Abstract
Background The establishment of a spine trauma registry collecting both spine column and spinal cord data should improve the evidential basis for clinical decisions. This is a report on the pilot of a spine trauma registry including development of a minimum dataset.
Methods A minimum dataset consisting of 56 data items was created using the modified Delphi technique. A pilot study was performed on 104 consecutive spine trauma patients recruited by the Victorian Orthopaedic Trauma Outcomes Registry (VOTOR). Data analysis and collection methodology were reviewed to determine its feasibility.
Results Minimum dataset collection aided by a dataset dictionary was uncomplicated (average of 5 minutes per patient). Data analysis revealed three significant findings: (1) a peak in the 40 to 60 years age group; (2) premorbid functional independence in the majority of patients; and (3) significant proportion being on antiplatelet or anticoagulation medications. Of the 141 traumatic spine fractures, the thoracolumbar segment was the most frequent site of injury. Most were neurologically intact (89%). Our study group had satisfactory 6-month patient-reported outcomes.
Conclusion The minimum dataset had high completion rates, was practical and feasible to collect. This pilot study is the basis for the development of a spine trauma registry at the Level 1 trauma center.
Keywords: registry, spine trauma, minimum dataset, Victorian Orthopaedic Trauma Outcomes Registry
Introduction
Spine trauma contributes significantly to the global health and economic burden of individuals, families, and society. Spine trauma has traditionally been divided into spinal cord and spine column injuries. It is interesting to note that there is disproportionate emphasis on spinal cord injuries in the literature1 even with published incidence of spinal column trauma being much greater than spinal cord injuries.2 3 4 While the lifetime cost of a single spinal cord injured patient is significant, spine column injuries have a similar economic burden.5 6
Spine trauma data are collected mainly by dedicated spine trauma registries.7 8 9 10 11 12 13 14 15 16 17 18 19 20 These registries collect spinal cord injury data alone or spinal cord and spine column trauma data. At present, there is a paucity of dedicated spine trauma registries. Also, the majority of these registries collect only spinal cord injury data. It is imperative that spine trauma registries collect both spine column and spinal cord injury data as there is still little consensus on the optimal management of spine trauma. This is compounded by the difficulty in performing spine trauma randomized controlled trials.21 Clinical registry and cohort data are a feasible and alternative source of evidence-based information that may be a better methodology for many of the questions related to spine trauma. To be most useful, registries should meet the five standards that define clinical quality registries: (1) having mergeable data, (2) having a standardized dataset, (3) having rules for data collection, (4) having knowledge of patient outcomes, and (5) having a queriable database.22
Victorian Orthopaedic Trauma Outcomes Registry (VOTOR) is a comprehensive sentinel site database of orthopedic injuries including spinal injuries based on admissions to the adult Major Trauma Services (MTSs) and the Geelong and Northern Hospitals in Victoria.23 24 VOTOR reports spinal fractures as one the five most common injuries sustained by patients with isolated orthopedic and other injuries.23
This study was undertaken to develop and pilot a spine trauma registry minimum dataset. It was also performed to define the data collection methodology.
Method
Site
The establishment of the Victorian State Trauma System in 2000 ensured that 90% of major trauma patients were treated in a MTS with an estimated capture of 1700 major trauma cases annually.25 26 As a result, adult patients with acute spine column and spinal cord injury are delivered rapidly to the Alfred Hospital, a Level 1 trauma center that provides initial care and definitive management for the majority of spine trauma patients presenting in the state of Victoria.
Minimum Dataset
A review of all publications relating to spine trauma registries was conducted using Medline (1950 to April 2011) and EMBASE (1980 to April 2011). We identified 3756 articles that reported on spinal cord and/or spine column trauma. We excluded articles by title or abstract that clearly indicated that the data source was not a trauma or spine registry or if the spinal injury was not traumatic. Then, 323 full-text articles of the remaining studies were obtained and reviewed to ascertain the range of clinical data collected.
Using the modified Delphi technique, a minimum dataset and dataset dictionary were created.27 The Delphi technique is a structured communication technique,developed as a systematic and interactive method, which relies on a panel of experts in achieving a consensus. The modified Delphi technique used here differs from the Delphi technique by commencing the process with items synthesized from the literature reviews and content expert interviews rather than an open-ended question. The minimum dataset was a collaborative effort between the neurosurgery, orthopedic, and trauma departments of the Alfred Hospital, Melbourne. Two rounds of the modified Delphi technique were conducted before consensus was achieved.
The spine trauma registry pilot minimum dataset consists of 56 data items (Table 1). The minimum dataset has seven history data items consisting of comorbidities, anticoagulation and antiplatelet medications, previous spinal injury or surgery, and premorbid functional status indicators (activities of daily living, mobility, and cognition). There are four clinical examination data items consisting of the American Spinal Injury Association impairment scale, spinal cord injury level(s), spinal cord injury clinical syndromes, and nerve root injury level(s). There are 22 spine injury characteristics data items consisting of total spine injured levels, description of spine fractures from the occipital condyle to the coccyx based on radiographic injury morphology, and discoligamentous integrity for the subaxial cervical spine, thoracic, and lumbar spine (C3-L5). There are 18 management data items consisting of management approach, listing of orthosis, surgical parameters such as timing to surgery, surgical approach, surgical level(s), surgical procedure(s), and device(s) used. There are five outcome data items consisting of physician-reported outcomes such as findings during the outpatient review and patient-reported outcomes collected at 6 and 12 months posttrauma such as the short-form health survey (SF-12),28 Glasgow outcome score extended (GOSE),29 and pain scores.
Table 1. Spine Trauma Registry Minimum Dataset Data Items.
| Category | Data Items |
|---|---|
| History | • Comorbidities • Anticoagulation medications • Antiplatelet medications • Previous spinal injury or surgery • Functional status ○ Activities of daily living ○ Mobility ○ Cognition |
| Clinical examination | • ASIA impairment scale • Spinal cord injury level(s) • Spinal cord syndromes • Nerve root injury level(s) |
| Spine injury characteristic | • Sum of injury levels • Upper cervical spine (C0-C2) ○ C0-C2 dislocation/dissociation ○ Occipital condyle fracture (list subtypes) ○ C1 arch fracture (list subtypes) ○ C1/2 rotatory subluxation ○ C2 Hangman's fracture (list subtypes) ○ Odontoid fracture (list subtypes) • Subaxial cervical spine (C3-7) ○ Morphology • Compression • Burst • Distraction • Translational or rotational ○ Discoligamentous complex integrity • Anterior ligamentous complex (disk/anterior longitudinal ligament/posterior longitudinal ligament) • Posterior ligamentous complex (facet joint/ligamentum flavum/spinous ligaments) • Thoracolumbar spine ○ Morphology • Compression • Burst • Translational or rotational • Distraction ○ Discoligamentous complex integrity • Anterior ligamentous complex (disk/anterior longitudinal ligament/posterior longitudinal ligament) • Posterior ligamentous complex (facet joint/ligamentum flavum/spinous ligaments) • Sacrum (subtypes to be listed) and coccyx |
| Management | • Conservative ○ Without orthosis ○ Orthosis (list type) • Surgery ○ Timing to surgery ○ Surgical approach ○ Surgical level(s) ○ Procedure(s) • Decompression • Corpectomy/vertebrectomy • Discectomy • Instrumentation • Fusion • Osteotomy • Others ○ Devices • Cage (list type) • Screws (list type) • Wiring • Graft (list type) • Adjuncts (bone substitute/bone morphogenetic proteins/others) |
| Outcomes | • Physician reported ○ Imaging studies (list different modalities) ○ Outpatient review (neurological examination) • Patient reported ○ SF-12 ○ GOSE ○ Pain scores |
ASIA, American Spinal Injury Association; SF-12, Short-Form Health Survey; GOSE, Glasgow outcome score extended.
Pilot Study
A pilot study was performed to assess the feasibility of the minimum dataset in terms of data registration and data quality. In this study, 104 consecutive spine trauma patients admitted in the months of August and September 2010 to the Alfred Hospital were recruited by VOTOR.24 The methodology for VOTOR data collection is well established with all patients admitted to the participating hospitals (both the adult MTSs and the Geelong and Northern Hospitals) with an emergency admission of more than 24 hours for an orthopedic injury being eligible for inclusion in the registry.
Clinical data collection was performed by the first author (senior neurosurgery trainee) with patient data acquired from The Alfred's acute care electronic medical record (PowerChart, Cerner Solutions, Kansas City, MO, USA). The radiological aspect of clinical data collection was conjointly collected by the first and second authors (consultant neurosurgeon).
Outcomes 6-month postinjuries were assessed by administration of the SF-12 and GOSE by VOTOR personnel. The patients were also assessed by the Alfred Spine Service clinicians in the outpatient setting, with attention placed on their neurological status and fracture imaging review. The tabulated data were inserted into a computerized database and analyzed using the Statistical Package for the Social Sciences program (SPSS v19 Inc., Chicago, Illinois, United States).
Results
Minimum Dataset Feasibility
VOTOR patient recruitment for trauma patients with significant spine injuries necessitating admission of more than 24 hours in this study was 100%. There were eight patients without spinal fractures included in the initial patient shortlist. They were omitted from further analysis. Ease of data collection and entry without compromise of data quality was evident in our pilot study. The average time taken for clinical data entry per patient was approximately 5 minutes, with the aid of our dataset dictionary.
General Cohort
In our pilot study of 104 patients, three peaks were identified in the bar chart depicting the age distribution. These peaks corresponded to 16 to 25 years, 46 to 55 years, and more than 75 years age groups, representing 54% of our patients (Fig. 1). There was a higher rate of injury in males (65%) when compared with females (35%).
Figure 1.
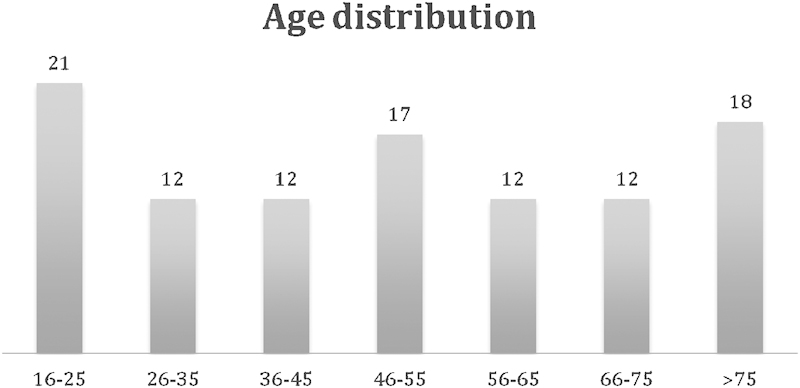
General cohort age distribution (in years).
Motor vehicle-related incidents (48%) and falls (40%) were the major injury mechanisms. A further 5% of the patients were injured while pursuing recreational activities with 7% forming the “other mechanisms” group. Of the 104 patients, 62% of the patients did not have any medical comorbidity nor were they taking any antiplatelet or anticoagulant agents. Approximately, one-fifth of the patients (21%) were on antiplatelet or anticoagulant agents and one-third (32%) of the patients had multiple medical comorbidities. In our study cohort, the large majority had good function; 94% of the patients were independent in their activities of daily living (ADL), 99% of them were mobile without the need of assistance, and 97% of them had normal cognition.
A total of 141 traumatic spinal fractures were reported in this group of 104 multitrauma patients. The thoracolumbar segment was the most frequent site injury (53%), followed by the subaxial cervical region (31%), and the sacrococcygeal and upper cervical region (C0-C2) (Fig. 2).
Figure 2.
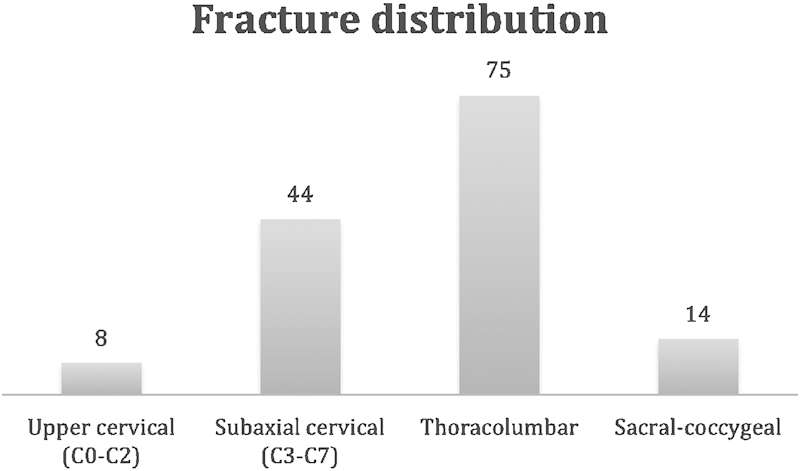
General cohort fracture distribution (total).
The majority of these patients presented neurologically intact (89%). Ten patients (10%) presented with varying degrees of incomplete neurological deficit on admission and one patient (1%) presented with complete neurological deficit and a T5 sensory level. Out of the 10 neurologically compromised patients, there were 5 patients with central cord syndrome. These patients usually have a degree of degenerative central canal stenosis with no acute traumatic bony or discoligamentous injury. These patients were managed conservatively. They were reviewed in the outpatient setting with a follow-up magnetic resonance imaging to assess neurological improvement and the need for decompression.
High Cervical Spine (Occipital Condyle or C0 to C2) Traumatic Injuries
There were eight patients with high cervical spine injuries. This constituted 6% of spine injuries and the least frequent site of injury. There were two occipital condyle fractures, one Jefferson's type fracture (C1), two Hangman's fracture (C2), one C2 body fracture, and two odontoid fractures (C2). There were no neurological deficits associated with these fractures. The majority of these patients (75%) were managed with a halo vest with only two patients (25%) managed in a rigid collar.
Subaxial Cervical Spine (C3-7) Traumatic Injuries
There were a total of 44 subaxial cervical spine injuries including 33 (75%) fractures. Out of the 33 reported fractures, the majority (79%) were compression type fractures. Distraction and rotation/translation type fractures were next with 9%, respectively, and burst fractures were the least common fracture type with 3%. Out of the 44 subaxial cervical spine injuries, 21 (48%) had radiological evidence of discoligamentous complex injuries.
Subaxial cervical spine injuries were managed surgically in 7 (16%) cases, and nonoperatively, with rigid orthoses in 35 (80%) cases. Only two (4%) fractures were managed without an orthosis as they had mild ligamentous injuries with no instability demonstrated on dynamic cervical plain radiographs.
Thoracolumbar Spine Traumatic Injuries
There were a total of 75 thoracolumbar spine injuries all including a fracture. Of these fractures, the majority (75%) were compression type fractures, followed by burst fractures (14%). Distraction type fractures were third (8%) and rotation/translation type fractures least common (3%). There was radiology evidence of discoligamentous complex injuries in 16 cases.
Thoracolumbar spine injuries were managed surgically in seven cases (9%). A total of 68 cases (91%) were managed in a nonoperative manner with fitting of a rigid orthosis occurring in 28 cases (38%). Fractures were managed without an orthosis in 40 cases (53%) as they had mild compression injuries and/or mild ligamentous injuries, with no instability shown on dynamic thoracolumbar plain radiographs.
Sacrococcygeal Traumatic Spine Injuries
There were a total of 14 sacrococcygeal spine injuries, representing 10% of the total spine injuries by segment. There were 10 Denis type 1 fractures and two Denis type 2 fractures. There were two coccygeal fractures. There were no neurological deficits associated with these fractures. All of these injuries were managed conservatively.
Outcomes: Physician-Reported Outcomes
Successful follow-up of physician-reported outcomes occurred in 91 patients (87.5%). Of these, 88 patients (97%) had satisfactory physician-reported outcomes with spine imaging studies demonstrating no evidence of spinal instability. Only three patients had surgery as a secondary procedure. One patient suffered an infection at his operative site requiring a washout procedure and cervical fracture stabilization revision surgery. Another patient had evidence of progressive neurological deficits (myelopathic signs) at his 4-week outpatient clinic review following conservative management of his central cord syndrome. He had an uncomplicated C3/4 anterior cervical discectomy and fusion (ACDF). The final patient had radiographic evidence of fracture instability at the 2-week outpatient clinic review while remaining neurologically intact and well. She initially had her C4/5 right-sided facet fracture treated with a rigid collar and underwent an uncomplicated C4/5 ACDF.
Outcomes: Patient-Reported Outcomes
VOTOR reports all patients who survived to hospital discharge using functional, health status, and pain measures, and provided the pilot study with 6-month postinjury data for reporting. Successful follow-up of patient-reported outcomes occurred in 95 patients (91%).
The functional outcomes of our patient cohort were assessed using the GOSE. A GOSE score of 5 or more was present in 79% with 21% having a GOSE score of 4 and less at the 6-month follow-up.
The health status of our patient cohort was measured at 6 months using the physical health summary score of the SF-12. The majority of spinal trauma cases (75%) reported physical health scores (PCS-12) below the general Australian population norm.
The mental health of our patient cohort was measured at 6 months using the mental health summary score of the SF-12. The majority of spinal trauma cases (60%) reported mental health scores (MCS-12) above the general Australian population norm.
The eighth question in the SF-12 (Fig. 3) was used to assess the level of pain experienced by our patient cohort at 6-month postinjury. Most patients (67%) had satisfactory pain control enabling commencement of normal daily activities, 17% had moderate activity restriction, and 16% were significantly prevented from satisfactorily performing their normal activities.
Figure 3.
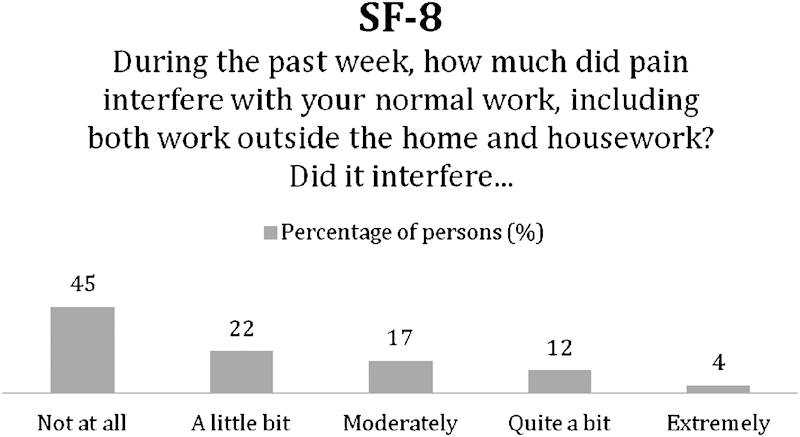
The eighth question in the SF-12 survey (evaluating pain tolerance and interference with daily activities).
Discussion
Findings
This study has demonstrated that it is feasible to collect accurate, reproducible, and clinically relevant data on spine trauma with marginal additional cost. Prospectively collected observational data are the most practical way to resolve spine trauma management controversies. Importantly, long patient enrollment periods to recruit adequate numbers may make the conclusions irrelevant by the time of trial completion. With a spine trauma registry, we should be able to define the current epidemiology of spine trauma and inform the development of spine trauma injury prevention strategies. We should also be able to monitor present spine trauma management and outcomes. By establishing the clinical outcomes of spine trauma patients, we will improve service planning and develop best practice clinical guidelines and initiatives. Benchmarking performance indicators on a national and international level is the ultimate goal, as it will push healthcare providers to be proactive and committed in the long term to improve program planning and policy development.
The majority of our epidemiological findings concurred with current literature with motor vehicle crashes and falls being the main causes of spinal trauma.3 4 16 30 We also found the thoracolumbar level as the most common fracture site and a low incidence of traumatic spinal cord injury when compared with spinal column trauma.2 3 4 Of interest however is our finding in our patient cohort of 104 patients, of three peaks in the age distribution. These peaks corresponded to 16 to 25 years, 46 to 55 years, and more than 75 years age groups, altogether representing 54% of our patients. Spinal trauma has been generally reported as having a bimodal peak with one in the early 1920s and another in the elderly population21 or a gradual decline from a peak in early adulthood.4 30 Our finding of a peak in the 46 to 55 years age group is especially significant as this age group represent the major breadwinners and main income earners of families and the society. We also found that 90% of the patients were fully independent and close to 80% having no medical comorbidities. Again, this shows the value of targeting general preventive services and health promotion toward this subgroup of spinal trauma patients. 20% of the patient cohort was on either an antiplatelet agent or an anticoagulant. It is likely that a large proportion of these patients are on these medications for cardiac disease or ischemic cerebrovascular disease prophylaxis. This increases the complexity of treatment in these patients, especially in those with incomplete neurological deficits and requiring urgent spinal surgical decompression and stabilization.
Health-related quality of life is an important outcome measure of any treatment. In recent times, trends of outcome reporting have incorporated patient-reported outcomes to supplement physician-reported outcomes. Patient-reported outcome data are key elements in resolution of spine trauma controversies such as the management of type 2 odontoid fractures in the elderly, thoracolumbar burst fractures, and traumatic central cord syndromes without evidence of acute bony or discoligamentous injury. It is likely that registry-methodology-type data would negate the controversy of performing a clinical trial if the perception of treatment leading to poor outcome is overwhelming (e.g., halo treatment in the elderly group for upper cervical spine injuries).
Physician-reported outcomes were determined during the follow-up clinic review. Patients reported satisfactory progress both in terms of fracture stability and healing as measured by dynamic imaging and on physical examination in 97% of cases. Three patients with subaxial cervical spine injuries required surgery as a secondary procedure. One patient suffered an infectious complication postsurgery while the other two patients failed conservative management. All three patients had their complications identified promptly with all of them recovering satisfactorily.
Our patient cohort had 91% 6-month patient-reported outcome follow-up rate (SF-12 and GOSE). The health status of our patient cohort showed that the majority of our spinal trauma cases had physical composite scores (PCS) below the general population norm, which is consistent with other subgroups of major trauma, including spinal cord injury cases.31 However, the median mental composite scores (MCS) of our patient cohort were higher than the general population norm. This is consistent with the spinal cord injury cohort in Victoria but not with other subgroups of major trauma.31 It is uncertain why this is so and we acknowledge that this result could be spurious due to the small numbers. Another finding was that our patient cohort had satisfactory pain control with only 16% complaining of pain significantly affecting their normal activities.
The GOSE was used to assess our patient cohort in terms of independence. A GOSE score of 5 or above indicates that a patient is living independently. In our patient cohort, 79% of our patients had a GOSE score of 5 or more at the 6-month follow-up. This is a favorable outcome relative to other major trauma patients. We acknowledge that our spinal patients may have polytrauma, and this may affect the outcome reporting of our patient cohort by biasing them toward a poorer outcome if compared with those with isolated spine injuries. A larger cohort will be necessary to explore the effects of various injury patterns on outcomes. It should be emphasized that this is a pilot study for minimum dataset feasibility, explaining the relatively short period of data collection.
The spine trauma literature is lacking general postdischarge physician- and patient-reported outcomes. There is however, literature with outcome reporting looking at spine column level specific management techniques. The general outcome of spinal trauma patients in terms of physician-reported outcomes and patient-reported outcomes are essential data required to ensure the safety and efficiency of a spine trauma service. Such data can also be used as performance indicators for benchmarking purposes however high follow-up rates are necessary. The pilot demonstrated satisfactory follow-up rates.
Strengths and Limitations
Analysis of trauma records showed that there were five spine trauma patients who failed VOTOR capture. One patient was transferred out within 12 hours of admission (and therefore did not qualify for VOTOR enrollment), to the Austin Hospital while four others died in hospital. The patient transferred out had an isolated spinal cord injury (central cord syndrome). The four deaths were multitrauma in nature with only minor spine injuries. The mortality subgroup may be excluded from the registry as no postdischarge outcome data can be derived. Our spine trauma registry proper will aim to capture all spine trauma patients presenting or transferred to the Alfred Hospital to ensure complete capture. This will include those that are outside of the VOTOR recruitment criteria and are those whose length of stay is less than 24 hours.
An important limitation of the pilot study was the reliability of data entry in terms of spine trauma imaging interpretation. We found that the dataset dictionary assisted us during the radiological interpretation of our patient cohort. Most, if not all studies to date performed by the spine trauma study group based in North America and other pioneers in spine trauma have involved mainly spine surgeons and not radiologists. We plan to improve on observer reliability and accuracy by utilizing synoptic reporting for spine trauma.32 Synoptic reporting is a method of template reporting and of structured data capture. It uses discrete and scientifically validated data elements, a set of universally required findings and provides a consistent report structure. This method of data capture and reporting has been used to great effect in oncological histopathology reporting.33 34
We acknowledge that the longevity and success of a clinical quality spine trauma registry is dependent on the involvement, enthusiasm, and skill of individual clinicians. The minimum dataset was created with this concern in mind. Ease of data collection and data entry is paramount in the prevention of registration fatigue. It is difficult to have a minimum number of data items and simultaneously preserve the quality of the spine trauma registry. Our premise for the minimum dataset was to allow prospective data collection and plan for future data extraction for the purpose of spine trauma clinical studies. For instance, the spine injury characteristic data items were selected based on current management guidelines. Descriptions of high cervical spine (C0-C2) injuries are exhaustive as current management treatment algorithms for this spinal region is injury-type specific.35 36 37 38 39 It is the converse for the subaxial cervical and thoracolumbar spine, which are based on the Subaxial Cervical Spine Injury Classification System (SLIC) and the Thoracolumbar Injury Classification and Severity Score (TLICS). They are at present, the most current and complete spine trauma treatment algorithms. They not only incorporate injury morphology and soft-tissue complex (discoligamentous structures) integrity but also consider the neurological status of the patient. The SLIC and TLICS have also relatively higher observer reliability and construct validity,40 41 which sets them apart from previous spine trauma classifications and algorithms.
Future Directions
The refined data collection methodology consists of the initial data collection being performed by the spine service registrar using a spine trauma assessment chart collecting history, clinical examination, and spine injury characteristics components of the minimum dataset. This data will be verified and entered into the registry database by the clinical nurse specialist. The clinical nurse specialist will also review individual spine trauma patient files for data on the definitive spine management and physician-reported outcomes.
VOTOR is a unique Victorian resource, which also has established infrastructure for collection of patient-reported outcomes.24 The registry's clinical nurse specialist will continue to liaise with VOTOR to acquire the SF-12, GOSE, pain, and other collected functional scores.
This article has demonstrated the likely benefits from collection of clinically relevant information in a spine trauma registry. We acknowledge that our pilot was facilitated by an existing data collection infrastructure. A region without robust data collection systems would require significant financial investments to research and develop such an entity. This investment is likely to be small when compared with the potential benefits of improving the fiscal and societal burden of spine trauma.
Conclusion
Spinal column injuries are common and under-researched and there is a paucity of knowledge regarding epidemiology and optimal management. There is a need for an all-inclusive spine trauma registry collecting both spine column and spinal cord injury data to inform management and future prevention strategies for spine trauma patients. This pilot study has shown the minimum dataset to be useful and data collection feasible. This pilot study demonstrates the practicality of a spine trauma registry at the Level 1 trauma center, where the majority of significant acute spinal injury is managed.
Acknowledgment
We would like to thank the VOTOR for assistance in data collection and analysis for this pilot project.
Disclosure, Competing Interests, and Ethics
There have been no competing interests or funding received for this article. Full ethics approval has been received for the published work.
Disclosures
Jin Tee, None
Patrick Chan, None
Russel Gruen, None
Mark Fitzgerald, None
Sue Liew, None
Peter Cameron, None
Jeffrey Rosenfeld, None
References
- 1.Fisher C G Noonan V K Dvorak M F Changing face of spine trauma care in North America Spine 20063111, SupplS2–S8., discussion S36 [DOI] [PubMed] [Google Scholar]
- 2.Hasler R M, Exadaktylos A K, Bouamra O. et al. Epidemiology and predictors of spinal injury in adult major trauma patients: European cohort study. Eur Spine J. 2011;20(12):2174–2180. doi: 10.1007/s00586-011-1866-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hu R, Mustard C A, Burns C. Epidemiology of incident spinal fracture in a complete population. Spine. 1996;21(4):492–499. doi: 10.1097/00007632-199602150-00016. [DOI] [PubMed] [Google Scholar]
- 4.Lenehan B, Boran S, Street J, Higgins T, McCormack D, Poynton A R. Demographics of acute admissions to a National Spinal Injuries Unit. Eur Spine J. 2009;18(7):938–942. doi: 10.1007/s00586-009-0923-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Access Economics Pty Limited The economic cost of spinal cord injury and traumatic brain injury in Australia. The Victorian Neurotrauma Initiative Available at: www.tac.vic.gov.au/upload/vni. Accessed June 2009 [Google Scholar]
- 6.van der Roer N, de Bruyne M C, Bakker F C, van Tulder M W, Boers M. Direct medical costs of traumatic thoracolumbar spine fractures. Acta Orthop. 2005;76(5):662–666. doi: 10.1080/17453670510041745. [DOI] [PubMed] [Google Scholar]
- 7.Aebi M, Grob D. SSE Spine Tango: a European Spine Registry promoted by the Spine Society of Europe (SSE) Eur Spine J. 2004;13(8):661–662. doi: 10.1007/s00586-004-0868-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Becker B E, DeLisa J A. Model Spinal Cord Injury System trends, and implications for the future. Arch Phys Med Rehabil. 1999;80(11):1514–1521. doi: 10.1016/s0003-9993(99)90266-6. [DOI] [PubMed] [Google Scholar]
- 9.DeVivo M J, Go B K, Jackson A B. Overview of the national spinal cord injury statistical center database. J Spinal Cord Med. 2002;25(4):335–338. doi: 10.1080/10790268.2002.11753637. [DOI] [PubMed] [Google Scholar]
- 10.Dimar J R, Fisher C, Vaccaro A R. et al. Predictors of complications after spinal stabilization of thoracolumbar spine injuries. J Trauma. 2010;69(6):1497–1500. doi: 10.1097/TA.0b013e3181cc853b. [DOI] [PubMed] [Google Scholar]
- 11.Ditunno J F Jr, Apple D F, Burns A S. et al. A view of the future Model Spinal Cord Injury System through the prism of past achievements and current challenges. J Spinal Cord Med. 2003;26(2):110–115. doi: 10.1080/10790268.2003.11753668. [DOI] [PubMed] [Google Scholar]
- 12.Dryden D M, Saunders L D, Rowe B H. et al. The epidemiology of traumatic spinal cord injury in Alberta, Canada. Can J Neurol Sci. 2003;30(2):113–121. doi: 10.1017/s0317167100053373. [DOI] [PubMed] [Google Scholar]
- 13.Hebert J S, Burnham R S. The effect of polytrauma in persons with traumatic spine injury. A prospective database of spine fractures. Spine. 2000;25(1):55–60. doi: 10.1097/00007632-200001010-00011. [DOI] [PubMed] [Google Scholar]
- 14.Johnson R L, Gabella B A, Gerhart K A, McCray J, Menconi J C, Whiteneck G G. Evaluating sources of traumatic spinal cord injury surveillance data in Colorado. Am J Epidemiol. 1997;146(3):266–272. doi: 10.1093/oxfordjournals.aje.a009262. [DOI] [PubMed] [Google Scholar]
- 15.Kattail D, Furlan J C, Fehlings M G. Epidemiology and clinical outcomes of acute spine trauma and spinal cord injury: experience from a specialized spine trauma center in Canada in comparison with a large national registry. J Trauma. 2009;67(5):936–943. doi: 10.1097/TA.0b013e3181a8b431. [DOI] [PubMed] [Google Scholar]
- 16.O'Connor P J. Development and utilisation of the Australian spinal cord injury register. Spinal Cord. 2000;38(10):597–603. doi: 10.1038/sj.sc.3101048. [DOI] [PubMed] [Google Scholar]
- 17.Roche S J, Sloane P A, McCabe J P. Epidemiology of spine trauma in an Irish regional trauma unit: a 4-year study. Injury. 2008;39(4):436–442. doi: 10.1016/j.injury.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 18.Tator C H, Carson J D, Edmonds V E. Spinal injuries in ice hockey. Clin Sports Med. 1998;17(1):183–194. doi: 10.1016/s0278-5919(05)70072-7. [DOI] [PubMed] [Google Scholar]
- 19.Torg J S, Guille J T, Jaffe S. Injuries to the cervical spine in American football players. J Bone Joint Surg Am. 2002;84-A(1):112–122. doi: 10.2106/00004623-200201000-00017. [DOI] [PubMed] [Google Scholar]
- 20.Utku S, Baysal H, Zileli M. Spine surgery database: a Turkish registry for spinal disorders. Turk Neurosurg. 2010;20(2):223–230. doi: 10.5137/1019-5149.JTN.2538-09.1. [DOI] [PubMed] [Google Scholar]
- 21.Bradley C, Harrison J. Adelaide: Australian Institute of Health and Welfare; 2004. Descriptive Epidemiology of Traumatic Fractures in Australia. Injury Research and Statistics Series Number 17 (AIHW cat. no. INJCAT 57) [Google Scholar]
- 22.Drolet B C, Johnson K B. Categorizing the world of registries. J Biomed Inform. 2008;41(6):1009–1020. doi: 10.1016/j.jbi.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 23.Urquhart D M, Williamson O D, Gabbe B J. et al. Outcomes of patients with orthopaedic trauma admitted to Level One Trauma Centres. ANZ J Surg . 2006;76(7):600–606. doi: 10.1111/j.1445-2197.2006.03785.x. [DOI] [PubMed] [Google Scholar]
- 24.Victorian Orthopaedic Trauma Outcomes Registry (VOTOR) . Epidemiology and preventative medicine. Medicine, nursing and health sciences. Monash University. http://www.med.monash.edu.au/epidemiology/traumaepi/orthoreg.html http://www.med.monash.edu.au/epidemiology/traumaepi/orthoreg.html
- 25.Victorian State Trauma System (VSTS). Victorian Government Health Information. State Government of Victoria, Department of Health. October 31, 2010. http://www.health.vic.gov.au/trauma/about.htm http://www.health.vic.gov.au/trauma/about.htm
- 26.Jackson G, Babbel R, Papastamopoulos D. Melbourne: Trauma System Co-ordination Unit, Service Development Branch, Department of Human Services; 2001. Major Trauma Data Review: Modelling the Impact of the Trauma Triage Guidelines. [Google Scholar]
- 27.Custer R L, Scarcella J A, Stewart B R. The modified Delphi technique: a rotational modification. Journal of Vocational and Technical Education. 1999;15(2):1–10. [Google Scholar]
- 28.Ware J E Jr, Kosinski M, Keller S D. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Wilson J T, Pettigrew L E, Teasdale G M. Structured interviews for the Glasgow Outcome Scale and the extended Glasgow Outcome Scale: guidelines for their use. J Neurotrauma. 1998;15(8):573–585. doi: 10.1089/neu.1998.15.573. [DOI] [PubMed] [Google Scholar]
- 30.Pirouzmand F. Epidemiological trends of spine and spinal cord injuries in the largest Canadian adult trauma center from 1986 to 2006. J Neurosurg Spine. 2010;12(2):131–140. doi: 10.3171/2009.9.SPINE0943. [DOI] [PubMed] [Google Scholar]
- 31.Victorian State Trauma Outcome Registry and Montoring Group (VSTORM) . Special Focus Report on Spinal Cord Injury (SCI) 2001–2008. Department of Health, State Government of Victoria, Australia. http://www.health.vic.gov.au/trauma/publications/vstorm-sci.pdf http://www.health.vic.gov.au/trauma/publications/vstorm-sci.pdf
- 32.Tee J W, Chan P C, Gruen R L, Rosenfeld J V. Synoptic reporting for spine trauma. Spine. 2011;36(23):1997. doi: 10.1097/BRS.0b013e3182333089. [DOI] [PubMed] [Google Scholar]
- 33.Gill A J, Johns A L, Eckstein R. et al. Synoptic reporting improves histopathological assessment of pancreatic resection specimens. Pathology. 2009;41(2):161–167. doi: 10.1080/00313020802337329. [DOI] [PubMed] [Google Scholar]
- 34.Srigley J R, McGowan T, Maclean A. et al. Standardized synoptic cancer pathology reporting: a population-based approach. J Surg Oncol. 2009;99(8):517–524. doi: 10.1002/jso.21282. [DOI] [PubMed] [Google Scholar]
- 35.AANS . Diagnosis and management of traumatic atlanto-occipital dislocation injuries. Neurosurgery. 2002;50(3, Suppl):S105–S113. doi: 10.1097/00006123-200203001-00018. [DOI] [PubMed] [Google Scholar]
- 36.AANS . Occipital condyle fractures. Neurosurgery. 2002;50(3, Suppl):S114–S119. doi: 10.1097/00006123-200203001-00019. [DOI] [PubMed] [Google Scholar]
- 37.AANS . Isolated fractures of the atlas in adults. Neurosurgery. 2002;50(3, Suppl):S120–S124. doi: 10.1097/00006123-200203001-00020. [DOI] [PubMed] [Google Scholar]
- 38.AANS. Isolated fractures of the axis in adults Neurosurgery 2002503, SupplS125–S139. [DOI] [PubMed] [Google Scholar]
- 39.AANS. Management of combination fractures of the atlas and axis in adults Neurosurgery 2002503, SupplS140–S147. [DOI] [PubMed] [Google Scholar]
- 40.Vaccaro A R, Lehman R A Jr, Hurlbert R J. et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine. 2005;30(20):2325–2333. doi: 10.1097/01.brs.0000182986.43345.cb. [DOI] [PubMed] [Google Scholar]
- 41.Vaccaro A R, Hulbert R J, Patel A A. et al. Spine Trauma Study Group . The subaxial cervical spine injury classification system: a novel approach to recognize the importance of morphology, neurology, and integrity of the disco-ligamentous complex. Spine. 2007;32(21):2365–2374. doi: 10.1097/BRS.0b013e3181557b92. [DOI] [PubMed] [Google Scholar]


