Abstract
Study Design This is a retrospective study.
Objective The objective of this study was to assess the sagittal stable vertebra (SSV) versus the first lordotic vertebra (FLV) as the inferior fusion level in patients undergoing spinal surgery for thoracic hyperkyphosis. The main outcome of interest was the development of distal junctional kyphosis (DJK).
Summary of Background Data Prior research has pointed to selection of the FLV for the distal instrumentation level in fusion for thoracic hyperkyphosis. In 2009, Cho et al introduced the concept of the SSV after recognizing the development of DJK despite fusion to the FLV.
Methods Patients were reviewed who had undergone spinal fusion for thoracic hyperkyphosis. Preoperative radiographs were reviewed to assess thoracic kyphosis, lumbar lordosis, SSV, and FLV. Postoperative radiographs were reviewed to assess curve correction and whether patients developed DJK or implant failure.
Results We reviewed 22 patients with a mean age at surgery of 18 (range 14 to 22). Mean preoperative kyphosis was 85 ± 14 degrees, and mean postoperative kyphosis at final follow-up was 59 ± 12 degrees for a mean correction of 26 ± 12 degrees. Eleven patients developed DJK and four patients experienced hardware failure. In 12 patients, the SSV was inferior to the FLV. Rates of DJK when the instrumentation included the SSV or FLV were 13 and 38%, respectively.
Conclusions Fusion to the SSV is superior at preventing DJK when compared with fusion to the FLV.
Keywords: thoracic hyperkyphosis, Scheuermann kyphosis, spinal fusion, sagittal stable, vertebra
Introduction
Deciding on surgical fusion levels in spinal deformity surgery is a challenging process. While there has been a great deal published to guide the decision-making process in scoliosis, the evidence in thoracic hyperkyphosis is limited to multiple small case series.1 2 3 4 5 6 Much of the literature regarding thoracic hyperkyphosis has pertained to Scheuermann kyphosis (SK). SK is the most common etiology of thoracic hyperkyphosis in adolescent and young adult patients presenting to spinal surgeons with a reported incidence between 1 and 8%.7
The indications and methods for spinal fusion in thoracic hyperkyphosis are controversial. The most accepted indication for surgery is a painful kyphosis resistant to nonoperative management,8 while some authors still advocate for surgery based on deformity alone.9 Current controversies regarding the natural history of thoracic hyperkyphosis versus the outcomes of surgical intervention make the process of clinical decision-making difficult.7 8 10
Surgery for thoracic hyperkyphosis was originally described as a posterior only instrumented fusion procedure.1 Many authors now advocate the addition of an anterior release and segmental interbody fusion before posterior instrumentation to optimize curve correction and fusion.5 8 As pedicle screw instrumentation has developed with superior strength compared with hooks and cables,11 the superiority of combined anterior/posterior surgery over posterior alone procedures has been questioned.4
Complication rates following surgery for thoracic hyperkyphosis have been reported at 15%, with rates significantly higher in adult patients.12 A well-recognized complication is the development of junctional kyphosis.3 5 8 This can occur proximal or distal to the instrumentation. It is generally accepted that fusion must include the superior end of the thoracic kyphosis to avoid superior junctional kyphosis.3 8 Previous authors have advocated extending instrumentation down to the first lordotic vertebra (FLV) to minimize the risk of developing distal junctional kyphosis (DJK).3 5 8 The FLV has been defined as the vertebra immediately inferior to the first lordotic lumbar disk.3
King et al first introduced the concept of the stable vertebra to guide the selection of fusion levels in surgery for scoliosis.13 In 2009, Cho et al introduced the concept of the sagittal stable vertebra (SSV) to guide selection of the inferior fusion level in the setting of thoracic hyperkyphosis. The SSV was defined as “the most proximal vertebra touched by the posterior sacral vertical line (PSVL).2”
The primary purpose of the present study was to assess whether the SSV or FLV would be a better measurement tool in determining the inferior fusion level for thoracic hyperkyphosis. Both of these are relatively easy measurements that can be made off the lateral standing radiograph routinely obtained before surgery, as outlined in Fig. 1. We sought to investigate the rates of clinical and radiographic failure at the inferior end of these fusion constructs.
Figure 1.
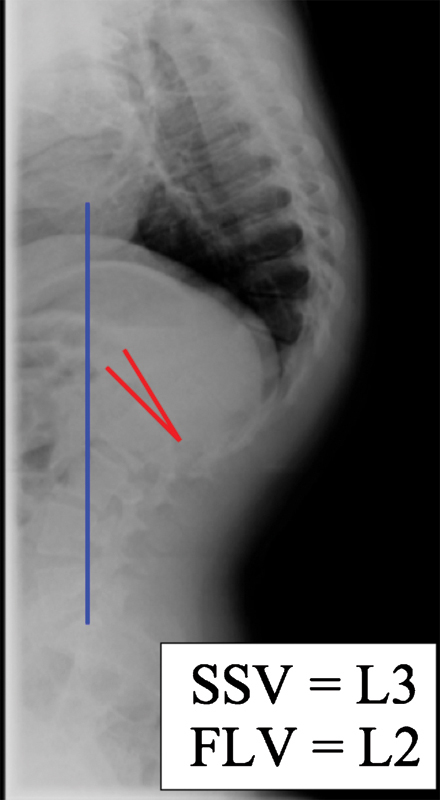
This figure demonstrates how to determine the SSV and FLV. The blue line represents the posterior sacral vertical line draw vertically from the posterior margin of superior endplate of S1. The most superior vertebra, inferior to the apex of the kyphosis, touched by this line represents the SSV. The red lines demonstrate the first lordotic lumbar disk segment. The FLV is the vertebra just inferior to this disk segment. FLV, first lordotic vertebra; SSV, sagittal stable vertebra.
Materials and Methods
Patient databases from the local children's hospital and from the practice of one adult spinal deformity surgeon were searched to find all patients who had undergone surgery for the correction of thoracic hyperkyphosis. We sought to include all patients where selection of the distal fusion level was based on assessment of sagittal balance on the lateral upright spine radiograph. Patients with a primary diagnosis of scoliosis were excluded as their distal fusion level was generally more influenced by coronal balance on the PA radiograph. Patients were excluded if their pre- or postoperative full-length standing spine radiographs were unavailable for review. We also chose to exclude patients with syndromic spinal deformity.
Pre- and postoperative standing lateral complete spine radiographs were reviewed. The first lordotic disk and FLV were recorded, and the SSV was established based on the description by Cho et al on the preoperative film.2 Other measurements included pre- and postoperative thoracic kyphosis, lumbar lordosis, lowest instrumented vertebra (LIV), and upper instrumented vertebra. All curve measurements were obtained using the cobb technique whereby curves were measured from the uppermost to the lowermost tilted vertebra for that curve.14 All postoperative films were assessed for evidence of hardware failure (defined as breakage or intraosseous change in position from immediate postoperative imaging) and for development of DJK (Fig. 2). DJK was defined as any disk distal to the instrumentation that was lordotic preoperatively and became neutral or kyphotic postoperatively, based on the standing lateral radiograph.
Figure 2.
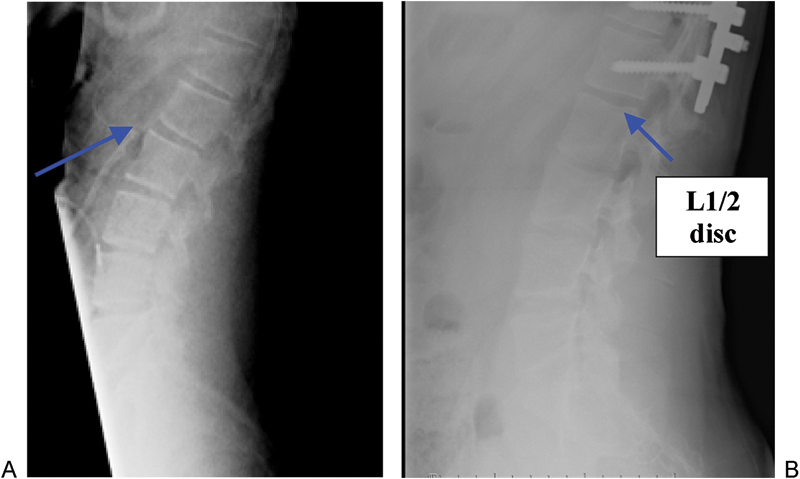
This figure demonstrates the development of distal junctional kyphosis. Note how the lordotic alignment of the L1/2 disk space changes between the (A) pre- and (B) postoperative standing lateral radiograph.
All patients in this study underwent a staged anterior release and interbody grafting followed by an instrument posterior fusion. The anterior release involved a thoracotomy including excision of one rib. Complete discectomies were performed at all levels that could access through the single level thoracotomy. The excised rib was then cut into two pieces and used as interbody bone graft at all discectomy sites. Posterior instrumented fusion was performed on a separate day. Fusion levels were decided intraoperatively by the chief operating surgeon on the day of the operating room. Instrumentation included all pedicle screw constructs at the inferior segments. At the superior end of the instrumentation, a variety of pedicle screws, hooks, and claw constructs was used at the discretion of the operating surgeon.
Statistical analysis was performed using Stata 10 (StatCorp, Texas, United States) software. Basic demographic data were analyzed for mean and standard deviation. Mann–Whitney U test was used to assess curve differences between patients who did or did not develop DJK. Logistic regression was performed to assess the contribution of fusion to the FLV versus the SSV for prevention of DJK. Statistical significance was defined as a p value <0.05.
Results
We included 22 patients for analysis. The mean age at surgery was 18 years (range 14 to 22). Half of the patients (11/22) was male. Sixteen patients had radiographic findings consistent with SK. Three patients had a mild scoliosis in conjunction with their hyperkyphosis. This scoliosis measured less than 25 degrees in all cases. Two patients had a diagnosis of congenital kyphosis. All but one patient had at least 2 years of postoperative follow-up. The one patient who did not is case #1 in Table 1. This patient had DJK and hardware failure before the 6-month follow-up following fusion to the FLV, but above the SSV. She underwent revision to extend her fusion distally.
Table 1. Demographic Patient Data Including Basic Radiographic Data.
| Case # | Age at Surgery (y) | Diagnosis | SSV | FLV | LIV | Inferior Implant Failure | Inferior Junctional Kyphosis |
|---|---|---|---|---|---|---|---|
| 1 | 18 | SK | L3 | L2 | L2 | Yes | Yes |
| 2 | 22 | Kyphosis (mild scoliosis) | L3 | L2 | L2 | No | No |
| 3 | 18 | Kyphosis (mild scoliosis) | L2 | L2 | L3 | No | No |
| 4 | 17 | SK | L3 | L3 | L3 | Yes | Yes |
| 5 | 19 | SK | L3 | L2 | L1 | Yes | Yes |
| 6 | 19 | SK | L2 | L2 | L1 | Yes | Yes |
| 7 | 20 | SK | L2 | L2 | L1 | No | No |
| 8 | 17 | SK | L1 | L1 | L1 | No | No |
| 9 | 18 | SK | L2 | L2 | L1 | No | Yes |
| 10 | 16 | SK | L2 | L1 | L1 | No | Yes |
| 11 | 19 | SK | L3 | L2 | L2 | No | No |
| 12 | 17 | Congenital kyphosis | L3 | L2 | L2 | No | No |
| 13 | 15 | SK | L2 | L1 | L2 | No | No |
| 14 | 14 | Congenital kyphosis | L3 | L2 | L2 | No | Yes |
| 15 | 15 | SK | L2 | L1 | T12 | No | Yes |
| 16 | 16 | SK | L3 | L2 | L2 | No | Yes |
| 17 | 17 | Kyphosis (mild scoliosis) | L3 | L2 | L1 | No | Yes |
| 18 | 15 | SK | L2 | L2 | L2 | No | No |
| 19 | 19 | SK | L3 | L2 | L2 | No | Yes |
| 20 | 17 | SK | L1 | L1 | L1 | No | No |
| 21 | 22 | SK | L2 | L2 | L2 | No | No |
| 22 | 22 | SK | L1 | L1 | L1 | No | No |
y, year; SSV, sagittal stable vertebra; FLV, first lordotic vertebra; LIV, lowest instrumented vertebra; SK, Scheuermann kyphosis.
The mean preoperative thoracic kyphosis was 85 ± 14 degrees. The mean postoperative kyphosis at final follow-up was 59 ± 12 degrees, resulting in a mean curve correction of 26 ± 12 degrees. This represents a mean 30 ± 11% (range 8 to 50%) curve correction.
In 12 patients, the SSV was one vertebral level inferior to the FLV. The SSV and FLV were measured at the same level in the remaining 10 patients. Table 1 outlines the SSV, FLV, and LIV for each patient as well as whether they developed DJK or implant failure.
Eleven patients developed DJK. All cases of DJK were evident on standing lateral radiographs within 6 months of surgery. There were no significant differences in the curve characteristics in those patients who did or did not develop DJK (Table 2). DJK developed in 6/16 (38%) patients who were fused to the FLV as compared with 1/9 (11%) patients who were fused to the SSV. If the LIV fell proximal to the FLV or SSV, the respective rates of DJK were 5/6 (83%) and 10/14 (71%). Fig. 3 outlines the rates of DJK in these groups. Logistic regression analysis revealed that fusion to the FLV was over four times more likely to produce DJK than when fused to the SSV, with odds ratio of 0.33 and 0.08, respectively (Table 3).
Table 2. Comparison of Curve Measurements and Correction in Those Who Did and Did Not Develop DJK.
| Developed DJK | |||
|---|---|---|---|
| Yes (n = 11) | No (n = 12) | p Value | |
| Preoperative thoracic kyphosis | 84° ± 17° | 87° ± 11° | ns |
| Final postoperative thoracic kyphosis | 58° ± 12° | 60° ± 12° | ns |
| Kyphosis correction | 26° ± 13° | 27° ± 12° | ns |
| Preoperative lumbar lordosis | 73° ± 14° | 78° ± 16° | ns |
| Final postoperative lumbar lordosis | 57° ± 13° | 66° ± 15° | ns |
| Lordosis correction | 16° ± 8° | 12° ± 6° | ns |
ns, not significant; p > 0.05.
DJK, distal junctional kyphosis.
Figure 3.
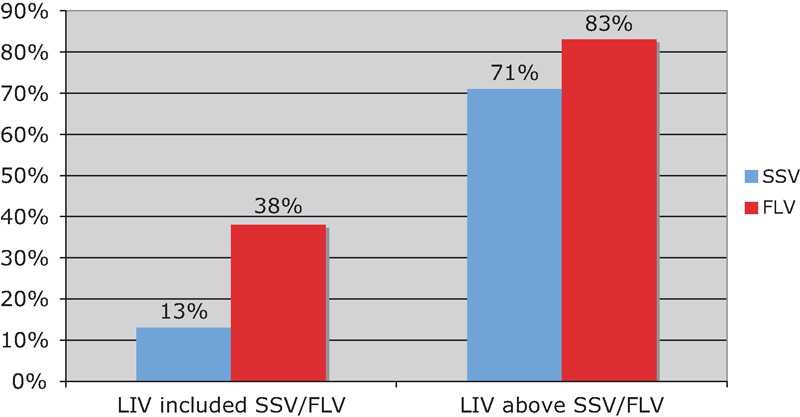
Rates of the development of distal junctional kyphosis depending on whether the patients' LIV included, or was above, the SSV or the FLV. FLV, first lordotic vertebra; LIV, lowest instrumented vertebra; SSV, sagittal stable vertebra.
Table 3. Logistic Regression Analysis—Odds of Developing DJK When Fused to the SSV versus the FLV.
| Odds Ratio | p Value | 95% Confidence Interval | |
|---|---|---|---|
| Fused to SSV | 0.08a | <0.05a | 0.01–1.0 |
| Fused to FLV | 0.34 | ns (>0.05) | 0.03–4.4 |
Achieved statistical significance.
DJK, distal junctional kyphosis; SSV, sagittal stable vertebra; FLV, first lordotic vertebra; ns, not significant.
Four patients developed inferior implant failure and three of these required revision surgery. One of these patients displayed an intraosseous shift in their inferior pedicle screws, but was asymptomatic and thus has been followed clinically. In total, five patients required revision surgery: three for inferior implant failure and two for superior hardware failure. All three inferior implant failures were pedicle screw constructs. Both of the superior implant failures were hook/claw constructs and one had been fused inferior to the superior end of the thoracic kyphosis. Both of these cases were revised to superior pedicle screw constructs and were extended to include the superior end of the kyphosis. Fig. 4 outlines the rates of implant failure in those patients who were or were not fused to the SSV or FLV.
Figure 4.
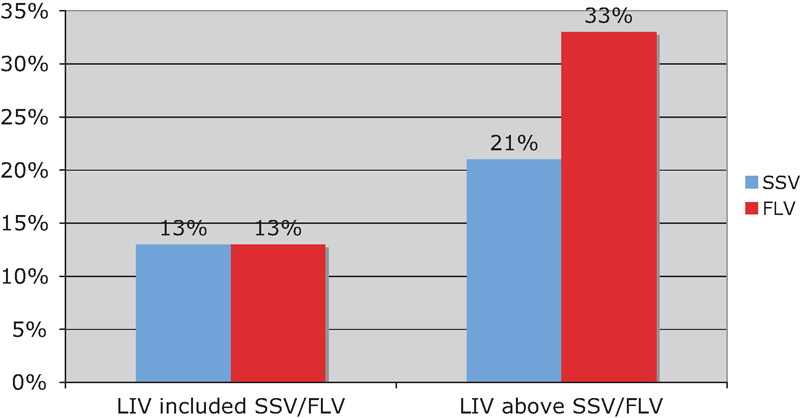
Rates of implant failure if the patients' LIV included, or was above, the SSV or the FLV. FLV, first lordotic vertebra; LIV, lowest instrumented vertebra; SSV, sagittal stable vertebra.
Discussion
The SSV was one vertebra inferior to the FLV in 55% (12/22) of patients. One case at our institution was operated on where the SSV was superior to the FLV (SSV at T10 and FLV at L2 with LIV at L2), but this patient had a diagnosis of Stickler syndrome with an atypical etiology to their spinal deformity and thus was excluded from analysis. This patient did not display any evidence of proximal or DJK and had no hardware issues. On review of the work of Cho et al, 61% of their patients had an SSV inferior to the FLV and no patients had an SSV superior to the FLV.2
DJK occurred in 50% of patients in this study. Previously reported rates range from 0 to 28%.2 3 Our rate of DJK when the LIV was superior to the SSV was 71%, which was identical to the rate of DJK that was observed in the study by Cho et al.2 Six patients in this study were fused above the FLV, five of which developed DJK. Fusion above either the FLV or the SSV results in a concerning rate of DJK.
Only one patient developed DJK despite fusion to the SSV. This patient also experienced distal implant failure and required revision surgery to extend the fusion. Fusion to the SSV was proven to be statistically superior over fusion to the FLV in preventing DJK based on logistic regression analysis (Table 3).
The clinical significance of DJK is currently unclear. Of the 11 patients with DJK in this study, seven were clinically asymptomatic. It is possible that a mild degree of DJK would go unnoticed without careful inspection of the postoperative radiographs. Patients with thoracic hyperkyphosis have an increased lumbar lordosis, likely representing a compensatory mechanism to help optimize sagittal balance. Jansen et al demonstrated, in a case series of 30 patients with SK, that this lordosis decreases when the thoracic hyperkyphosis is corrected surgically, and that most of this lordosis correction occurs in the upper lumbar segments.15 One may argue that DJK represents the lumbar spine's attempt to optimize sagittal balance without sacrificing lordosis in the lower lumbar segments. DJK may be a natural postoperative compensatory mechanism rather than a progression of the pathologic kyphosis in the thoracic spine.
Three patients in this series experienced distal implant failure requiring revision surgery. Two other patients had failure of their proximal instrumentation. This represents a clinical failure rate of 22%, which is higher than previously reported rates of 0 to 3% for implant complications.11 12 The mean curve correction in this study was 30% with no patient corrected >50%, which has previously been reported as a significant risk factor for the development of junctional kyphosis or implant failure requiring revision surgery.3 5 Distal pedicle screw constructs have been shown to have biomechanical superiority to hook or cable constructs alone, but hooks or cables can be used as supplements for additional strength.11 Due to the small numbers in this study, we were unable to show a difference in implant failure rates in relation to fusion to the SSV or FLV.
As a consequence of this study, we now routinely assess for the SSV on the lateral standing complete spine radiograph. We recently operated on a young male patient with a 110-degree kyphosis secondary to Marfan syndrome. On the preoperative standing lateral radiograph, the FLV was L1 and the SSV was L2. The patient underwent an anterior release from T3 to T8 with interbody rib grafting followed by a staged posterior fusion 2 weeks later. In between the anterior and posterior surgery, the patient had a repeat standing lateral radiograph of his spine. On this interim radiograph the FLV remained at L1, but the SSV was now also at L1. The anterior release had altered the sagittal alignment of the spine. This led to the question of whether it would be best to fuse to the SSV based on the preoperative radiograph versus the interim radiograph; clearly a question for further research.
This study contains several limitations. It is a relatively small retrospective case series and contains the inherent bias therein. Surgery for thoracic hyperkyphosis is relatively uncommon surgery, and this series is similar in size to other series published on this topic. Also, our series does not exclusively deal with patients with a diagnosis of SK. We felt that the criteria discussed in this study was relevant to surgical decision making in most cases of thoracic hyperkyphosis where fusion levels were decided based on measurements from the lateral radiograph.
Additionally, not all patients had identical surgical procedures. All patients had an anterior release and interbody bone grafting followed by a staged posterior fusion with pedicle screws used for the lower instrumentation. Instrumentation varied for the upper segments and included hook/claw constructs, pedicle screw constructs, and hybrid constructs. Our numbers were not large enough to subdivide the different instrumentation groups for analysis.
The main goal for this article was to assess distal fusion level and DJK. Proximal junctional kyphosis is also a significant clinical issue following spinal deformity surgery and definitely occurred in some of the patients in this series. However, due to the heterogeneity in fixation methods at the proximal end of the fusion constructs in patients, in this series we considered it more appropriate to try and focus on one the single clinical question of assessing the optimal distal fusion level.
Based on this study, fusion to the SSV is superior as compared with fusion to the FLV in preventing the postoperative development of DJK in patients with thoracic hyperkyphosis. This case series was not large enough to provide good evidence to support either the SSV or FLV as a guide to prevent implant failure. The SSV appears to fall inferior to the FLV in over 50% of cases. Given the high rates of DJK when fusion is superior to either the SSV or the FLV, we would recommend fusion to at least the more inferior of the two measurements.
Disclosures
Kristopher Lundine, None
Peter Turner, None
Michael Johnson, None
References
- 1.Bradford D S, Moe J H, Montalvo F J, Winter R B. Scheuermann's kyphosis. Results of surgical treatment by posterior spine arthrodesis in twenty-two patients. J Bone Joint Surg Am. 1975;57(4):439–448. [PubMed] [Google Scholar]
- 2.Cho K J, Lenke L G, Bridwell K H, Kamiya M, Sides B. Selection of the optimal distal fusion level in posterior instrumentation and fusion for thoracic hyperkyphosis: the sagittal stable vertebra concept. Spine. 2009;34(8):765–770. doi: 10.1097/BRS.0b013e31819e28ed. [DOI] [PubMed] [Google Scholar]
- 3.Denis F, Sun E C, Winter R B. Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: minimum five-year follow-up. Spine. 2009;34(20):E729–E734. doi: 10.1097/BRS.0b013e3181ae2ab2. [DOI] [PubMed] [Google Scholar]
- 4.Lee S S, Lenke L G, Kuklo T R. et al. Comparison of Scheuermann kyphosis correction by posterior-only thoracic pedicle screw fixation versus combined anterior/posterior fusion. Spine. 2006;31(20):2316–2321. doi: 10.1097/01.brs.0000238977.36165.b8. [DOI] [PubMed] [Google Scholar]
- 5.Lowe T G, Kasten M D. An analysis of sagittal curves and balance after Cotrel-Dubousset instrumentation for kyphosis secondary to Scheuermann's disease. A review of 32 patients. Spine. 1994;19(15):1680–1685. doi: 10.1097/00007632-199408000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Poolman R W, Been H D, Ubags L H. Clinical outcome and radiographic results after operative treatment of Scheuermann's disease. Eur Spine J. 2002;11(6):561–569. doi: 10.1007/s00586-002-0418-6. [DOI] [PubMed] [Google Scholar]
- 7.Lowe T G, Line B G. Evidence based medicine: analysis of Scheuermann kyphosis. Spine. 2007;32(19, Suppl):S115–S119. doi: 10.1097/BRS.0b013e3181354501. [DOI] [PubMed] [Google Scholar]
- 8.Wenger D R, Frick S L. Scheuermann kyphosis. Spine. 1999;24(24):2630–2639. doi: 10.1097/00007632-199912150-00010. [DOI] [PubMed] [Google Scholar]
- 9.Lowe T G. Scheuermann disease. J Bone Joint Surg Am. 1990;72(6):940–945. [PubMed] [Google Scholar]
- 10.Murray P M, Weinstein S L, Spratt K F. The natural history and long-term follow-up of Scheuermann kyphosis. J Bone Joint Surg Am. 1993;75(2):236–248. doi: 10.2106/00004623-199302000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Sun E, Alkalay R, Vader D, Snyder B D. Preventing distal pullout of posterior spine instrumentation in thoracic hyperkyphosis: a biomechanical analysis. J Spinal Disord Tech. 2009;22(4):270–277. doi: 10.1097/BSD.0b013e31816a6887. [DOI] [PubMed] [Google Scholar]
- 12.Coe J D, Smith J S, Berven S. et al. Complications of spinal fusion for Scheuermann kyphosis: a report of the scoliosis research society morbidity and mortality committee. Spine. 2010;35(1):99–103. doi: 10.1097/BRS.0b013e3181c47f0f. [DOI] [PubMed] [Google Scholar]
- 13.King H A, Moe J H, Bradford D S, Winter R B. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am. 1983;65(9):1302–1313. [PubMed] [Google Scholar]
- 14.Winter R B, Lonstein J E, Denis F. Sagittal spinal alignment: the true measurement, norms, and description of correction for thoracic kyphosis. J Spinal Disord Tech. 2009;22(5):311–314. doi: 10.1097/BSD.0b013e31817dfcc3. [DOI] [PubMed] [Google Scholar]
- 15.Jansen R C, van Rhijn L W, van Ooij A. Predictable correction of the unfused lumbar lordosis after thoracic correction and fusion in Scheuermann kyphosis. Spine. 2006;31(11):1227–1231. doi: 10.1097/01.brs.0000217682.53629.ad. [DOI] [PubMed] [Google Scholar]


