Abstract
Background and Aim: The classification of weight gain during pregnancy and the somatic classification of neonates according to birth weight and duration of pregnancy can be done using percentile values. We aimed to compare such classifications using percentiles of the overall study population with classifications using percentiles that were calculated taking account of maternal height and weight. Material and Methods: Using data from the German Perinatal Survey (1995–2000, over 2.2 million singleton pregnancies) we classified weight gain during pregnancy as low (< 10th percentile), high (> 90th percentile), or medium (10th–90th percentile). Neonates were classified by birth weight as small for gestational age (SGA, < 10th percentile), large for gestational age (LGA, > 90th percentile), or appropriate for gestational age (AGA, 10th–90th percentile). Classifications were performed for 12 groups of women and their neonates formed according to maternal height and weight, either with the percentiles calculated from the total study population or with group-specific percentiles. Results: Using percentiles of the total study population there was large variability between the 12 groups in the proportions with low and high weight gain and in the proportions of SGA and LGA neonates. The variability was much lower when group-specific percentiles were used. Conclusions: Classifications of maternal weight gain during pregnancy and birth weight differ substantially, depending on whether percentiles calculated from the total study population or group-specific percentiles are used. The impact of using percentiles that take account of maternal anthropometric parameters for the medical care and health of neonates needs to be elucidated in future research.
Key words: epidemiology, pregnancy, growth retardation
Abstract
Zusammenfassung
Hintergrund und Fragestellung: Die Klassifikation der Gewichtszunahme während der Schwangerschaft und die somatische Klassifikation der Neugeborenen nach Geburtsgewicht und Schwangerschaftsdauer können mit Perzentilwerten durchgeführt werden. Unser Ziel war, solche Klassifikationen basierend auf Perzentilen der gesamten Studienpopulation mit Klassifikationen basierend auf Perzentilwerten, die mütterliche Größe und Gewicht berücksichtigen, zu vergleichen. Material und Methodik: Anhand von Daten der Deutschen Perinatalerhebung (1995–2000, über 2,2 Mio. Einlingsschwangerschaften) klassifizierten wir die Gewichtszunahme während der Schwangerschaft als gering (< 10. Perzentile), groß (> 90. Perzentile) oder mittel (10.–90. Perzentile). Die Neugeborenen wurden nach dem Geburtsgewicht als „small for gestational age“ (SGA, < 10. Perzentile), „large for gestational age“ (LGA, > 90. Perzentile) oder „appropriate for gestational age“ (AGA, 10.–90. Perzentile) klassifiziert. Diese Klassifikationen wurden für 12 Gruppen von Frauen und deren Neugeborenen, die aufgrund von mütterlicher Körpergröße und -gewicht gebildet wurden, durchgeführt, entweder mit den Perzentilen der gesamten Studienpopulation oder mit gruppenspezifischen Perzentilen. Ergebnisse: Bei Gebrauch von Perzentilen der gesamten Studienpopulation ergab sich zwischen den 12 Gruppen eine große Variabilität in den Anteilen mit geringer und großer Gewichtszunahme und in den Anteilen von SGA- und LGA-Neugeborenen. Bei Gebrauch gruppenspezifischer Perzentilen war diese Variabilität deutlich kleiner. Schlussfolgerungen: Die Klassifikationen der Gewichtszunahme während der Schwangerschaft und des Geburtsgewichts unterscheiden sich deutlich, je nachdem, ob Perzentilen der gesamten Studienpopulation oder gruppenspezifische Perzentilen verwendet werden. Die Auswirkungen des Gebrauchs von Perzentilen, welche die mütterlichen Körpermaße berücksichtigen, auf die medizinische Versorgung und Gesundheit der Neugeborenen müssen noch untersucht werden.
Schlüsselwörter: Epidemiologie, Schwangerschaft, Wachstumsretardierung
Introduction
The weight gain of women during pregnancy is a key perinatal parameter; it is easily measured and there is now a wealth of evidence showing that weight gain has an impact on a number of important maternal and neonatal outcomes, including the preterm birth rate and the duration of pregnancy 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, the birth weight 7, 8, 9, 10, 11, 12, 13, 15, 16, 17, 18, 19, 20, and the somatic classification of neonates 7, 8, 9, 15, 21, 22, 23, 24. For this somatic classification neonates are typically classified using the 10th and 90th birth weight percentiles, calculated according to gestational age; neonates below the 10th birth weight percentile are “small for gestational age” (SGA), those above the 90th birth weight percentile are “large for gestational age” (LGA), and all those in-between are “appropriate for gestational age” (AGA).
We previously investigated weight gain in pregnancy in relation to maternal anthropometric measurements, finding an increase in the weight gained during pregnancy with increasing maternal height and, for women weighing more than about 63 kg at the first obstetric consultation (for the pregnancy in question), an inverse relationship between maternal weight at the first consultation and the weight gained during pregnancy 25. Maternal anthropometric measurements of course also influence neonatal anthropometric measurements and therefore the somatic classification of neonates, when this is performed using percentiles of the total study population 26, 27.
The classification of weight gain during pregnancy and the somatic classification of neonates can therefore be expected to be more accurate when maternal body height and weight are taken into account, rather than when percentiles calculated from the total study population are used, irrespective of maternal anthropometric measurements. As body height and weight can be combined into a single measure such as the body mass index (BMI), the question arises whether the classification of maternal weight gain and the neonatal somatic classification should be undertaken according to maternal BMI, e.g. whether the ranges for weight gain should be specified for different BMI ranges. Indeed, the Institute of Medicine recommends assessing weight gain during pregnancy by maternal BMI 28. However, we have shown that both maternal weight gain 25 and the somatic classification of neonates 29 can differ substantially between women who have the same BMI but different body heights and weights.
An alternative approach, i.e. taking account of maternal anthropometric measurements by grouping women according to their height and weight, therefore deserves investigation. We previously presented norm values for weight gain during pregnancy for different maternal height and weight groups 30. In the present analysis, we investigate the classification of weight gain during pregnancy and the somatic classification of neonates: we compare classifications based on weight gain and birth weight percentiles that were calculated from the total study population with classifications based on percentiles that were calculated separately for the different maternal height and weight groups.
The question we wanted to answer was whether these classifications differ substantially, because if they do not, it would be hard to see any advantage of using classification systems that take maternal height and weight into account.
Material and Methods
The data on which this analysis is based were taken from the routine data collection of the German Perinatal Survey that is done throughout Germany. Data were kindly made available to Dr. Voigt by the Chambers of Physicians of the States of Germany. The data were collected in the years 1995 to 2000. For the years 1995–1997 all States of Germany except Baden-Württemberg provided data; thereafter only Bavaria, Brandenburg, Hamburg, Mecklenburg-Western Pomerania, Lower Saxony, Saxony, Saxony-Anhalt, and Thuringia provided data, not necessarily for all years. Overall, our database contains datasets from more than 2.2 million singleton pregnancies; this is our total study population. Because not all datasets were complete with regard to all maternal and neonatal parameters collected, the sample sizes vary between analyses. The figures presented in this paper and the supplemental online figures contain information on the case numbers included in individual analyses.
We calculated weight gain during pregnancy from the weights recorded at the first obstetric consultation and at the end of pregnancy; weight gain was classified using the 10th and 90th weight gain percentiles; “low weight gain” was defined as a weight gain below the 10th percentile, “high weight gain” as above the 90th percentile, and “medium weight gain” was between the 10th and 90th percentiles.
As described in the introduction, the neonatal somatic classification was based on birth weight percentiles specified according to gestational age, using the 10th and 90th percentiles; neonates with a birth weight below the 10th percentile were SGA, those with a birth weight greater than the 90th percentile were LGA, and those in-between were AGA.
The classification of weight gain during pregnancy and the somatic classification of neonates were done using either the 10th and 90th percentiles calculated from the total study population or the 10th and 90th percentiles calculated specifically for the groups of mothers and neonates compiled based on maternal height and weight. We compiled 12 such groups based on a division of maternal height into three groups (≤ 161 cm, 162–171 cm, ≥ 172 cm) and a division of maternal weight into four groups within the height groups, as described previously 30. In addition to presenting the classification of maternal weight gain during pregnancy and the somatic classification of neonates separately, we also show combined classifications: neonatal somatic classifications are presented separately for low, medium, and high weight gain.
The chi-squared test was used to establish the statistical significance of differences between neonatal somatic classifications of different maternal weight gain groups. Data analysis was performed using the computer programme SPSS (version 20) in the computing centre of the University of Rostock, Germany.
Results
Using percentile values for maternal weight gain and birth weight calculated from the total study population
In the printed version of this article we show data for women with a height ≤ 161 cm and their neonates. Similar findings were obtained for the other maternal height groups: 162–171 cm and ≥ 172 cm (see supplemental online figures). Fig. 1 and supplemental online Figs. 1S and 2S illustrate the classification of maternal weight gain during pregnancy and the neonatal somatic classification as well as the combination of these classification systems (neonatal somatic classifications presented separately for low, medium, and high weight gain, as described above) when the percentiles used for the classification of weight gain and the somatic classification of neonates (i.e. the 10th and 90th percentiles) were calculated from the total study population of women or neonates, respectively.
Fig. 1.
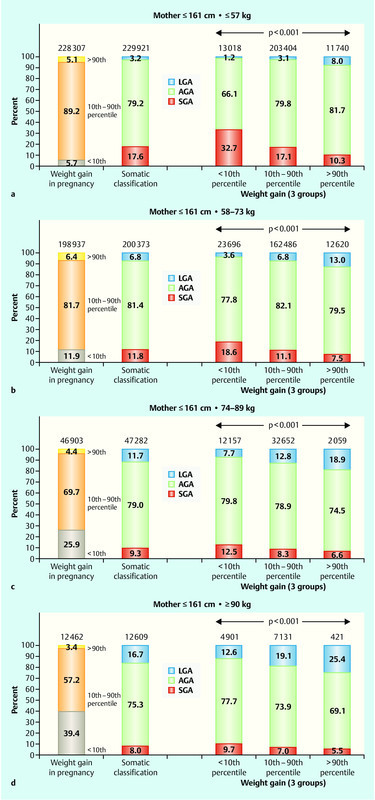
Classifications based on weight gain and birth weight percentiles calculated from the total study population for women with a height ≤ 161 cm and their neonates. The classification of maternal weight gain during pregnancy for women with a height ≤ 161 cm and a weight of ≤ 57 kg, 58–73 kg, 74–89 kg, or ≥ 90 kg (Figs. 1 a–d, respectively) and the somatic classification of infants born to them are shown in the two columns on the left of each figure. The right side of each figure shows a combination of the two: the somatic classification of neonates within the three weight gain groups (< 10th, 10–90th and > 90th weight gain percentile). Neonates were classified as small for gestational age (SGA, < 10th birth weight percentile), appropriate for gestational age (AGA, 10–90th birth weight percentile), or large for gestational age (LGA, > 90th weight gain percentile). Contributing case numbers are shown on top of the columns. The p-values were calculated using the chi-squared test.
Using percentile values for maternal weight gain and birth weight calculated separately for the 12 groups of women compiled according to height and weight
Fig. 2 and supplemental online Figs. 3S and 4S show the classification of maternal weight gain during pregnancy and the neonatal somatic classification as well as the combination of these classification systems (as above) but this time using group-specific percentiles for weight gain during pregnancy and also group-specific percentiles of birth weight for gestational age calculated separately for the 12 groups of women and their neonates formed according to maternal height and weight.
Fig. 2.
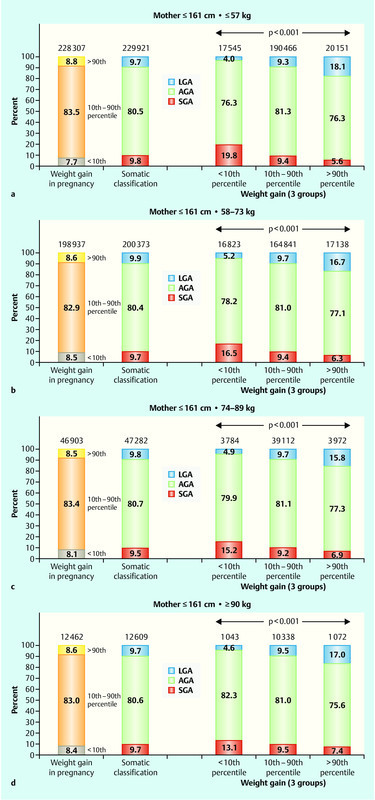
Classifications based on weight gain and birth weight percentiles calculated specifically for the maternal height and weight groups in question for women with a height ≤ 161 cm and their neonates. Details are analogous to the description in the legend to Fig. 1.
When percentiles based on the total study population were used, there was a large variability in the percentages of women with low and high weight gain and in the percentages of SGA and LGA neonates. When group-specific percentiles were used, this variability was much lower. For example, for percentiles calculated from the total study population the percentage of women with a low weight gain (below the 10th weight gain percentile) ranged between 5.7 and 39.4 % in women with a height ≤ 161 cm, depending on their weight group (Fig. 1). Using group-specific percentiles the variation was considerably lower and ranged between 7.7 and 8.5 % (Fig. 2).
The proportion of SGA neonates born to women with a height ≤ 161 cm varied between 8.0 and 17.6 %, depending on maternal weight, when percentiles calculated from the total study population were used for the somatic classification of neonates; when group-specific percentiles were used, the variation was between 9.5 and 9.8 %, again substantially lower. The same pattern was observed for the other maternal height and weight groups.
When the combined classifications of weight gain during pregnancy and birth weight for gestational age were examined, considerable differences were also found between classifications using percentiles calculated from the total study population and those using group-specific percentiles. When percentiles calculated from the total study population were used, there was considerable variability between maternal weight groups with regard to the influence of maternal weight gain on the somatic classification of neonates. Using group-specific percentiles there was less variability between the maternal weight groups in this regard.
Discussion
We were fortunate to have a large amount of data available which permitted reliable calculations of percentiles for weight gain during pregnancy and birth weight for gestational age even in sub-populations of our total study population, i.e. in the groups of women and neonates compiled according to maternal height and weight. Our key finding is that the classifications of maternal weight gain during pregnancy by weight gain percentiles and the somatic classifications of neonates as SGA, AGA, or LGA differ substantially depending on whether these classifications were done using percentiles calculated from the total study population or using group-specific percentiles calculated specifically for the groups of women and neonates compiled based on maternal height and weight. The impact of using classification systems that take account of maternal height and weight on the medical care and health of neonates still needs to be investigated and this remains a task for future research.
Limitations of our study include a degree of uncertainty with regard to the calculation of weight gain during pregnancy: weight at the first obstetric consultation depends on when the first consultation occurs and weight at the end of pregnancy varies depending on the length of gestation. Moreover, the grouping of women by maternal height and weight was arbitrary and different cut-off points and different numbers of groups would also have been possible.
Because the classification of neonates as small, appropriate, or large for gestational age may well have consequences for the care of these neonates and with regard to the use of resources, it is important to use as accurate a classification system as possible. A classification system that takes account of maternal anthropometric measurements should more accurately identify small or large neonates due to abnormal intrauterine growth as compared to constitutionally small or large neonates.
Acknowledgements
We would like to thank the Chambers of Physicians of the States of Germany for contributing data to our database. We also thank Christel Fernow for her help with preparing the figures.
Footnotes
Conflict of Interest None.
Supporting Information
References
- 1.Abrams B, Newman V, Key T. et al. Maternal weight gain and preterm delivery. Obstet Gynecol. 1989;74:577–583. [PubMed] [Google Scholar]
- 2.Carmichael S L, Abrams B. A critical review of the relationship between gestational weight gain and preterm delivery. Obstet Gynecol. 1997;89:865–873. doi: 10.1016/s0029-7844(97)00047-1. [DOI] [PubMed] [Google Scholar]
- 3.Schieve L A, Cogswell M E, Scanlon K S. Maternal weight gain and preterm delivery: differential effects by body mass index. Epidemiology. 1999;10:141–147. doi: 10.1097/00001648-199903000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Schieve L A, Cogswell M E, Scanlon K S. et al. The NMIHS Collaborative Study Group . Prepregnancy body mass index and pregnancy weight gain: associations with preterm delivery. Obstet Gynecol. 2000;96:194–200. doi: 10.1016/s0029-7844(00)00883-8. [DOI] [PubMed] [Google Scholar]
- 5.Dietz P M, Callaghan W M, Cogswell M E. et al. Combined effects of prepregnancy body mass index and weight gain during pregnancy on the risk of preterm delivery. Epidemiology. 2006;17:170–177. doi: 10.1097/01.ede.0000198470.26932.9a. [DOI] [PubMed] [Google Scholar]
- 6.Stotland N E, Caughey A B, Lahiff M. et al. Weight gain and spontaneous preterm birth: role of race and ethnicity and previous preterm birth. Obstet Gynecol. 2006;108:1448–1455. doi: 10.1097/01.AOG.0000247175.63481.5f. [DOI] [PubMed] [Google Scholar]
- 7.Sekiya N, Anai T, Matsubara M. et al. Maternal weight gain rate in the second trimester are associated with birth weight and length of gestation. Gynecol Obstet Invest. 2007;63:45–48. doi: 10.1159/000095286. [DOI] [PubMed] [Google Scholar]
- 8.Fox N S, Rebarber A, Roman A S. et al. Weight gain in twin pregnancies and adverse outcomes: examining the 2009 Institute of Medicine guidelines. Obstet Gynecol. 2010;116:100–106. doi: 10.1097/AOG.0b013e3181e24afc. [DOI] [PubMed] [Google Scholar]
- 9.Savitz D A, Stein C R, Siega-Riz A M. et al. Gestational weight gain and birth outcome in relation to prepregnancy body mass index and ethnicity. Ann Epidemiol. 2011;21:78–85. doi: 10.1016/j.annepidem.2010.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mamun A A, Callaway L K, OʼCallaghan M J. et al. Associations of maternal pre-pregnancy obesity and excess pregnancy weight gains with adverse pregnancy outcomes and length of hospital stay. BMC Pregnancy Childbirth. 2011;11:62. doi: 10.1186/1471-2393-11-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Han Z, Lutsiv O, Mulla S. et al. Knowledge Synthesis Group . Low gestational weight gain and the risk of preterm birth and low birthweight: a systematic review and meta-analyses. Acta Obstet Gynecol Scand. 2011;90:935–954. doi: 10.1111/j.1600-0412.2011.01185.x. [DOI] [PubMed] [Google Scholar]
- 12.McDonald S D, Han Z, Mulla S. et al. Knowledge Synthesis Group . High gestational weight gain and the risk of preterm birth and low birth weight: a systematic review and meta-analysis. J Obstet Gynaecol Can. 2011;33:1223–1233. doi: 10.1016/S1701-2163(16)35107-6. [DOI] [PubMed] [Google Scholar]
- 13.González-Quintero V H, Kathiresan A S, Tudela F J. et al. The association of gestational weight gain per institute of medicine guidelines and prepregnancy body mass index on outcomes of twin pregnancies. Am J Perinatol. 2012;29:435–440. doi: 10.1055/s-0032-1304824. [DOI] [PubMed] [Google Scholar]
- 14.Carnero A M, Mejía C R, García P J. Rate of gestational weight gain, pre-pregnancy body mass index and preterm birth subtypes: a retrospective cohort study from Peru. BJOG. 2012;119:924–935. doi: 10.1111/j.1471-0528.2012.03345.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mewitz M, Voigt M, Schild R L. et al. On weight gain during pregnancy: relationships between weight gain during pregnancy, duration of pregnancy and the somatic classification of neonates. Z Geburtshilfe Neonatol. 2012;216:22–26. doi: 10.1055/s-0031-1298028. [DOI] [PubMed] [Google Scholar]
- 16.Seidman D S, Ever-Hadani P, Gale R. The effect of maternal weight gain in pregnancy on birth weight. Obstet Gynecol. 1989;74:240–246. [PubMed] [Google Scholar]
- 17.Shapiro C, Sutija V G, Bush J. Effect of maternal weight gain on infant birth weight. J Perinat Med. 2000;28:428–431. doi: 10.1515/JPM.2000.056. [DOI] [PubMed] [Google Scholar]
- 18.Rode L, Hegaard H K, Kjaergaard H. et al. Association between maternal weight gain and birth weight. Obstet Gynecol. 2007;109:1309–1315. doi: 10.1097/01.AOG.0000266556.69952.de. [DOI] [PubMed] [Google Scholar]
- 19.Frederick I O, Williams M A, Sales A E. et al. Pre-pregnancy body mass index, gestational weight gain, and other maternal characteristics in relation to infant birth weight. Matern Child Health J. 2008;12:557–567. doi: 10.1007/s10995-007-0276-2. [DOI] [PubMed] [Google Scholar]
- 20.da Fonseca C R, Strufaldi M W, de Carvalho L R. et al. Risk factors for low birth weight in Botucatu city, SP state, Brazil: a study conducted in the public health system from 2004 to 2008. BMC Res Notes. 2012;5:60. doi: 10.1186/1756-0500-5-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nohr E A, Vaeth M, Baker J L. et al. Combined associations of prepregnancy body mass index and gestational weight gain with the outcome of pregnancy. Am J Clin Nutr. 2008;87:1750–1759. doi: 10.1093/ajcn/87.6.1750. [DOI] [PubMed] [Google Scholar]
- 22.Margerison Zilko C E, Rehkopf D, Abrams B. Association of maternal gestational weight gain with short- and long-term maternal and child health outcomes. Am J Obstet Gynecol. 2010;202:5740–5.74E10. doi: 10.1016/j.ajog.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 23.Deierlein A L, Siega-Riz A M, Adair L S. et al. Effects of pre-pregnancy body mass index and gestational weight gain on infant anthropometric outcomes. J Pediatr. 2011;158:211–216. doi: 10.1016/j.jpeds.2010.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krentz H, Voigt M, Hesse V. et al. Somatic classifications of neonates based on weight-for-length and Rohrerʼs ponderal index: effects of maternal BMI and smoking. Geburtsh Frauenheilk. 2011;71:973–978. [Google Scholar]
- 25.Voigt M, Straube S, Olbertz D. et al. Beziehungen zwischen Körpergewicht, Körperhöhe, Body-Mass-Index und der Gewichtszunahme von Frauen in der Schwangerschaft. Z Geburtshilfe Neonatol. 2007;211:147–152. doi: 10.1055/s-2007-981236. [DOI] [PubMed] [Google Scholar]
- 26.Voigt M, Rochow N, Jährig K. et al. Dependence of neonatal small and large for gestational age rates on maternal height and weight-an analysis of the German Perinatal Survey. J Perinat Med. 2010;38:425–430. doi: 10.1515/jpm.2010.059. [DOI] [PubMed] [Google Scholar]
- 27.Stein R G, Meinusch M, Diessner J. et al. Fruchtwasserinsulin und C-Peptid als prädiktive Marker für Makrosomie und Geburtskomplikationen? Geburtsh Frauenheilk. 2012:72–P39. [Google Scholar]
- 28.Rasmussen K M Yaktine A Leds.Committee to Reexamine IOM Pregnancy Weight Guidelines; Institute of Medicine; National Research Council Weight Gain during Pregnancy: reexamining the Guidelines Washington, DC: National Academies Press; 2009 [PubMed] [Google Scholar]
- 29.Krentz H, Voigt M, Guthmann F. et al. On the variability in preterm birth rate, birth weight, and somatic classification among neonates of mothers with the same body mass index. Z Geburtshilfe Neonatol. 2011;215:163–166. doi: 10.1055/s-0031-1285847. [DOI] [PubMed] [Google Scholar]
- 30.Voigt M, Straube S, Schmidt P. et al. Vorstellung von Normwerten der Gewichtszunahme in der Schwangerschaft (20–43 vollendete Schwangerschaftswochen) unter Berücksichtigung von Körperhöhe und Körpergewicht der Frauen. Z Geburtshilfe Neonatol. 2007;211:191–203. doi: 10.1055/s-2007-981327. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


