinical utility providing a quick way to target treatments more effectively. Adolescents reporting alcohol/drug use for predominantly negative reinforcement reasons may respond better with a focus that helps them develop coping skills (e.g., in dealing with stress/high risk social situations/emotional regulation). On the other hand, adolescents using for predominantly positive reinforcement reasons may respond better to personalized feedback and other motivational enhancement techniques (e.g., personalized, normative, feedback in an MI style) designed to develop discrepancies between their substance use and their personal values in order to heighten cognitive dissonance, increase recovery motivation, and mobilize adaptive change.
References
- Anderson KG, Ramo DE, Brown SA. Life Stress, coping and comorbid youth: An examination of the stress-vulnerability model for substance relapse. Journal of Psychoactive Drugs. 2006;38(3):255–262. doi: 10.1080/02791072.2006.10399851. [DOI] [PubMed] [Google Scholar]
- Babor TF, Hoffman M, DelBoca FK, Hesselbrock V, Meyer RE, Dolinsky ZS, et al. Types of alcoholics I: Evidence for an empirically derived typology based on indicators of vulnerability and severity. Archives of General Psychiatry. 1992;49:599–608. doi: 10.1001/archpsyc.1992.01820080007002. [DOI] [PubMed] [Google Scholar]
- Brown SA, Myers MG, Lippke L, Tapert SF, Stewart DG, Vik PW. Psychometric evaluation of the Customary Drinking and Drug Use Record (CDDR): A measure of adolescent alcohol and drug involvement. Journal of Studies on Alcohol. 1998;59(4):427–438. doi: 10.15288/jsa.1998.59.427. [DOI] [PubMed] [Google Scholar]
- Brown SA, Ramo DE. Clinical course of youth following treatment for alcohol and drug problems. In: Liddle H, Rowe C, editors. Adolescent substance abuse: Research and clinical advances. Cambridge, UK: Cambridge University Press; 2006. pp. 79–103. [Google Scholar]
- Brown SA, Vik PW, Creamer VA. Characteristics of relapse following adolescent substance abuse treatment. Addictive Behaviors. 1989;14(3):291–300. doi: 10.1016/0306-4603(89)90060-9. [DOI] [PubMed] [Google Scholar]
- Burleson JA, Kaminer Y, Burke RH. Twelve-month follow-up of aftercare for adolescents with alcohol use disorders. Journal of Substance Abuse Treatment. 2012;42:78–86. doi: 10.1016/j.jsat.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung T, Maisto SA. Relapse to alcohol and other drug use in treated adolescents: Review and reconsideration of relapse as a change point in clinical course. Clinical Psychology Review. 2006;26(2):149–161. doi: 10.1016/j.cpr.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Cloninger C, Sigvardsson S, Gilligan SB, von Knorring A. Genetic heterogeneity and the classification of alcoholism. Advances In Alcohol & Substance Abuse. 1988;7(3–4):3–16. doi: 10.1300/J251v07n03_02. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- Dennis M, Funk R, Godley SH, Godley MD, Waldron H. Cross-validation of the alcohol and cannabis use measures in the Global Appraisal of Individual Needs (GAIN) and Timeline Followback (TLFB; Form 90) among adolescents in substance abuse treatment. 2004;99(suppl 2):120–128. doi: 10.1111/j.1360-0443.2004.00859.x. [DOI] [PubMed] [Google Scholar]
- Dennis M, Scott C, Funk R, Foss M. The duration and correlates of addiction and treatment careers. Journal of Substance Abuse Treatment. 2005;28:s51–s62. doi: 10.1016/j.jsat.2004.10.013. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory (BSI): An introductory report. Psychological Medicine. 1983;13(3):595–605. [PubMed] [Google Scholar]
- Engle B, MacGowan MJ. A critical review adolescent substance abuse group treatments. Journal of Evidence-Based Social Work. 2009;6(3):217–243. doi: 10.1080/15433710802686971. [DOI] [PubMed] [Google Scholar]
- Godley M, Godley S, Dennis M, Funk R, Passetti L. The effect of assertive continuing care on continuing care linkage, adherence and abstinence following residential treatment for adolescents with substance use disorders. Addiction. 2007;102(1):81–93. doi: 10.1111/j.1360-0443.2006.01648.x. [DOI] [PubMed] [Google Scholar]
- Godley S, Meyers R, Smith J, Karvinen T, Titus J, Godley M, et al. DHHS Pub No 01-3489. Vol. 4. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2001. The Adolescents Community Reinforcement Approach to Adolescent Cannabis use, Cannabis Youth Treatment (CYT) series. [Google Scholar]
- Goodman I, Peterson-Badali M, Henderson J. Understanding motivation for substance use treatment: The role of social pressure during the transition to adulthood. Addictive Behaviors. 2011;36(6):660–668. doi: 10.1016/j.addbeh.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Hesselbrock VM, Hesselbrock MN. Are there empirically supported and clinically useful subtypes of alcohol dependence? Addiction. 2006;101(s1):97–103. doi: 10.1111/j.1360-0443.2006.01596.x. [DOI] [PubMed] [Google Scholar]
- Jellinek EM. The Disease Concept of Alcoholism. New Haven CT: Hillhouse; 1960. [Google Scholar]
- Kaminer Y. Challenges and opportunities of group therapy for adolescent substance abuse: A critical review. Addictive Behaviors. 2005;30(9):1765–1774. doi: 10.1016/j.addbeh.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Kaminer Y, Burleson JA, Burke RH. Efficacy of outpatient aftercare for adolescents with alcohol use disorders: A randomized controlled study. Journal Of The American Academy Of Child & Adolescent Psychiatry. 2008;47(12):1405–1412. doi: 10.1097/CHI.0b013e318189147c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Dow SJ, Yeterian JD, Kahler C. Can 12-step group participation strengthen and extend the benefits of adolescent addiction treatment? A prospective analysis. Drug and Alcohol Dependence. 2010;110(1–2):117–125. doi: 10.1016/j.drugalcdep.2010.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Dow SJ, Yeterian JD, Kahler C. Can 12-step group participation strengthen and extend the benefits of adolescent addiction treatment? A prospective analysis. Drug and Alcohol Dependence. 2010;110(1–2):117–125. doi: 10.1016/j.drugalcdep.2010.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Myers MG, Brown SA. Do adolescents affiliate with 12-step groups?: A multivariate process model of effects. Journal Of Studies On Alcohol. 2002;63(3):293–304. doi: 10.15288/jsa.2002.63.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, White WL, editors. Addiction Recovery Management: Theory, Research, and Practice. New York, NY: Springer Science; 2011. [Google Scholar]
- Kelly JF, Urbanoski K. Youth Recovery Contexts: the incremental effects of 12-step attendance and involvement on adolescent outpatient treatment outcomes. Alcoholism: Clinical and Experimental Research. 2012 doi: 10.1111/j.1530-0277.2011.01727.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knudsen HK, Ducharme LJ, Roman PM, Johnson JA. Robert Wood Johnson Foundation’s Substance Abuse Policy Research Program (Grant No. 53130) 2008. Service delivery and use of evidence-based treatment practices in adolescent substance abuse treatment settings: Project report. [Google Scholar]
- Koob GF. Allostatic view of motivation: implications for psychopathology. In: Bevins RA, Bardo MT, editors. Motivational factors in the etiology of drug abuse. Vol. 50. Lincoln, NE: University of Nebraska Press; 2004. pp. 1–18. [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Engels R, Gmel G. Being drunk to have fun or to forget problems? Identifying enhancement and coping drinkers among risky drinking adolescents. European Journal of Psychological Assessment. 2010;26(1):46–54. [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- Miller WR, Del Boca F. Measurement of drinking behavior using the Form 90 family of instruments. Journal of Studies on Alcohol. 1994;S12:s112–s118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Moss HB, Chen CM, Yi H. Subtypes of alcohol dependence in a nationally representative sample. Drug and Alcohol Dependence. 2007;91(2–3):149–158. doi: 10.1016/j.drugalcdep.2007.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers MG, Brown SA. Coping and appraisal in potential relapse situations among adolescent substance abusers following treatment. Journal of Adolescent Chemical Dependency. 1990;1:95–115. [Google Scholar]
- National Institute of Drug Abuse. NIH publication no. 08-5605. 2008. Drugs, brains, and behavior: The science of addiction. [Google Scholar]
- Patrick ME, Schulenberg JE, O’Malley PM, Maggs JL, Kloska DD, Johnston LD, Bachman JG. Age-related changes in reasons for using alcohol and marijuana from ages 18 to 30 in a national sample. Psychology Addictive Behaviors. 2011a;25(2):330–339. doi: 10.1037/a0022445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Schulenberg JE, O’Malley P, Johnston LD, Bachman JG. Adolescents’ Reported Reasons for Alcohol and Marijuana Use as Predictors of Substance Use and Problems in Adulthood. Journal of studies on alcohol and drugs. 2011b;72(1):106–116. doi: 10.15288/jsad.2011.72.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo D, Brown SA. Reasons for relapse: Classes of substance abuse relapse situations: A comparison of adolescents and adults. Psychology of Addictive Behaviors. 2008;22 (3):372–379. doi: 10.1037/0893-164X.22.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheurich A, Müller MJ, Anghelescu I, Lörch B, Dreher M, Hautzinger, Szegedi M. Reliability and Validity of the Form 90 Interview. European Addiction Research. 11(1):50–56. doi: 10.1159/000081417. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas C, Dulcan M, Schwab-Stone M. NIMH Diagnostic Interview Schedule for Children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Silkwood WD. Alcoholics Anonymous: The story of how thousands of men and women have recovered from alcoholism. 4. New York, NY: Alcoholics Anonymous World Services; 2001. The doctor’s opinion; pp. xxiii–xxxii. [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biochemical methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Sussman S, Skara S, Ames SL. Substance abuse among adolescents. Substance Use & Misuse. 2008;43(12–13):1802–1828. doi: 10.1080/10826080802297302. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration [SAMSHA] NSDUH Series H-38A, HHS Publication No SMA 10-4586 Findings. Rockville, MD: Office of Applied Studies; 2010. Results from the 2009 National Survey on Drug Use and Health: Volume I. Summary of National Findings. [Google Scholar]
- Swindle RW, Peterson K, Paradise MJ, Moos RH. Measuring substance abuse program treatment orientations: The Drug and Alcohol Program Treatment Inventory. Journal of Substance Abuse. 1995;7(1):61–78. doi: 10.1016/0899-3289(95)90306-2. [DOI] [PubMed] [Google Scholar]
- The National Center on Addiction and Substance Abuse (CASA) at Columbia University. Adolescent substance use: America’s #1 public health problem. New York: CASA; 2011. [Google Scholar]
- Tims FM, Dennis ML, Hamilton N, Buchan BJ, Diamond G. Characteristics and problems of 600 adolescent cannabis abusers in outpatient treatment. Addiction. 2002;97:46–57. doi: 10.1046/j.1360-0443.97.s01.7.x. [DOI] [PubMed] [Google Scholar]
- Titus JC, Godley SH, White MK. A post-treatment examination of adolescents’ reasons for starting, quitting, and continuing the use of drugs and alcohol. Journal of Child & Adolescent Substance Abuse. 2007;16(2):31–49. [Google Scholar]
- Tonigan JS, Miller WR. The Inventory of Drug Use Consequences (InDUC): Test-retest stability and sensitivity to detect change. Psychology of Addictive Behaviors. 2002;16(2):165–168. [PubMed] [Google Scholar]
- Webb C, Scudder M, Kaminer Y, Kadden R. DHHS Pub No (SMA) 02-3659. Vol. 2. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2002. The Motivational Enhancement Therapy and Cognitive Behavioral Therapy Supplement: 7 Sessions of Cognitive Behavioral Therapy for Adolescent Cannabis Users, Cannabis Youth Treatment (CYT) Series. [Google Scholar]
- Wei CC, Heckman BD, Gay J, Weeks J. Correlates of motivation to change in adolescents completing residential substance use treatment. J Subst Abuse Treat. 2011;40:272–280. doi: 10.1016/j.jsat.2010.11.014. [DOI] [PubMed] [Google Scholar]
- White WL. Recovery Management and Recovery-Oriented Systems of Care: Scientific Rationale and Promising Practices. Northeast Addiction Technology Transfer Center, Great Lakes Addiction Technology Transfer Center, Philadelphia Department of Behavioral Health/Mental Retardation Services; 2008. [Google Scholar]
- Winters KC, Henly GA. Personal Experience Inventory (PEI) Test and Manual. Los Angeles, CA: Western Psychological Services; 1989. [Google Scholar]